In present times, ventilation therapies such as intubation are more prominent, and difficulties have been reported during intubations [1–4]. Endotracheal intubations are critical in the resuscitation of the acutely ill and complications such as bradycardia and hypoxaemia have been reported [5–7]. Laryngoscopy is associated with a reflex sympathetic pressor response resulting in hypertension and arrhythmia [8–12]. During intubations, the haemodynamic responses are mostly short-lived and tolerated by healthy patients but can be detrimental in patients with cardiovascular diseases [13, 14]. Diverse views on the efficacy of intubating laryngeal mask airways (ILMA), Macintosh, and McGrath video laryngoscopy have appeared in the literature [15–20]. Therefore, the present research is a comparative study of haemodynamic changes, time taken, and success rate associated with intubation techniques such as ILMA, Macintosh and McGrath to determine the most efficient of the three techniques.
METHODS
Study design and participants
The study was approved by the Institutional Ethics committee (Sri Ramachandra University: CSP-II/PG/ANE5414001/14/Nov/2017) and the requirement for written informed consent was waived by the ethics committee. No underage subject was enrolled. Study design: This is a prospective, single-blinded, randomised controlled trial. Main outcome measures: The primary outcome was the identification of the most efficient intubation technique. The secondary outcomes were the haemodynamic parameters, time taken for intubation and the rate of success of intubation. In this single-blinded study, the intubating anaesthetist knew the identity of the subject and the laryngoscopic technique used, whereas the anaesthetist recording the parameters was blinded to the identity of the subject and the technique used for intubation. For the sake of uniformity, one of the anaesthetist-authors performed the intubations, and the other recorded the data for all the patients. The intubation and data recording were carried out by highly experienced and professionally trained Masters degree anaesthesiologist-consultants with over eight years of clinical anaesthesia experience. In this study, 90 participants were randomly and equally assigned to ILMA, Macintosh and McGrath groups with a set of random numbers generated by a computer. Inclusion criteria: both sexes, age: 18–55 years, ASA I or II, Mallampati < III, Mouth opening > 2 fingers, BMI < 40 kg m-2 and any elective surgery requiring endotracheal intubation. Exclusion criteria: ASA > II, Mallampati > II, anticipated difficult intubation, GERD, respiratory diseases, cardiovascular diseases, hypertension, history of upper/lower respiratory tract infection within two weeks of intubation and unwillingness to participate.
Sedation protocol, laryngoscopic procedure and data analysis
Baseline vitals were recorded with electrocardio-graphy and noninvasive blood pressure. Oxygen saturation levels were measured with an IntelliVue MP50 pulse oximeter (Philips Healthcare, Eindhoven, Netherlands). Patients were pre-oxygenated with 100% oxygen at the rate of 6 L min-1 for three minutes. Subsequently, anaesthesia was induced with midazolam (0.03 mg kg-1) and fentanyl (2 µg kg-1) intravenously. Induction was completed with propofol (3–5 mg kg-1) and vecuronium (0.1 mg kg-1) injections while bag valve mask ventilation was applied with 100% oxygen and sevoflurane. At the end of three minutes of administration of vecuronium, ensuring complete muscle relaxation with BIS (< 60), orotracheal intubation was performed. No other medications were administered or procedures performed during the data collection period after endotracheal intubation. A patient was randomly allocated to one of the three groups: ILMA, Macintosh, and McGrath. Each group comprised 30 patients. In the ILMA group, a laryngoscope of suitable size (3 for females and 4 for males) was inserted with the head in a neutral position. The cuff was inflated with 20–30 mL of air, maintaining ILMA cuff pressure close to and not exceeding 60 cm H2O as checked by a cuff pressure manometer. As and when ventilation with ILMA was found to be unobstructed, two effective breaths with 100% oxygen and sevoflurane were given. A well-lubricated reinforced, straight silicone tipped ILMA endotracheal tube with a suitable diameter (7.5 or 8 mm) was passed through the metal tube into the trachea, the cuff was inflated, and the circuit was reconnected. For the 30 patients in the Macintosh group the following steps were carried out: i) the laryngoscopic blade was inserted at the right side of the patient’s mouth leading to the right tonsillar fossa, ii) the tip of the blade was advanced until the glottis was visualised, and iii) intubation was completed with the insertion of an endotracheal tube of appropriate size. Disposable laryngoscopic blades are used in the McGrath technique. Thirty patients were assigned to the McGrath group. In this procedure, the disposable laryngoscopic blade was introduced from the centre of the opening of the patient’s mouth. Subsequently, by gentle manoeuvres, the view of glottis was optimised with the help of the attached video screen. In the final step, with just sufficient force to negotiate the glottis, the stylet was removed.
Tracheal intubation was attempted only twice with a particular technique. Heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP) and mean arterial pressure (MAP) were recorded at ‘baseline’ (BL), post-induction (PI), during insertion of the laryngoscope (LI), and every minute until the fourth minute of intubation (M0, M1, M2, M3, M4).
Continuous variables are reported with mean and 95% CIs. The collected data were analysed with IBM-SPSS statistical software version 23.0. In the multivariate analysis, the one-way ANOVA with Tukey-Kramer post-hoc test (for unequal population of groups) was used [16, 21]. The sample size was determined on the basis of a pilot study in which a total of 15 patients were divided randomly into three groups of five each. Collected haemodynamic parameters (mean values) were used to find the parameter “f” as 0.3937 for “effect size”. For α = 0.05, f = 0.3937, power = 90% (numerator df = 2, denominator df = 85, actual power = 0.9082), a total sample size of 87, distributed evenly in three groups of 29 patients in each group was obtained. In the present study, a total of 90 patients were chosen for the investigation (Figure 1).
RESULTS
Of the 90 participants enrolled in this study, 65.4% (59) were female, and 34.4% (31) were male.
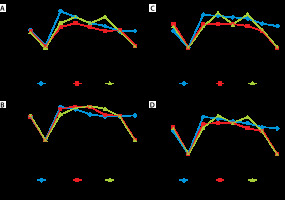
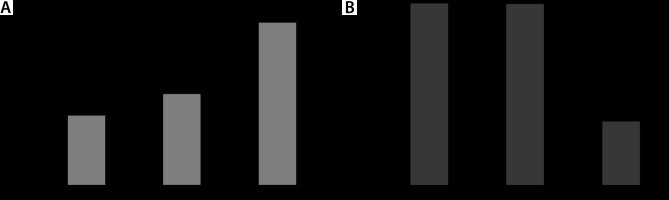
Overall, 58.9% (53) ASA I and 41.1% (37) ASA II patients were investigated, and there was no significant difference in ASA grading between the groups (Table 1). One-way ANOVA was performed on data collected at different time points of intubation and only Fs (2, 85) > Fc (= 3.10) and P = 0 indicated significant differences among the three values of X– . The Tukey-Kramer (T-K) test was then performed, and qs (3, 85) > qc (= 3.40) suggested statistical significance for a pair. Analysis of BL haemodynamic parameters with one-way ANOVA showed no statistically significant differences with respect to HR (Fs = 0.099, P = 0.905), SBP (Fs = 0.150, P = 0.860), DBP (Fs = 1.493, P = 0.230) or MAP (Fs = 1.532, P = 0.221). A similar analysis of the post-induction, haemodynamic parameters also exhibited statistically insignificant differences for the three techniques (HR (Fs = 0.099, P = 0.905, X– = 61.79 ± 1.87), SBP (Fs = 0.150, P = 0.860, X– = 105.00 ± 1.78), DBP (Fs = 1.493, P = 0.230, X– = 63.97 ± 1.84) and MAP (Fs = 1.532, P = 0.221, X– = 77.72 ± 1.48). A comparison of the BL and PI parameters clearly reveals a clinically favourable drop in haemodynamics during induction. The laryngoscope insertion process had an impact on haemodynamic parameters in all three groups. In general, no significant differences were found between BL, PI and M3 time points of the intubations. At M2, ILMA assisted intubations showed a significant spike in haemodynamic parameters due to its removal manoeuvre. At the LI time point, statistically significant differences were observed in the one-way ANOVA examination of HR data, and hence a subsequent Tukey-Kramer (T-K) test showed statistically significant differences in the following increasing order: McGrath < ILMA < Macintosh (Table 2 and Figure 2A). At M0 and M1 time points, the McGrath group demonstrated the lowest heart rates and statistical analysis supported the inference. After two minutes of intubation, in the ILMA group, an increase in heart rate was registered, while at the same time, the McGrath group registered the lowest heart rate. McGrath and ILMA intubations showed comparable HR after four minutes of intubation (M4) (Figure 2A). Statistically indistinguishable nature of McGrath and ILMA HR was indicated by AT-K (one-way ANOVA followed by Tukey-Kramer test) analysis with qs (McGrath–ILMA) = 0.10 < qc (= 3.40) (Table 2). Statistically significant differences in SBP were not observed among the three groups at BL, PI, M0 and M3 time points of intubation. McGrath (X– = 105.46 ± 2.64 mm Hg) and ILMA groups (X– = 104.96 ± 2.01 mm Hg) displayed lower SBP at the M4 time frame compared to the Macintosh group (X– = 128.36 ± 2.64 mm Hg). SBP values of the McGrath and ILMA groups were statistically indistinguishable, and the observation was supported by Tukey-Kramer analysis (qs = 0.43). During the insertion of the laryngoscope, the DBP was the highest in the Macintosh group. McGrath and ILMA guided intubation groups displayed statistically indistinguishable behaviour with comparatively lower values in the M4 time frame. At LI, M0, M2 and M4 time points of intubation, statistically significant differences in MAP were observed among the groups (Table 2 and Figure 2D). After the fourth minute of intubation, McGrath and ILMA groups displayed an identical decrease in MAP (qs = 1.01). The mean time (95% CI) taken for intubation procedures with Macintosh, McGrath and ILMA techniques are 30.63 ± 1.53, 40.26 ± 1.36, and 71.64 ± 2.14 seconds, respectively (Figure 3). One-way ANOVA showed the presence of statistically significant differences between the three groups (Fs = 589.5 > > Fc = 3.10, P = 0). The sub-sequent Tukey-Kramer test showed that all three pairs of groups differed statistically significantly (Macintosh-McGrath [qs = 11.15]; McGrath-ILMA [qs = 35.68]; Macintosh-ILMA [qs = 46.64]; qc = 3.40). Macintosh and McGrath intubations were all successful, while two failures were reported in the ILMA group, but the failures observed were statistically insignificant (95% CI: 93.33 ± 4.35%) (Figure 3).
TABLE 1
Gender and ASA grade distribution
TABLE 2
Mean haemodynamic parameters and the results of one-way ANOVA and Tukey-Kramer test
[i] PI – post induction, LI – laryngoscope insertion, M0, M1, M2, M3 and M4 – just after intubation, first, second, third and fourth minutes after intubation. HR – heart rate, SBP – systolic blood pressure, DBP – diastolic blood pressure, MAP – mean arterial pressure; MAC – MACINTOSH, MCG – McGrath, ILM – ILMA; X– = Mean with CI, 95%; A – one-way ANOVA, Fs – F-Statistical, Fc – F-Critical: 3.10. ‡Because of absence of statistically significant difference, Tukey-Kramer test was not performed, T – post-hoc Tukey-Kramer test; qc = 3.4, critical q value from Student’s t test table for number of groups = 3 and degrees of freedom equal to 85. *Statistically significantly difference observed and Tukey-Kramer test was carried out.
DISCUSSION
One-way ANOVA for all the haemodynamic parameters at BL, PI and M3 time points showed no statistically significant differences. A comparative analysis of obstetric intubations showed higher mean HR during McGrath intubations relative to Macintosh [22]. A critical conclusion from the A T-K analysis of the HR data in the present study is the fact that the McGrath technique registered the lowest HR relative to the other two techniques at LI, M0, M1, M2 and M4 time points, which is supported by a recent study [23]. The highest mean HR recorded at the second minute of intubation with ILMA was attributed to its removal manoeuvre, as reported earlier [24, 25]. Both McGrath and ILMA groups recorded the lowest HR after the third minute of intubation. After the fourth minute of intubation, SBP reported for the McGrath group showed a minimum. Similar data analysis of the McGrath group’s DBP and MAP revealed that both parameters displayed corresponding minima at M0, M2 and M4 time points (Table 2, Figure 2C and D). Mean DBP recorded from LI to M4 time frames for the McGrath group was the lowest among the three groups. Screening of the data related to Macintosh guided intubations showed a statistically significant spike in HR when the laryngoscope was inserted (Figure 2A), and subsequently maintained a steady state until four minutes were completed. For the Macintosh group, relatively low SBP was observed among the three groups after completion of the first minute of intubation, and then remained steady until the fourth minute. However, the lowest SBP values among the three techniques were recorded for the Macintosh and McGrath groups after the completion of two minutes of intubation (Figure 2B). Compared to McGrath, the Macintosh group showed higher DBP and MAP from LI to M4 time frames. The ILMA group displayed higher HR, SBP, DBP and MAP values after two minutes of intubation due to the removal manoeuvre of ILMA uniformly, though there are a few contradicting reports [26–28]. After induction, the number of minima observed for the four haemodynamic parameters in the time series plot is 12 (McGrath) > 8 (ILMA) > 2 (Macintosh) (Table 2, Figure 2A–D), which clearly identified the McGrath technique as the most efficient. One-way ANOVA, followed by a Tukey-Kramer analysis of the time taken for intubations, indicated the increasing order of the groups: Macintosh < McGrath< ILMA, in line with a recent study [27]. McGrath required marginally more time for intubation than the Macintosh technique. Statistically, rates of success of the techniques were indistinguishable. In our study, there was no episode of desaturation.
CONCLUSIONS
Among the three techniques, ILMA required the longest time. There was no statistically significant difference in success rates between the techniques. Although McGrath intubation was slightly more time consuming than Macintosh, McGrath is the most advantageous technique due to its highly favourable haemodynamic response.