Introduction
Endoscopy plays a vital role as a method of diagnosis and treatment in different fields of modern surgery. This is because it is less invasive and usually has a shorter recovery time. For a long time, medical doctors used different types of endoscopy to make a proper diagnosis. The first description of anoscopy and treatment of haemorrhoids is available in the works of Hippocrates [1]. John Macintyre manufactured the first self-illuminated endoscope at Glasgow Royal Infirmary in 1894 or 1895. Since then, we have made tremendous progress by applying endoscopy in nearly every surgical subspecialty.
One of the elements of evaluating surgical procedures is their safety. To increase patient safety and support surgical education, surgeons should train their surgical skills. They gain experience through fellowship programmes under the supervision of the licensed practitioner. It is widely believed that surgeons should be talented manually and have other predispositions such as resistance to stress and the ability to make quick decisions. One of the most significant challenges nowadays is to educate and predict the preferences of young surgeons taking into consideration that every skill has a learning curve.
Endoscopic simulators could help in perfecting skills before operating on patients.
Although according to Grantcharov [2] preparation for becoming good at technical skills should concern three main components – the cognitive knowledge surrounding the specific medical conditions, instruction enabling abilities that will prepare students by giving them the fundamental elements needed to perform particular procedures and an opportunity to perform a procedure in an environment that is safe and close to real conditions – it could be done outside the clinical setting, reducing the number of errors and increasing the speed of performing the task on patients, which is crucial in times of pressure on speed and maximum efficiency.
Aim
The aim of the study was to investigate the shape and the length of the learning curve in performing three simple tasks on the endoscopic simulator in relation to selected factors (playing a musical instrument, doing physical activity, playing computer games, time achieved in the Minnesota Manual Dexterity Test).
Material and methods
To perform this study, the Laparo Aspire endoscopic simulator was used (Photo 1). This trainer is quite simple equipment that needs to be connected to a computer and allows simple tasks to be performed with endoscopic instruments. Also it is rather inexpensive, at about $400. It is equipped with several training modules – three of them were used in our research.
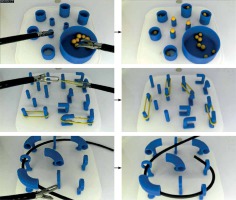
A group of 20 students was recruited for the study of the Poznan University of Medical Sciences. Each participant took part in 4 sessions, and each course was composed of two parts: 12 min of self-directed training and completing three tasks. Photo 2 shows tasks that had to be completed in each session.
The initial state on the left and the final state on the right. First row – transferring balls between containers. Second row – change in the configuration of elastic bands. Third row – placing a rubber line through circles.
Tasks that need to be completed on each course are: (1) to move small balls between containers; (2) to change the configuration of elastic bands stretched between sticks; (3) to pass a rubber line through circles (Photo 2).
The time that was spent to complete each task during each session was measured.
To find factors that may influence the participant’s performance, all students were asked to fill in two surveys: one at the very beginning of the study, and the second before each session.
In the first survey the following data were collected: age, sex, field of study, year of study, handedness, type of sport that is regularly played (if any), whether he/she plays a musical instrument, amount of time that he/she spends and has spent on playing computer games, chronic disease and whether he/she has ever used endoscopic equipment.
In the second survey (that was carried out before each session) the following data were collected: level of stress, number of hours that were spent on sleeping last night, drinking coffee or energising drinks, smoking, physical activity in previous 24 h, drinking alcohol in last 24 h, taking drugs in last 24 h.
The Minnesota Manual Dexterity Test (MMDT) is a unified test for rating an ability to move small objects for various distances. It measures the subject’s ability of rapid eye-hand coordination and arm-hand dexterity. It was used previously in occupational therapy, and physical therapy, especially when assessing progress after using different treatment methods due to injuries or rehabilitation [3–5].
Participants were asked to perform one of the subtests of this test – the placing test [4]. We measured four trials of the placing test, and we calculated the average time of performing this test.
Results
The mean age of the participants was 22.95 years (range: 20–29 years). Fourteen men and six women took part in our research.
Our research revealed that the mean time of performing each task decreased in every session (when compared to the previous session). All participants were right-handed and studied medicine (Figure 1).
Figure 1
Average time of performing tasks on each training day (in seconds) and logarithmic learning curve fitting
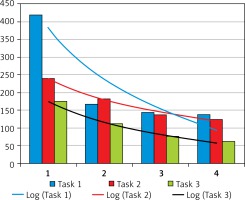
Improvement in time of performing tasks after the fourth session was 75% for the first task (moving small balls between containers), 50% for the second task (changing configuration of elastic bands stretched between sticks) and 67% for the third exercise (passing a rubber line through circles). The Friedman test with the post-hoc test (Dunn Bonferroni test) was performed to determine whether differences between times of completing each task in each session were statistically significant. For each task, a statistically significant difference occurred between different sessions (Table I).
Table I
Results of Friedman test with post-hoc test (Dunn Bonferroni) for each task (yes – significant difference, no – no significant difference)
| Session number | Exercise 1 | Exercise 2 | Exercise 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 | |
| 2 | Yes | No | No | ||||||
| 3 | Yes | No | Yes | Yes | Yes | No | |||
| 4 | Yes | No | No | Yes | Yes | No | Yes | No | No |
Ramsay et al. have shown that the learning curve can be approximated in the most accurate way by a logarithmic curve. Based on that calculated logarithmic curve, coefficients for each task were calculated.
According to that, it seems that each task has its own level of difficulty. A significant correlation between the learning curve of transferring rubber bands (task 2) and threading (task 3) was documented, thus suggesting similar complexity of these tasks.
Figure 1 shows approximated learning curves of tasks 1–3. The mean time of performing MMDT was 57 s (range: 44–75 s).
To assess whether there is a correlation between the MMDT result and the time to accomplish each task, Spearman’s rank correlation coefficient was calculated. No statistically significant correlation was found. Also, Spearman’s rank correlation coefficient for the comparison between tasks was carried out, and a significant correlation (p < 0.05) was found.
Comparison of participants who used to take part in specific activities in their free time with those who did not revealed a significant difference in results achieved on the simulator. Playing music, playing computer games and doing physical activity were assessed (Table II).
Discussion
The goal of the study was to determine the shape of the learning curve of laparoscopic work and evaluate whether chosen factors affect the speed of task execution.
After reviewing the available medical literature, we noted that several similar studies focus on the use of various simulation methods and the resulting improvement in abilities, not only in orthopaedics or surgery but in medicine in general. Training and simulation are seen today as an essential element in medical education and are increasingly appearing in the teaching of students and residents, ensuring more excellent patient safety [6]. It is also necessary to emphasise a higher value of the practical training over the observation itself [7]. However, as Panek et al. reported, not only manual skills influence the learning curve of an individual but also their experience with regard to the entire therapeutic process, including choice of the optimal surgical method [8].
It has been proven that much more expensive virtual reality simulators bring equal benefits to those in training, compared to box trainers, to which the Laparo Aspire belongs [9–11]. Therefore, one can confirm the benefits of the availability of training on box trainers, which one can even take home. However, even though they can effectively support the laparoscopic training, personal possession of a portable simulator does not result in voluntary long-term practice [12].
In the studies comparing also the mental training, which turns out to be very important in the case of additional stress factors appearing during an operation [13, 14], one can note the decisive advantage of training on box simulators and virtual training simulators over mental training [15] in the matter of laparoscopic performance, which also confirms the validity of practical training on simulators. There are also studies available that support the superiority of training on box trainers over virtual reality trainers [16].
To assess the length and shape of the learning curve of laparoscopic work and factors affecting the speed of task execution, 20 medical students completed questionnaires and performed training on the endoscopic simulator. The findings indicate a logarithmic learning curve with a marked improvement in results after all training and research sessions. No error frequency was recorded as it was assumed that the error would directly affect the time necessary to complete the task. The decrease in path length, which can be used for assessment in curricula for laparoscopic cholecystectomy [17, 18] and rating in surgical skills [19] is seen by some as a somewhat manual skill, developed with task repetition. However, error frequency is a crucial component in the clinical marker, and the indicator of the quality of the operation [20] was left unrecorded. It has been shown that a decrease in error frequency number is possible to achieve in structured coaching [18], which was lacking in our study.
Cumpanas et al. [21] examined how sleep deprivation influenced performance on the robotic virtual reality simulator. In their research sleep deprivation does not influence the time of performance on easier tasks but influences time of performing more difficult tasks.
During training sessions, we noted that the type of exercise performed in the current study had a positive effect on the students’ abilities. The Laparo Aspire simulator proved to be an excellent learning method, mainly for simple tasks. What is more, for students who have never had a chance to deal with laparoscopic work, such training was an introduction to a two-dimensional vision. It is undoubtedly one of the significant difficulties faced by amateurs of laparoscopic surgery.
During the university classes, medical students have practically no contact with the laparoscope, apart from observing the procedures carried out by older, experienced surgeons. Medical students and young adepts of orthopaedics and surgery should have constant contact with laparoscopic trainers [21–23].
In contradiction to Buckley CE’s findings, which state that high aptitude is directly related to earlier completion of the learning curve [24], our studies did not show a significant correlation between the results in the MMDT test and the laparoscopic work.
The weakness of our study might be an insufficient number of surveyed students, which could be a reason for limited and inadequate trends for initial aptitude and the length of the learning curve. Despite the size of our group of participants, our findings that laparoscopic training improves performance correlate with those of others [25, 26]. We should also consider introducing more complex tasks to lengthen the learning curve.
To further advance our study, we would also like to compare the results that the students achieved with the results achieved by the experienced surgeons who work laparoscopically daily, to confirm the trends observed by other researchers [27].
One may suspect that, as in some studies [28], training on the box trainer can produce similar results compared to traditional methods, where experienced surgeons educate trainees through the process of graduated responsibility. On the other hand, we think that, based on the learning curve in our research, results of a randomised controlled trial that show how laparoscopic surgical skills are significantly improved by use of a portable laparoscopic simulator [29] and other studies proving that warm-up sessions before operations cause improvement of performance [30, 31] training on the box trainers and/or laparoscopic simulators may be widely and effectively used in many different aspects. As other researchers discovered, many attempts are required in different surgery cases to stabilize the learning curve [32]. That is why targeted training sessions are required to obtain sufficient proficiency.
Conclusions
The assessment made in our study suggests that regular training on an endoscopic simulator significantly decreases the time needed to perform different tasks (both in general and compared to the previous session). We did not find a significant correlation between initial aptitude and the time necessary to complete given tasks. What is more, we should consider comparing students with experienced surgeons.