Introduction
Gallstone disease is a common disorder affecting the biliary tract and is considered the outcome of a lowered biliary epithelium contractility, supersaturated cholesterol in bile, and inadequacy of bile salt function/levels. It is typically influenced by factors such as hormones, diet, and genetics [1, 2]. The incidence of gallstones is 10–20% [3], which is further increasing with the worsening of living standards, poor dietary habits, and environmental deterioration. Most patients with gallbladder stones remain asymptomatic throughout their life, but approximately 13–22% eventually develop symptoms [4]. Acute choledocholithiasis (AC) is often a result of gallbladder stones migrating into the biliary tree, which has been considered one of the most common complications in patients with gallstones [5–7]. Reportedly, approximately 8–20% of patients with gallstones have choledocholithiasis [8]. AC frequently results in obstructive jaundice, biliary colic, cholangitis, acute pancreatitis, and even liver cirrhosis if not addressed early [9].
The traditional treatment for AC is open choledocholithotomy with T-tube drainage (TD) [10]. Laparoscopic common bile duct exploration (LCBDE) was first successfully performed by Stoker et al. in the United States in 1991 [11]. Since then, the treatment pattern for gallstone and choledocholithiasis has changed substantially. With the improvement of minimally invasive techniques such as laparoscopy and choledochoscopy, clinical treatment is more inclined toward laparoscopy combined with choledochoscopy for common bile duct (CBD) exploration and stone removal [12]. On completing laparoscopic choledochotomy, TD of the CBD is traditionally employed to prevent biliary stricture and biliary fistula [13]. However, LCBDE with T-tube drainage often causes discomfort and complications such as retrograde biliary tract infection that ascends through the drain. As an alternative scheme, the primary closure (PC) of the CBD on completion of laparoscopic choledochotomy has been proposed [14, 15]. Many systematic reviews have recently shown that PC of the CBD after LCBDE provides better therapeutic outcomes than TD of the CBD after LCBDE [16].
Aim
In this retrospective study, we evaluated the therapeutic outcomes of PC and TD after LCBDE in the surgical treatment of acute choledocholithiasis and assessed the safety and effectiveness of PC after LCBDE in acute choledocholithiasis patients.
Material and methods
Patient selection and review
From January 2015 to December 2019, 232 patients with acute choledocholithiasis who received PC or TD after LC + LCBDE at The Third Affiliated Hospital of Soochow University were enrolled in this study. All patients had different degrees of right upper abdominal pain, jaundice, and other symptoms at admission.
The inclusion criteria were as follows: 1) patients whose common bile duct stones were confirmed by preoperative routine abdominal (hepatobiliary, splenic, and pancreatic) colour ultrasound, upper abdominal computerized tomography, or magnetic resonance cholangiopancreatography (MRCP); 2) patients with no intrahepatic bile duct calculi; 3) patients with no other liver diseases or serious comorbidities; and 4) patients with no history of abdominal surgery. Patients with Mirizzi syndrome or those who required open surgery due to difficulty clearing stones were excluded. This study was approved by the Ethics Committee of The Third Affiliated Hospital of Soochow University.
LCBDE technique
Under general anaesthesia, the patient was placed in the supine position with the head elevated and the left side of the soles of the feet tilted by 30°. A trocar was placed according to the “4-hole method” for cholecystectomy. Pneumoperitoneum was established, and the abdominal cavity was explored. If no abnormality was found, the gallbladder triangle was dissected for complete exposure. A Hem-o-lock clamp was used to ligate the gallbladder duct. An absorbable clamp was used to close the cystic artery and resect it. The CBD was exposed, and a longitudinal incision was made on the anterior wall of the CBD using an electric hook to drain bile; the length of the incision depended on the size of the stone diameter. A 30-mm pipe was inserted through the trocar into the CBD from the xiphoid process, and we rinsed with normal saline from a 50-ml syringe at low pressure to remove the calculi in the distal end of the CBD. If we encountered hard stones, stone baskets or electrohydraulic lithotripsy (EHL) were applied under the choledochoscope. Subsequently, choledochoscopy was performed to probe the CBD, the common hepatic duct, and the left and right hepatic ducts to ensure that there were no residual stones and that the duodenal papilla opened and closed normally.
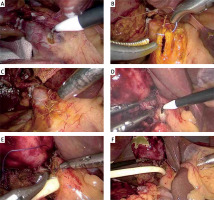
For patients who underwent PC, the CBD incision was continuously sutured with a 4-0 unidirectional barbed wire (Photos 1 A–C). For patients who underwent TD, a latex T-tube of the proper size (18–22) was placed in the CBD, and the front wall of the CBD was sewn intermittently with the same suture material and technique. The T-tube was removed using a trocar in the midclavicular line, and normal saline was pumped into the T-tube using a 50-ml syringe to ensure no fluid leakage at the CBD incision (Photos 1 D–F).
Photo 1
Representative images of T-tube drainage and primary closure. A–C – representative images of primary closure. A – Free anterior wall of the common bile duct before opening, B – primary closure of the common bile duct after LCBDE, C – completed primary suture of the common bile duct. D, E – representative images for T-tube drainage. D – The free anterior wall of the common bile duct before opening, E – insertion of the T-tube and interrupted suture after LCBDE. F – The common bile duct sutured after insertion of the T-tube
For patients undergoing cholecystectomy, the gallbladder was detached from the serosal membrane, and the haemorrhage from the gallbladder bed was stopped by electrocoagulation. The gallbladder was removed from the xiphoid process using a trocar through the gallbladder bag. Intraoperatively, the abdominal cavity was rinsed, and an abdominal drainage tube was routinely placed through the Winslow hole.
Evaluation indicators and follow-up
The following indicators were retrospectively reviewed and compared between the PC and TD groups: operation time, CBD suturing time, estimated blood loss, intraoperative transfusion, the stone removal method, postoperative liver function, gastrointestinal recovery, the time of drainage removal, postoperative hospital stay, and complications. All patients were followed up for 6 months. Liver function tests and abdominal ultrasound were performed every 3 months. Further MRCP was performed if necessary.
Statistical analysis
Data were analysed using SPSS 21.0 software (SPSS Inc., Chicago, IL, USA). Measurement data are presented as mean ± standard deviation. The independent t-test was used for comparisons between groups. Count data were compared between the groups using the χ2 test. Statistical significance was set at p < 0.05.
Results
Between January 2015 and December 2019, a total of 232 patients with a mean age of 60.83 ±12.26 years, who were diagnosed with acute choledocholithiasis were enrolled in this retrospective analysis. Patients were categorized into the PC (n = 102) and TD (n = 130) groups. Table I lists the demographic and clinical data. As Table I shows, The PC group was composed of 52 females and 50 males whereas the TD group consisted of 67 females and 63 males. There were no significant differences in age (58.24 ±16.18 vs. 63.08 ±6.84 years; p = 0.118), body mass index (BMI) (25.65 ±1.75 vs. 25.66 ±1.63 kg/m2; p = 0.948), comorbidities (hypertension: 52 (51.0%) vs. 67 (51.5%); p = 0.933; diabetes: 22 (21.6%) vs. 31 (23.8%); p = 0.682), or preoperative liver function (total bilirubin (TBIL) 56.01 ±40.17 vs. 65.12 ±35.78 μmol/l; p = 0.449; alanine transaminase (ALT) 240.05 ±246.81 vs. 244.05 ±251.99 U/l; p = 0.959). In the preoperative imaging data, no significant differences were found in the number of CBD stones (1.70 ±0.78 vs. 1.62 ±0.75; p = 0.426) or CBD diameter (10.86 ±0.44 vs. 11.23 ±0.47 mm; p = 0.882) between the 2 groups, suggesting that the groups were comparable.
Table I
Demographic data and clinical characteristics of all patients
All surgical operations were performed successfully without conversion to other procedures. Significant differences were observed in operating time (95.22 ±19.35 vs. 115.96 ±26.80 min; p < 0.001) and CBD suturing time (9.66 ±2.50 vs. 14.59 ±11.49 min; p < 0.001) between the groups. However, there was no significant difference in estimated blood loss (27.38 ±26.06 vs. 27.75 ±21.67 ml; p = 0.961). In 50 and 71 patients in the PC and TD groups, only pipe washing was used to remove stones in the CBD (50 (49.0%) vs. 71 (54.6%); p = 0.397). No significant difference was found. The rate of basket use (51 (50.0%) vs. 55 (42.3%); p = 0.243) and EHL use (1 (1.0%) vs. 4 (3.1%); p = 0.525) was also similar in the 2 groups (Table II).
Table II
Comparisons for intraoperative situations between the 2 groups
All patients were routinely treated for infection prevention, liver protection, and fluid rehydration after surgery to keep the T-tube and abdominal drainage unobstructed. As shown in Table III, patients in the PC group had a significantly shorter time of gastrointestinal recovery (2.33 ±0.66 vs. 3.15 ±0.80 days; p = 0.002), time of drainage removal (5.35 ±1.87 vs. 6.30 ±1.49 days; p < 0.001), and time of postoperative hospital stay (6.38 ±3.20 vs. 8.80 ±1.44 days; p = 0.004) than those in the TD group. However, the postoperative liver function (TBIL 20.35 ±10.48 vs. 23.83 ±9.64 μmol/l; p = 0.275; ALT 41.95 ±27.69 vs. 44.85 ±21.76 U/l; p = 0.712) in the 2 groups was similar with no significant difference. Table III also shows the postoperative complications between the 2 groups. Three patients had postoperative bleeding and were cured by non-surgical means. There was no significant difference between the PC and TD groups (1 (1.0%) vs. 2 (1.5%); p = 1.000). Biliary leakage occurred in 3 cases in each group. According to the bile leakage grading system, these 6 patients belonged to grade A and were cured by conservative treatment (3 (3.0%) vs. 3 (2.3%); p = 1.000). It was statistically similar in the PC and TD groups in terms of incision infection (0 (0.0%) vs. 3 (2.3%); p = 0.338) and cholangitis (1 (1.0%) vs. 5 (3.8%); p = 0.343). No postoperative mortality occurred in either group. No significant difference in residual stones was found in the 2 groups (2 (2.0%) vs. 4 (3.1%); p = 0.908).
Table III
Comparisons for postoperative situations and complication between the 2 groups
Among the 6 patients with residual stones, 2 in the PC group were treated with ERCP, and 4 in the TD group underwent extraction through the T-tube sinus tract using a choledochoscope. All patients were followed up for 6 months. During the follow-up period, only 1 case in the PC group showed biliary stricture and was cured by biliary stent insertion (1 (1.0%) vs. 0 (0.0%); p = 0.903). One patient in the TD group was found to have stone recurrence and was treated using ERCP (0 (0.0%) vs. 1 (0.8%); p = 1.000).
Discussion
In 2008, guidelines on managing CBD stones proposed that LCBDE can be used in their treatment [17]. Since then, open choledocholithotomy has been gradually replaced by minimally invasive laparoscopic techniques. LCBDE has significant advantages, including minimal invasion, direct visualization, and optical magnification. In addition, LCBDE preserves the integrity of the sphincter of Oddi and avoids bile reflux. Moreover, LCBDE during laparoscopic cholecystectomy allows for dealing with both problems simultaneously under a single anaesthesia, resulting in effective stone extraction and low morbidity [18, 19]. Considering the possibility of duodenal papilledema caused by blockage of the lower end of the bile duct, severe oedema of the bile duct wall, and biliary leakage caused by excessive biliary pressure, TD is routinely placed after LCBDE. T-tubes have the function of biliary duct support to prevent stricture and are conducive to postoperative cholangiography to check whether there are residual stones in the CBD. They are also used to retain the postoperative choledochoscope for stone removal and avoid reoperation and relieve pain.
Nevertheless, insertion of a T-tube has underlying drawbacks and risks of complications, such as affecting fluid and electrolyte imbalances (especially Na+), digestive function, biliary obstruction, cholangitis caused by microorganisms retrograde through the T-tube, risk of tube shedding, and localized pain [20]. It takes a long time for patients with TD to recover after surgery and to ensure T-tube patency. Moreover, postoperative bile leakage cannot be avoided entirely with T-tube drainage [21]. In addition to the discomfort and inconvenience caused in the patients’ daily life, living with a T-tube for a few weeks also leads to the development of an abdominal scarring and adds a psychological load to patients, badly affecting their quality of life.
An increasing number of studies have compared the effect of LCBDE with and without TD in the past few years [14, 22–24] and revealed that PC of the CBD for patients with choledocholithiasis is effective and safe [23]. These studies demonstrated the superiority of LCBDE with PC of the CBD in terms of the decrease in operation time, suturing time, length of postoperative hospital stay, and hospitalization costs [14, 22–24]. In a review, Gurusamy et al. reported that, compared with PC, TD had a remarkably long operation time and prolonged the length of hospital stay with no evidence of benefit after LCBDE [16]. Yin et al. indicated that PC is superior to TD among patients receiving LCBDE, but no significant benefit was observed in terms of PC with various external or internal drainage techniques [25].
In this study, consistent with past studies, the average operation time and CBD suturing time in the PC group was significantly shorter than in the TD group, indicating that intracorporeal suturing is easier to perform than by T-tube drainage. It is worth noting that a knotless barbed suture and excellent laparoscopic skills, including suturing and knotting with laparoscopic instruments, are necessary to ensure the advantage of PC. Our results also showed that the PC group had a significantly shorter time of resumption of gastrointestinal function and decreased length of postoperative hospital stay and drainage removal than the TD group. Several factors might be responsible for such differences between the TD and PC groups: 1) patients undergoing TD lose some bile, which is an important component of digestive juices, due to long-term external drainage, which could result in water and electrolyte disturbances, loss of appetite, gastrointestinal dysfunction, and slow recovery; 2) the T-tube is a foreign body, and it is easy to stimulate the biliary tract and increase the possibility of biliary tract infection if it is kept in the CBD for a long time, which extends the drainage removal time; and 3) living with a T-tube for a long time causes a burden to patients, and postoperative care of the T-tube is needed, which extends the patients’ hospital stays. PC is associated with minor trauma, rapid recovery, and a short length of hospital stay, with no need for the T-tube postoperatively, reflecting the superiority of minimally invasive surgery and supporting accelerated rehabilitation after surgery.
Moreover, the risk of biliary leakage induced by high biliary pressure and biliary stricture considered before surgery is minimized due to the proficiency of the laparoscopic suture technique and improved suture materials. The careful suture and the closure with 4-0 unidirectional barbed lines can reduce the occurrence of biliary leakage. Several studies have found no significant difference in postoperative biliary leakage between PC and TD groups [24–26]. The absorption of unidirectional barbed lines after surgery also significantly reduces the incidence of biliary stricture [26].
In our study, mild biliary leakage was observed in 3 patients in each group, and they recovered with conservative treatment without further complications. Three cases of biliary leakage occurred in the PC group at the early stage of this study. The main reason is that there is a barb-free segment of approximately 5 mm in the round coil at the end of the barbed wire; therefore, the first suture should be adequately away from the lower edge of the CBD incision (about 3 mm) to prevent bile leakage at the end of the barbed wire suture without barbed wire. The suture clockwise distance and edge distance should be kept at 2 mm. After the improved suture method, there is no bile leakage.
Residual stones are a major complication of LCBDE combined with PC. Some studies even reported that the rate of residual stones after LCBDE with PC was up to 3.5% [26]. In our study, the rate of residual stones was similar between the PC and TD groups. Because of intraoperative choledochoscopy, the probability of residual stones is decreased. However, for emergency patients with severe acute choledocholithiasis, TD after LCBDE is a preferred option. Incision decompression of the CBD is the most important for patients with severe acute choledocholithiasis, and shortening the operation time could reduce the risk of surgery. Taking a long time to remove all CBD stones should be avoided. TD could provide a second chance to remove CBD stones postoperatively through a T-tube track.
It has been demonstrated that PC of the CBD after LCBDE is not applicable for all patients with acute choledocholithiasis [27]. In patients with outlet stenosis of the CBD or acute obstructive suppurative cholangitis, continuous decompression and drainage are required, and therefore PC is not recommended for these patients. In addition, PC is relatively prohibited for patients with very thin CBDs due to a higher risk of biliary leakage [28, 29]. The indications for PC of the CBD on completing LCBDE include the following: 1) patients with no recent episodes of severe biliary inflammation; 2) patients with a single CBD stone measuring < 2 cm; 3) cases in which the CBD is dilated at least 8 mm; 4) no residual stone in the bile duct and no intrahepatic bile duct stone; and 5) no apparent obstructive jaundice, the lower part of the CBD is unobstructed, and the choledochoscope can enter the duodenum smoothly. We suggest the need to always check for surgical indications, which should be determined on a per-patient basis, as well as the operative level and experience of the surgeon. Surgical indications can be appropriately relaxed in principle under the premise that the lower end of the CBD is unobstructed. For example, several patients who received PC of the CBD after LCBDE in our hospital had a CBD diameter of approximately 7–8 mm. The patients recovered well after surgery, and no bile leakage or CBD stenosis was observed. Certainly, some surgical units prefer to resolve CBD lithiasis with use of ERCP at first, and then perform cholecystectomy. ERCP + LC and LCBDE + LC were both safe and feasible in the management of grade I or II acute calculous cholangitis. Zou et al. compared the effect between an ERCP + LC group and an LCBDE + LC group, and they verified that, compared with the protocol of ERCP + LC, the protocol of LCBDE+LC had the advantages of fewer complications and lower therapeutic costs [30]. However, further studies are needed to verify these conclusions.
Conclusions
In our study, after LCBDE and intraoperative choledochoscopy, PC was superior to TD in terms of the operation time, CBD suturing time, gastrointestinal recovery time, drainage removal time, and postoperative hospital stay, and both have comparable incidences of intraoperative blood loss, method of removal stone, and complications. PC after LCBDE is safe and effective for patients with acute choledocholithiasis, and this effective treatment method is worthy of selection by surgeons.









