Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CORONARY ARTERY DISEASE / CLINICAL RESEARCH
Associations of changes in patient characteristics and management with decrease in mortality rates of men and women with ST-elevation myocardial infarction – a propensity score-matched analysis
1
2nd Cardiology Clinic, Swietokrzyskie Cardiology Center, Kielce, Poland
2
The Faculty of Medicine and Health Sciences, The Jan Kochanowski University, Kielce, Poland
3
Department of Interventional Cardiology, Świętokrzyskie Cardiology Center, Kielce, Poland
4
3rd Department of Cardiology, School of Medicine with the Division of Dentistry
in Zabrze, Medical University of Silesia in Katowice, Silesian Centre for Heart Diseases, Zabrze, Poland
Submission date: 2017-10-16
Final revision date: 2017-11-13
Acceptance date: 2017-11-15
Online publication date: 2020-03-10
Publication date: 2020-05-26
Arch Med Sci 2020;16(4):772-780
KEYWORDS
womenregistryall-cause mortalityin-hospital mortalitySTEMIpropensity scoreclinical characteristicsgender-related mattersmanagement and treatmentST-elevation myocardial infarction
TOPICS
ABSTRACT
Introduction:
The aim of this study is to estimate how much of the recent decrease in mortality among patients with myocardial infarction with ST-segment elevation (STEMI) can be attributed to improved treatment strategies, and how much it is related to changes in baseline clinical characteristics, and to compare these findings for men and women.
Material and methods:
This was a retrospective analysis of 32,790 patients with STEMI from the Polish Registry of Acute Coronary Syndromes PL-ACS hospitalised in 2005 and 2011. Changes in treatment strategies including pharmacotherapy were analysed. Observed in-hospital and 12-month mortality rates were compared with the outcomes in the groups matched on the propensity scores.
Results:
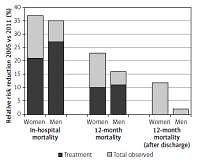
There was a substantial improvement in STEMI patient management between 2005 and 2011 in Poland. It included greater use of percutaneous coronary interventions and other guideline-based adjunctive therapies, and it was associated with a significant decline in in-hospital mortality. Relative 12-month mortality reduction rates were less pronounced and more related to changes in patients’ clinical characteristics. Higher mortality risk reductions were observed in women and were driven by relatively more positive changes in their baseline risk profiles when compared to men.
Conclusions:
The progress in the treatment strategies has helped to achieve better survival rates in STEMI patients. However, the ongoing changes in clinical characteristics of patients also played an important role, especially in women. Clinicians should focus on modifiable risk factors and post-discharge management to possibly prolong the positive aspects of in-hospital efforts.
The aim of this study is to estimate how much of the recent decrease in mortality among patients with myocardial infarction with ST-segment elevation (STEMI) can be attributed to improved treatment strategies, and how much it is related to changes in baseline clinical characteristics, and to compare these findings for men and women.
Material and methods:
This was a retrospective analysis of 32,790 patients with STEMI from the Polish Registry of Acute Coronary Syndromes PL-ACS hospitalised in 2005 and 2011. Changes in treatment strategies including pharmacotherapy were analysed. Observed in-hospital and 12-month mortality rates were compared with the outcomes in the groups matched on the propensity scores.
Results:
There was a substantial improvement in STEMI patient management between 2005 and 2011 in Poland. It included greater use of percutaneous coronary interventions and other guideline-based adjunctive therapies, and it was associated with a significant decline in in-hospital mortality. Relative 12-month mortality reduction rates were less pronounced and more related to changes in patients’ clinical characteristics. Higher mortality risk reductions were observed in women and were driven by relatively more positive changes in their baseline risk profiles when compared to men.
Conclusions:
The progress in the treatment strategies has helped to achieve better survival rates in STEMI patients. However, the ongoing changes in clinical characteristics of patients also played an important role, especially in women. Clinicians should focus on modifiable risk factors and post-discharge management to possibly prolong the positive aspects of in-hospital efforts.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.