Introduction
Hand surgeons, as unique specialists, appreciate the complexity of the anatomy of the hand. A hand is not merely a group of anatomic structures but a separate organ that works by feeling, sending information to the brain, and enabling a variety of movements, from precise skills to firm tasks.
Treatment plans for injury, chronic disease, or post-traumatic conditions require adequate imaging and close cooperation with radiologists. Despite thorough clinical evaluation, there is a lack of precision in assessing nerve lesions, tendon function, and the extent of filamentous injuries. These problems may be solved using modern imaging modalities, including magnetic resonance (MR) arthrogram, computed tomography (CT) with threedimensional reconstruction, or dynamic ultrasonography.
In the era of teleradiology and online meetings, seve-ral questions can be raised, such as how the interaction and communication between surgeons and radiologists should be verified and what kind of answers should be considered clinically relevant. Many of these questions differ according to world region, health care system, and cultural specificity. Depending on local regulations, there are different cooperation models between surgeons and radiologists, from sending a request for radiologic assessment and receiving an evaluation to discussing and tailoring the review to the clinical needs and specificity.
Appropriate radiographic findings could be expected when asking proper questions based on history taking and clinical assessment. Clinical information is not always accessible to radiologists. Therefore, our clinical assessments should be precisely described along with initial diagnosis and elements of patient history that can assist in accurate radiological assessment. We also prefer phone contact in complex cases where surgeons or radiologists require an explanation. In many cases, results of previous radiographic studies are necessary to help diagnose. In health systems based on teleradiology (e.g. in the U.S., radiological images are assessed by radiologists in India), direct or phone contact can be impossible, leaving no place for discussion, which is often needed in extraordinary cases.
What answers should we expect? First are the answers to the clinical question, usually structured and anatomic, about how we assess and see our patients. Accidental findings should also be added after the final assessment of diagnosis but should be separated from major findings to avoid misunderstandings. The pathological findings should be emphasised, and biomechanical interpretation should be included, such as in the case of dynamic ultrasonography.
If possible, direct contact between surgeons and radiologists working together as a team would be beneficial; this is still possible in larger hospitals or departments. Otherwise, it is crucial to have access to experienced radiologists so that unusual and complex cases can be further discussed.
Bones and joints
Bone fracture represents one of the most common injuries where the surgeon must decide between operative and non-operative treatment [1]. While some fractures, such as those involving the distal radius, still lack consensus on the most appropriate treatment, others, such as scaphoid fractures, have definite modalities for diagnosis and indications for surgery. There are several points when making the diagnosis:
Confirmation of fracture, which can be crucial in carpal fractures, such as scaphoid fractures, where delayed treatment may produce severe complications, including pseudoarthrosis and degenerative changes [2,3].
Extra/intraarticular or complex phalangeal fractures especially those involving the proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) joint, and carpometacarpal (CMC) joint. These fractures are often associated with displaced articular fragments, rotational misalignment, and abnormal angulation and/or shortening. Very often, X-ray images in typical projections are not sufficient to make the correct treatment decision. To better visualise the fracture, a special form of computed tomography is increasingly used, such as cone-beam computed tomography (CBCT) technology. The advantages of CBCT include smaller set-ups, high spatial resolution, optimal reduction in metal artefacts, low radiation dose, and relatively low cost of the equipment compared to multi-slice computed tomography (MSCT) [4].
Confirmation of dislocation – plain radiographs could be misleading in perilunate or carpometacarpal joint dislocations, especially if physicians in the emergency room are less experienced (Figure 1).
Extra or intraarticular fracture – extraarticular fractures can usually be managed by non-operative modalities, except for severely displaced shaft fractures with disrupted axis [5].
Level of comminution that is specific to some regions – severely comminuted fractures are unstable and, when not reduced and fixed, can lead to pain, limited range of motion (ROM), and early arthritic changes.
Stability of joint (reduced/subluxated) – in joint instability, even if the fragment is small, such as in avulsion fracture, operative reduction and fixation are mandatory to achieve good function. This is a common situation in proximal interphalangeal joints when an avulsion fracture of the volar plate or fracture of the base of the middle phalanx can result in subluxation of the joint. This possibility is often underestimated, and the injury is treated by closed reduction, which may lead to recurrence despite adequate splinting [1].
Involvement of growth plate in children [6].
Quality of bone stock is important in planning the method of fixation and evaluating the possibility of bone grafting.
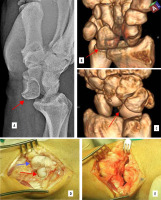
Figure 1
Neglected nonreduced lunate dislocation. A) Plain lateral radiogram (red arrow). B, C) 3D reconstruction. D) Blue arrow – scaphoid. E) After proximal row carpectomy joint is formed between the distal radius and capitate)
A second set of questions arises when dealing with fracture sequelae. One is delayed healing or nonunion, which is difficult to assess using standard radiographs and is not easily distinguishable at CT if it is in the early phase. In cases of scaphoid nonunion, it is desirable to estimate the bone loss, vascularity – mainly of the proximal pole, and peri-scaphoid degenerative changes. All these factors influence treatment decisions, from excision of nonunion and bone grafting to salvage procedures such as scaphoid resection or four-corner fusion. Each surgical technique has pros and cons that must be discussed with the patient before surgery [2,7].
The next set of problems arises with the more popular use of locking plates, especially in the distal radius. We frequently observe malpositioning of the screws, which influences or even destroys normal motion of joints such as the distal radioulnar joint (Figure 2) or causes inflammation leading to chronic rupture of the tendon, which is well depicted in Figure 3 by ultrasonography. These findings can be a reason for the removal of plates or screws, leading to unplanned secondary surgery. In cases of tendon rupture, such as in chronic injury of extensor pollicis longus, tendon transfer is often required for recovery of function [8].
Figure 2
Ulnar screw blocking and chronically damaging the distal radioulnar joint. A) Plain radiogram. B) CT scan showing protruding screw causing ulnar impingement and erosion – red arrow

Figure 3
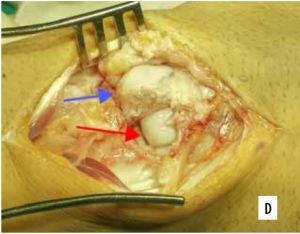
Volar plate screws conflict with extensors. A) Plain radiogram. B, C) CT scans showing screws between non-malreduced fragments (arrows). Sonographic (D) and intraoperative (E) presentation

The fourth group of cases are patients with chronic pain related to osteoarthritis. It can be primary or secondary, associated with trauma, instability, or inflammatory process such as rheumatoid arthritis (RA). We rely on plain radiographs in most situations. Still, detailed imaging of the joint surface using MRI is significant in conditions such as scapholunate advanced collapse (SLAC) or scaphoid nonunion advanced collapse (SNAC). In these conditions, surgical procedures are planned based on the status of the joint preservation from the disease. For instance, if the lunate fossa and capitate cartilage are spared, proximal row carpectomy is an acceptable choice in radiocarpal arthritis or lunate avascular necrosis cases [9-11].
In cases of RA, the disease pattern varies and differs from OA, and instability, subluxation, and massive degeneration are often seen in older patients treated with traditional RA medications. Despite the degeneration, the symptoms can be less severe, making the need for surgery difficult [12,13]. We pay much more attention to early changes of the degeneration or inflammatory process evaluated by MR or sonography to prevent future destruction [14]. Fortunately, this has become much easier with the introduction of biological treatment.
Ligaments
Most ligament problems are related to injuries (25% are sports-related). Thirty per cent of patients with wrist pain sustained an injury within the previous year. The structures that are most often repaired are the ulnar collateral ligament of the thumb, dorsoradial ligament or anterior oblique ligament of the trapeziometacarpal joint, scapholunate (SL) and lunotriquetral (LT) ligament, and triangular fibrocartilage complex (TFCC) of the wrist [11,15,16].
We can classify these clinical situations into 2 groups: acute and chronic. The former condition is usually assessed using primary imaging modalities such as plain radiographs or ultrasonography, which are adequate in decision-making for thumb lesions but are insufficient in wrist injuries. The question is how much information we need and whether it is accessible from the economic and organisational point of view in every wrist injury suspected of ligament tear. Currently, there is no consensus on the indication to perform MR arthrogram and what decision to make based on the MR result, namely, whether we should recommend surgery to patients with TFCC tear or SL ligament partial rupture having no radiological signs of instability (Figure 4). These issues are much more important for sports professionals where fast return to highly demanding activities is a matter of business [11,16,17].
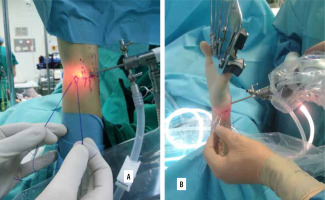
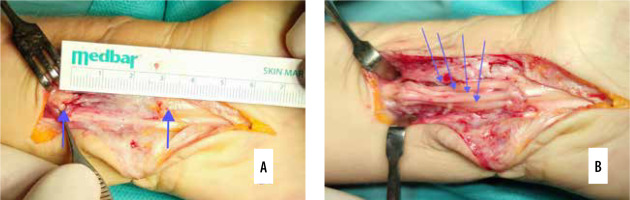
Figure 4
Arthroscopic capsular repair of ulnar triangular fibrocartilage complex attachment using inside-out technique. A) Scoping from 3-4 portal, sutures are pulled out on the ulnar side. B) Inside out technique of suture placement with needles
In usual practice, the following points should be addressed in the imaging examination:
Extent of injury – complete/partial, insertion avulsion/rupture, which can be applied to typical areas such as TFCC (superficial or deep layer in ulnar-sided lesions).
Type of injury – Sterner lesion with ligament migration, which disables primary healing and is a clear indication for surgical reinsertion (Figure 5A).
Joint stability assessed in stress X-rays or dynamic US.
Figure 5
Reinsertion of ulnar collateral ligament of the thumb with the usage of soft mini anchor. A) Anchor in the base of the proximal phalanx (blue arrow), torn ligament (red arrow), examples of soft (B) and titanium (C) implants
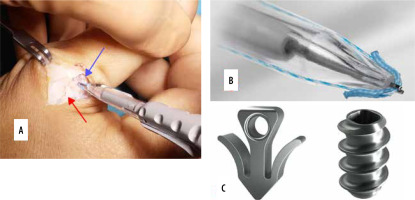
Clinical problems are always the most important [18]. If the remaining structures or part of the ligament is sufficient to keep the joint stable, the injury can usually be treated by non-surgical means. In other situations or if pain persists chronically, surgery could be considered, which includes reinsertion, local, or graft reconstruction [19]. When these techniques are planned, imaging studies should consider the type of implants or anchors used. These include metallic, non-metallic absorbable, or non-absorbable and present differently according to imaging modalities (Figures 5B and C). This knowledge is important when assessing the surgical results and planning revision surgeries.
Tendons and muscles
Intrinsic and extrinsic muscles of the hand and their complex function in every joint make diagnosis difficult [20]. Although acute injuries are usually not hard to assess by clinical examination, late presentation or chronic problems can be challenging. From the point of view of hand surgeons, the following aspects should generally be addressed:
Level of the lesion, which includes specific zones of flexors and extensors.
Type of lesion: cut, tear, or avulsion, and the specific points in flexor or extensor apparatus avulsion. In the flexor avulsion, tendon status and level of the retraction of the tendon are important in planning and surgical approach, especially in neglected cases.
Possible gap between tendon stumps when secondary treatment is required [21].
Accompanying damage of pulleys with resultant bowstringing that explains ROM insufficiency must be addressed during surgery of pulley reconstruction or sagittal band rupture in extensor cases producing tendon instability.
ECU tendon instability can be a part of the TFCC lesion or can be the only reason for pain [22].
For complex injuries that include many tendon/muscle units, anatomic reconstruction is impossible. Identifying the donor tendons is often problematic in proximally avulsed tendons or injuries of the musculotendinous junction – in these cases, other proximal donor tendons should be searched for reconstruction.
Tendon gliding in situations of insufficient function after tendon repair can be crucial in deciding on tenolysis surgery.
Accompanying injuries: nerves, fat tissue, skin according to Boyes score.
In these situations, ultrasonography will be helpful, enabling dynamic testing and assessment of the complete unit. All the above findings are necessary for planning the surgery and predicting the use of grafts (short zone I-III, long zone I-V), additional pulley reconstruction over silicone rod (Figure 6), or nerve reconstruction.
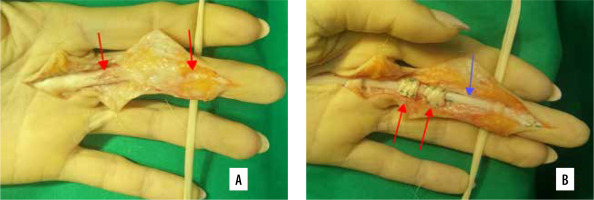
Figure 6
Staged flexor tendons reconstruction in massive scarring and no tendon continuity (A – between arrows): first stage – silicone rod (blue arrow) application with pulley reconstruction (B – pulleys reconstructed with FDS strip: red arrows)
Another group of tendon problems comprises enthesopathy changes. These conditions are easy to confirm clinically, but the aetiology is not easy to detect, whether functional or structural [23,24]. Confirmation of structural problem can affect treatment (e.g. anatomical variance of first extensor compartment that influences surgical technique) or suggest chronic or acute variant (e.g. tennis elbow with the presence of degenerative changes of extensor carpi radialis brevis origin). Ultrasonography or MR performed during treatment can offer these patterns and help determine the treatment method when many choices are possible.
Nerves
Hand surgeons care for various nerve conditions, from compressive neuropathies to nerve injuries, including brachial plexus lesions [25]. Treatment results depend on proper diagnosis and adequate timing. The questions that arise in the treatment of patients with nerve problems include the following:
In compression neuropathies – are there any visible signs of compression, including change in dimension or narrowing of the lesion? Although many studies have been performed on the correlation between radiologic parameters and symptoms, most of the findings do not accurately correlate with clinical presentation. Nonetheless, some can be useful when deciding on a surgical technique. In true Guyon’s canal syndrome, mass can be a source of compression – usually the muscle belly or ganglion. In clinical practice, we often see the correlation between the relief of symptoms and compressive lesions proven by imaging studies. Patients with typical findings of the affected nerve should be continuously assessed for other levels of injury (cervical spine or thoracic outlet syndrome) or neurologic disease. Further work-up, including specialised consultations, is required [26,27].
In nerve lesions – continuity of nerve trunk. Clinical presentation of open injuries (glass, knife) can be easy to assess with clinical examination, but closed injuries such as fracture of the humerus shaft in adults or supracondylar fracture in children are much more challenging [28].
In neglected or unsuccessfully treated nerve injuries – assessment of neuroma in continuity (including fascicles) – gap evaluation including prognosis after neuroma resection is helpful for assessment of the length of the nerve grafts in reconstructive procedures (Figure 7) [26].
Condition of innervated muscles – hypotrophy, atrophy, fatty degeneration.
Figure 7
Nerve reconstruction of the median nerve with sural grafts, the gap after neuroma resection (A – between arrows) can be assessed for planning a proper number of grafts (B – arrow pointing each graft)
Most of these questions can be clarified using a reliable ultrasonographic examination.
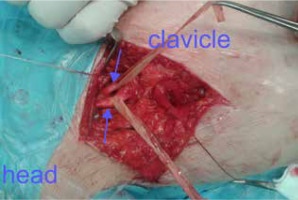
Brachial plexus lesions are challenging for surgeons and radiologists, and preoperative assessment is very important. We usually rely on combined MR and US evaluation to obtain information on possible root avulsion, continuity of brachial plexus, and quality of lesions with continuity. The findings must be strictly compared with a clinical presentation to avoid misunderstandings. Due to the recent development of nerve transfer techniques, precise assessment of the location of the primary lesion is not as important for decision-making as it used to be. The surgery involves beyond the primary area of injury, which is not applicable in all cases (only in partial lesions). Some injuries, such as obstetric palsy, are on the borderline when deciding between surgical and non-surgical treatment. The best assessments are crucial in these cases for making the final decision (Figure 8) [29-32].
Tumours
Hand tumours can be classified as benign and malignant. From a practical point of view, both can be divided into soft tissues or bone, based on the tissue origin.
A large variety of lesions can be found in the hand region, from nodules and tumour-like changes to true neoplasms, representing a challenge for hand surgeons. Even simple changes can be problematic in diagnosis and treatment, including a high risk of recurrence and rare but possible malignant transformation. Malignant tumours are uncommon, but if they occur, the consequences can be severe despite a seemingly small mass [33,34].
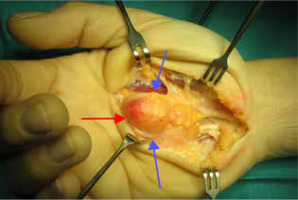
Pathological mass is almost always correlated with a patient’s anxiety, mainly when there are doubts about the diagnosis. Some typical conditions such as ganglion cyst, lipoma, mucous cyst, and Dupuytren’s disease can usually be diagnosed in the clinic using ultrasound. Other benign soft tissue tumours, such as giant cell tumours of tenosynovium or glomus tumours, require more advanced diagnostic modalities, including MR. In cases of hand patho-logy, localisation of the tumour relative to the surrounding structures, such as nerves and vessels, is important for safety when planning surgery [34]. A simple lipoma in the palmar region can include the digital nerve, which can be iatrogenically injured during preparation (Figure 9).
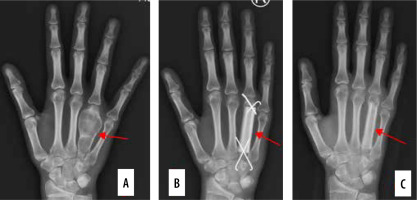
Typical bone tumours, including chondroma, solitary, or aneurysmal bone cysts, can be easily treated, but cases where fast growth or recurrence is seen require thorough preparation with bone resection and assessments of the size of the bone graft (Figure 10).
Complex problems and reconstructions
In many of the presented situations, the structures surrounding tumour lesions must be evaluated. The overall function represents a combination of independent structures and cannot be assessed separately. Tendons will not glide if the joint is stiff, and nerves will not regenerate without an adequate blood supply. We often face complex hand injuries and their sequelae, such as the loss of continuity in the radial/ulnar artery, flexor tendons, and median/ulnar nerve. In some cases, the bony framework may also be disrupted. Preoperative planning is crucial in deciding which imaging studies will be necessary to confirm the final diagnosis. Usually, one modality is insufficient, and each has its advantages and disadvantages. Therefore, it is important to have access to radiologists to discuss the most challenging cases.
Conclusions
Regardless of the region’s specificity, it is fundamental to order proper imaging as part of adequate pre-operative planning and to consult radiologists in most challenging cases. The choice of modality should be derived from the clinical evaluation and the initial diagnosis.
Final imaging results should be precise and confirm the clinical diagnosis to decide on the conservative versus surgical treatment of the hand problem.