Introduction
One of the most important causes of blindness is glaucoma, an age-related disease that can lead to blindness without appropriate medical treatment [1]. The visual impairment could also occur after eye surgical treatment, the risk being also related to the health status of the subject [2–4]. Filtration surgery (trabeculectomy) for glaucoma is performed whenever a maximal tolerable pharmacologic intraocular pressure (IOP) lowering therapy and/or laser surgery failed to decrease IOP in order to prevent optic nerve damage and visual field deterioration [5]. For decades, trabeculectomy has been the gold standard glaucoma filtration procedure, with a high success rate (IOP < 21 mm Hg for high-tension glaucoma and a reduction of at least 20% for normal-tension glaucoma) in most groups and glaucoma diagnoses, especially in the hands of an experimented surgeon [6]. However, this technique is associated with complications, including high IOP (27% late post-operative, > 1 month), hyphema (21% on the first postoperative day), enclosed bleb (11% post-operative, from 3 days to 1 month), scleral flap closure (10% late post-operative), choroidal detachment (5% post-operative, from 3 days to 1 month), decompression retinopathy (4%, first post-operative day) [7]. The popularity of trabeculectomy has been declining as newer options such as shunts or glaucoma devices have appeared. Ex-PRESS miniature glaucoma implant (Alcon Laboratories Inc., Fort Worth, Tx) is a biocompatible, non-valves stainless steel tube, currently implanted under a partial thickness scleral flap, as first suggested by Dahan and Carmichael [8]. Ex-PRESS miniature glaucoma diverts aqueous humor (AH) from the anterior chamber to the subconjunctival space. The Ex-Press was originally intended for direct implantation under the conjunctiva but was followed by several complications, especially conjunctival erosion [9]. Ex-Press has subsequently been modified to be placed under the scleral flap, making it similar to traditional trabeculectomy, while avoiding the need for trabecular meshwork removal and peripheral iridectomy (so less invasive), but with the price of introducing a metallic foreign body into the eye [10]. Either higher effectiveness in lowering IOP or better safety are the main reasons for implanting the Ex-PRESS mini-shunt [11]. Ex-PRESS implantation is associated with fewer complications, such as maculopathy and choroidal detachment [11–15]. Several types of Ex-Press such as R-50, T-50, X-50, P-50, X-200, and P-200 are used and proved similar efficacy as compared to standard trabeculectomy with regard to IOP decrease, and success rate [16].
Studies published since 2015 on heterogeneous types of glaucoma report similar performances in the decrease of IOP and success rate of Ex-PRESS shunt as compared to standard trabeculectomy (Table I). By contrast, in the case of neovascular glaucoma, standard trabeculectomy proved better performances as compared to Ex-PRESS. Ex-PRESS shunt interventions differ from one study to another, in terms of what and how frequently, but all patients received mitomycin C as anti-mitotic medication (Table I) [17–27].
Table I
Efficacy and/or safety of Ex-PRESS (ExP) vs. standard trabeculectomy (T)
| Author [ref.] | Study | No. of eyes ExP/T | Primary and secondary outcomes ExP/T |
|---|---|---|---|
| Moisseiev et al. [17] | 39/61 | Success rate: 84.6%/86.9% Complications: hypotony (7.7%/9.8%, p = 0.215), bleb leak (7.7%/6.5%), overfiltrating bleb (7.7%/1.6%), blebitis (0.0%/1.6%), choroidal and vitreal hemorrhage (2.5%/0.0%) | |
| Wagschal et al. [18] | 33/31 | IOP: 11.3/11.6, p = 0.81 Success rate: 57%/70%, p = 0.28 | |
| Liu et al. [19] | 16/17 | IOP: 19.53/18.2 Complete success rate: 43%/47% Qualified success rate: 75%/76.5% | |
| Gonzalez-Rodriguez et al. [20] | 32/31 | IOP: 10.3/11.1 mm Hg, p = 0.10 Complete success rate: 35%/38%, p = p p = 0.92 Further glaucoma surgery: 18.7%/12.9%, p = 0.73 Hypotony: 3.1%/0.0% | |
| Mendoza-Mendieta et al. [21] | 20/20 | IOP: 13.4/13.09 mm Hg, p = 0.627 Success: 80%/72.7%, p = 0.867 Complications: none at 12 months | |
| Dib Bustros et al. [22] | 28/28 | IOP: 15.6/13.7 mm Hg, p = 0.15 Complications (any): 7.1%/28.6%, p = 0.08 Success rate (> 30% no medication): 28.6%/35.7% | |
| Lee et al. [23] | 17/23 | IOP: 12.1/15.5 mm Hg, p = 0.212 Complete success rate: 65%/61%, p = 0.845 Laser suture lysis: 17.6%/21.7%, p = 0.537 Bleb needling procedures: 5.8%/21.7%, p = 0.216 | |
| Salvetat and Beltrame [24] | 132 | IOP: 15.0 mm Hg (1 year, n = 132), 15.5 mm Hg (2 years, n = 118), 15.9 mm Hg (3 years, n = 101), 15.6 mm Hg (4 years, n = 68) Complete success (60 months): 27% Qualified success (60 months): 68% | |
| Arimura et al. [25] | 32/32 28/25 – 2 years follow-up | Corneal endothelial cell density (ECD): 2,564/2,487 cells/mm2, p = 0.026 Light scattering intensities: 101.2/136.8 cct, p = 0.04 Complications: 3.1%/18.8%, p = 0.02 IOP: 14.7/15.0 mm Hg, p = 0.33 | |
| Tojo Notsuka and Hayashi [26] | 69/39 | IOP: 11.5/11.1 mm Hg, p = 0.612 (1 year), 10.9/13.0 mm Hg, p = 0.178 (4 years) Success rate: p = 0.570 Failure rate: 18.8%/17.9% Top three complications: choroidal detachment (15.9%/33.3%, p = 0.037), shallow anterior chamber (2.9%/7.7%, p = 0.255), hyphema (1.4%/7.7%, p = 0.099) | |
| Kawabata et al. [27] | 14/30 | Complete success rate (1 year): 25.7%/47.8% Qualified success (1 year): 31.8%/69.3%, p = 0.018 Top three complications: hyphema (21.4%/66.7%, p = 0.005), bleb leakage (14.3%/56.7%, p = 0.008), choroidal detachment (14.3%/13.3%, p = 0.932) |
Salvetat and Beltrame reported the absence of previous surgery (HR = 0.1, 95% CI: 0.0–0.9, p = 0.04), lens status = phakic (HR = 0.2, 95% CI: 0.1–0.5, p = 0.005), combined phaco + intraocular lens (HR = 3.2, 95% CI: 1.3–7.8, p = 0.001) as significant pre-operative variables for qualified success at 3-year follow-up (n = 101) [24].
To the best of our knowledge, no comparison has been conducted on Romanian patients, while most of the studies had up to 3 years’ follow-up. To fill these gaps, our study aimed to compare the 4-year efficacy in reducing the intraocular pressure and safety expressed as fewer complications of Ex-PRESS P-200 mini-shunt implantation as compared to standard trabeculectomy in patients with open-angle glaucoma.
Material and methods
Study design and outcome measurements
A single-center retrospective study on patients diagnosed with open-angle glaucoma with failed medical treatment (triple medication) and who underwent Ex-PRESS device implantation or standard trabeculectomy was conducted. The patients underwent surgery at Oculens, Cluj-Napoca, Romania. The patients were included in the study between January 2009 and December 2014, and followed up for 4 years (the last follow-up in December 2018).
Patients older than 50 years at the time of surgery, patients with cataract extraction in the past with intraocular lens (IOL) in the capsular bag and with triple medication uncontrolled primary or secondary (pseudophakic or pseudoexfoliation) open-angle glaucoma (OAG) were eligible for the study. Patients with angle-closure glaucoma or other secondary glaucoma as previously mentioned, pseudophakic patients with anterior chamber intraocular lens (AC-IOL), iris fixated or sulcus intraocular lens fixation, patients whose surgery was combined with any other procedure than cataract extraction and IOL implantation in the bag, history of retinal detachment, retinal vascular occlusion, optic neuropathy or trauma were excluded.
Medical charts were used to collect data such as baseline characteristics; the surgical records were used to collect information regarding the type of intervention, and the outpatient charts were used to collect follow-up outcomes. The number of pressure-lowering medications in use at all time points was also recorded. Patients with incomplete data in the medical charts were excluded from the analysis. Patients were divided into two groups: the T group included patients with standard trabeculectomy, and the ExP group included the patients who received the Ex-PRESS P-200 device.
All patients received prior to the intervention an ophthalmic examination including visual acuity, refraction (autorefractometer, Topcon, Japan), gonioscopy, Goldmann tonometry, fundus examination, automated perimetry (Humphrey Analyzer, Carl Zeiss Meditec, Dublin, CA, USA), coherence optical tomography (OCT) (Triton, Topcon, Japan), and measurement of central corneal thickness (CCT). The IOP measurements were recorded prior to the intervention and at 6 weeks, 1 year, 2 years, 3 years, and 4 years. IOP measurements were performed by Goldmann applanation tonometry. The following data were recorded for each follow-up: IOP, visual acuity (VA), number of medications. Early (in the first months after the surgery) and late complications (those complications that occurred after 3 months post-intervention) were also evaluated.
Interventions
The selection of the surgical procedure depended on the acceptance of the patients and their financial status. In Romania, the Ex-Press device is not covered by the Health Care Insurance, so all patients with Ex-Press intervention agreed prior to the surgery to pay 700 dollars. The study adhered to tenets of the Declaration of Helsinki. All patients signed an informed written surgery consent form before the surgery and underwent parabulbar anesthesia with xylene 2–4%.
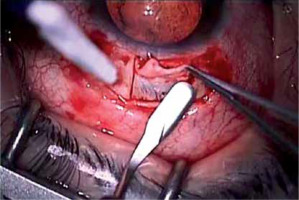
The surgical technique for trabeculectomy followed its usual steps: creation of a fornix conjunctival flap in the upper quadrants, creation of a scleral flap (4/5 mm) extending into the clear cornea, trabeculectomy, peripheral iridectomy, suturing the scleral flap with two 9.0 nylon sutures; the bleb was formed by suturing the conjunctiva using 7.0 resorbable sutures (Figure 1).
The surgical technique for Ex-PRESS intervention consisted in the creation of a fornix conjunctival flap in the upper quadrant, careful cauterization, creation of a limbal-based scleral flap extending into clear cornea (as in the traditional trabeculectomy), penetration of the anterior chamber using a 25G needle halfway between the white sclera and clear cornea (in the center of the grey zone), gently removed to avoid lateral movement that may extend the channel and cause aqueous humor to leak around the shunt and implantation of the Ex-PRESS P-200 implant preloaded on its inserter, through that pre-incision, withdrawal of the inserter, tucking the plate under the scleral flap and verification of its position. No peripheral iridectomy was required, the scleral flap was sutured with four 9.0 nylon sutures, and the bleb was formed by suturing the conjunctiva using 7.0 resorbable sutures. Ex-PRESS P-200 has a length of 2.64 mm, a decreased bevel angle, internal and external lumen diameter of 200 and 400 µm, respectively (Figure 2).
Mitomycin (0.4 mg/ml) was neither used in standard trabeculectomy nor in the Ex-PRESS implantation because of the possible corneal endothelial cell damage, postoperative long-term severe hypotony or risk for endophthalmitis.
Regardless of the type of intervention, all patients were treated with topical steroids (dexamethasone sulfate 0.1%) and antibiotics (ofloxacin 0.3%) 4 times/day for 1 month, with the cessation of all previous topical antiglaucoma therapy.
The surgical intervention was considered a complete success when there was a 20% reduction of IOP relative to the pre-operative value or IOP < 20 mm Hg without any postoperative antiglaucomatous medication. Qualified success was considered when there was a 20% reduction of IOP from the pre-operative value or IOP < 20 mm Hg with postoperative medication. The need for a second operation for glaucoma, persistent elevated IOP (> 20 mm Hg) despite medical therapy or persistent hypotony (< 5 mm Hg) was considered a failure.
The Oculens clinic’s ethical committee approved the study (no. 2/2019). Informed consent was obtained from each patient included in the study, which complied with all relevant national regulations and institutional policies and followed the Helsinki Declaration.
Statistical analysis
The eye represented the statistical unit according to the applied intervention, namely Ex-PRESS P-200 implant or trabeculectomy. Statistica program version 8 (StatSoft, USA) was used for statistical analysis. Univariate analysis was performed with the Mann-Whitney test non-parametric test since measurements proved not to follow the normal distribution (Shapiro-Wilk test), the χ2 test or Fisher’s exact test for the associations between qualitative data. P-values were considered statistically significant if less than 0.05. Friedman ANOVA test was applied to test differences in the visual acuity between follow-up measurements; the post-doc analysis was conducted whenever Friedman ANOVA proved statistically significant. Cox regression analysis was conducted to assess the risk of failure among groups with different interventions.
Results
Sixty-three patients with open-angle glaucoma age from 21 to 86 years were included in the study, and 73 eyes were evaluated (40 eyes with standard trabeculectomy and 33 eyes with Ex-Press P-200 shunt). No significant differences were observed between the investigated groups regarding the age, gender, affected eye, pre-operative IOP, and cup/disc ratio (p > 0.10, Table II).
Table II
Demographic and baseline characteristics of evaluated patients with open-angle glaucoma
| Characteristic | Ex-PRESS shunt (ExP; n = 33) | Standard trabeculectomy (T, n = 40) | Stat (p-value) |
|---|---|---|---|
| Age, median (Q1 to Q3) [years]a | 63.5 (60 to 69) | 64.5 (60.0 to 74.8) | –1.07 (0.2822) |
| Gender, n (%)b: | 0.12 (0.7278) | ||
| Female | 18 (64.3) | 21 (60.0) | |
| Male | 10 (35.7) | 14 (40.0) | |
| Affected eye, n (%)b: | 0.66 (0.4169) | ||
| Left | 18 (54.5) | 18 (45.0) | |
| Right | 15 (45.5) | 22 (55.0) | |
| Pre-operative IOP, median (Q1 to Q3) [mm Hg]a | 32 (29 to 40) | 35 (27.8 to 40.3) | –0.71 (0.4781) |
| Cup/Disc ratio median (Q1 to Q3)a | 0.8 (0.7 to 0.9) | 0.8 (0.7 to 0.9) | 1.40 (0.1625) |
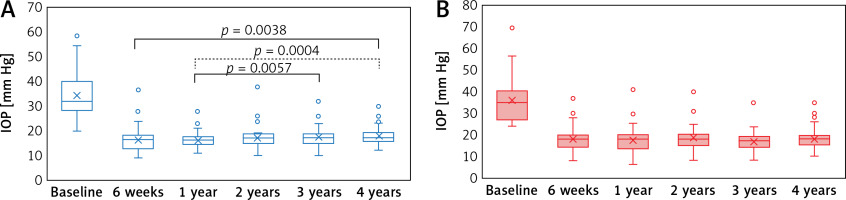
The values of IOP significantly decreased after intervention in both groups (Friedman ANOVA test: p < 0.001, ExP; p < 0.001, T; Figure 3), without significant differences between groups at any follow-up visits (Mann-Whitney test, p = 0.0838 6 weeks, p = 0.0771 1 year, p = 0.1450 2 years, p = 0.8549 3 years, p = 0.8505 4 years).
Figure 3
Variation of IOP along with time and differences between follow-up values by groups. The median values of IOP are slightly lower in Ex-PRESS P-200 shunt (ExP) group (A) as compared to standard trabeculectomy (T) group (B) for 6-week (16/18 mm Hg), 1-year (16/18 mm Hg), and 2-year (17/18 mm Hg) follow-up, identical at 3-year follow-up (17 mm Hg)
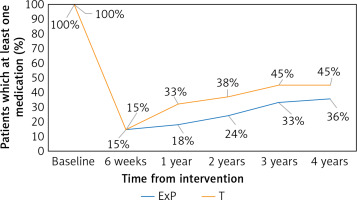
The trend in the medication proved similar for all follow-ups regardless of the intervention (Figure 4, Table III). However, no significant differences were observed when the ranks of number of anti-glaucoma drugs were compared between groups, in any of the investigated points (p-values from Mann-Whitney test: 0.7171 at baseline, 0.9470 at 6-week follow-up, 0.3873 at 1-year follow-up, 0.4313 at 2-year follow-up, 0.4510 at 3-year follow-up, and 0.5495 at 4 year-follow-up).
Table III
Post-surgery antiglaucomatous medication (β-blockers and/or carbonic anhydrase inhibitors) by follow-up and intervention
Figure 4
Trends in anti-glaucoma medication expressed as a percent of patients who received at least one drug. P-values for the association between the presence of anti-glaucoma drugs and the type of intervention were as follows: 0.9856 at 6-week follow-up, 0.1653 at 1-year follow-up, 0.2249 at 2-year follow-up, 0.3107 at 3-year follow-up, and 0.4554 at 4-year follow-up
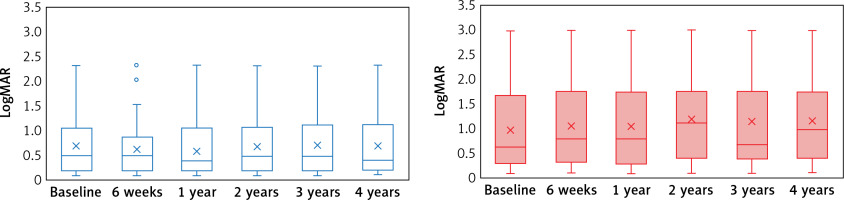
The preoperative corrected visual acuity (CDVA) expressed as logMAR (logarithm of the minimal angle of resolution) had borderline significance between groups (Mann-Whitney test: p = 0.0538). The changes in the corrected visual acuity at each follow-up are illustrated in Figure 5, with significantly better visual acuity at all follow-ups for ExP groups as compared with the T group, with the exception of 3-year follow-up when only borderline statistical significance was observed.
Figure 5
Trends in the evolution of corrected visual acuity by groups. Significantly lower values for ExP group as compared to the T groups at 6 weeks (p = 0.0324), 1 year (p = 0.0168), 2 years (p = 0.0162), and 4 years (p = 0.0111) with borderline statistical significance at 3 years (p = 0.0504) (Mann-Whitney test). The value at 4-year follow-up proved significantly higher in the T group as compared to baseline values (post-hoc analysis: p = 0.0067)
Similar results regarding the success (complete and qualified) and failure were observed between groups, with a slightly higher failure rate at 4-year follow-up in the ExP group as compared with the T group (Table IV). The hazard ratio of failure is in favor of the ExP group at 2-year follow-up with 48% higher risk for failure when the T intervention was applied, but with similar results at 6-week and 4-year follow-up (Table IV).
Table IV
Efficacy analysis: comparison (Fisher’s exact test) between interventions
The Cox regression model for failure as an outcome variable showed less risk for failure in the Ex-PRESS groups (HR = 0.72, 95% CI: 0.26–1.98, p-value = 0.523).
No significant association was observed between complications and type of intervention (Table V). No corneal decompensation or endophthalmitis was observed in the investigated sample, either in the ExP group or in the T group.
Table V
Association analysis between complications and type of intervention
| Complication | ExP group (n = 33) | T group (n = 40) | P-value |
|---|---|---|---|
| Early: | |||
| Hypotony | 7 (21.2) | 6 (15.0) | 0.4899* |
| Hypertony | 1 (3.0) | 0 (0.0) | 0.4521** |
| Total early complications | 8 (24.2) | 6 (15.0) | 0.3182* |
| Late: | |||
| Cataract | 2 (6.1) | 9 (25.5) | 0.0972** |
| Fibrosis | 1 (3.0) | 1 (2.5) | 0.9999** |
| Obstruction | 1 (3.0) | 0 (0.0) | 0.4521** |
| Total late complications | 4 (12.1) | 10 (25.0) | 0.1642* |
Discussion
The Ex-PRESS P-200 shunt implantation proved as good as standard trabeculectomy in the reduction of IOP in patients with OAG, with less risk of failure, significantly better results regarding visual acuity in favor of ExP intervention, and no significant differences regarding early and late complications.
Trabeculectomy is known as the gold standard glaucoma incisional procedure for lowering IOP in OAG. Despite its success, the standard trabeculectomy is not without risks [7], which is why surgeons search for new procedures with the same efficacy and safety, as an alternative to standard trabeculectomy.
In our study, the patients included in the groups were similar, with half of them younger than 63.5 and 64.5 years, respectively, and a predominance of women (Table II). No significant differences were observed with regard to baseline characteristics (e.g., IOP and cup/disc ratio, p > 0.10, Table II), supporting the comparison between the ExP group and T group.
Regardless of the type of intervention (Ex-PRESS or standard trabeculectomy), IOP significantly decreased after intervention in both groups (p < 0.001). The median values of IOP were slightly lower in the ExP group as compared to the T group at follow-ups points, but no significant differences between groups at any follow-up visits were observed (p > 0.08, Figure 3). Our result supports some of the previously reported results, with the same efficacy of both Ex-PRESS and standard trabeculectomy [28–33]. However, Dahan et al. [8] and de Jong [34] reported better control of IOP and a higher success rate compared to standard trabeculectomy. Liu et al. [19] showed good control of IOP with no statistical difference (p > 0.20) between the groups with Ex-PRESS implantation as compared with standard trabeculectomy at 1-year follow-up. Most frequently, the previous studies reported no significant difference in IOP reduction between Ex-PRESS and standard trabeculectomy [11, 12, 14, 17, 32, 33]. De Jong et al. [34] observed no difference in IOP after 3 years postoperatively. The studies reported by the American Academy of Ophthalmology concluded that available data are insufficient to demonstrate any superiority or inferiority of the Ex-PRESS device as compared to standard trabeculectomy [29]. At 2 years of follow-up, Omatsu et al. [35] observed a significant decrease in IOP in both groups (i.e. trabeculectomy and Ex-PRESS) compared to baseline IOP. The procedure for Ex-PRESS implantation under the sclera is almost the same as that for trabeculectomy; therefore it is not a surprise that the results of both procedures are almost the same. Gonzalez-Rodriguez et al. [20] demonstrated a reduction of IOP 3 years post-operatively of 41.1% in the Ex-PRESS group and 47.9% in the standard trabeculectomy group as compared to pre-operative IOP.
The number of post-operative anti-glaucoma drugs was similar in our sample regardless of the group (Table III), without significant differences at any follow-up (p > 0.30, Figure 4). The obtained results are similar to the results reported by other research groups. For example, Dip Bustros [19] reported a decrease in the number of medications to 0.53 ±0.80 (p < 0.001) in the Ex-PRESS group and to 0.78 ±1.13 (p < 0.01) in the group that received standard trabeculectomy. Similar results were also reported by Liu et al. [19], Tojo Notsuka and Hayashi [26], Omatsu et al. [35], Lee et al. [23], and Moisseiev et al. [17]. The absence of a significant difference regarding the number of post-operative medications after standard trabeculectomy as compared to Ex-PRESS intervention has been reported [17, 19, 25].
Fluctuation in the frequency of complete success, qualified success and failure was observed with different trends for Ex-PRESS P-200 as compared to standard trabeculectomy in the investigated sample (Table IV). A slightly higher percentage of complete success was seen in the ExP group but without significant differences between groups at different follow-up evaluations. Furthermore, a significant association was observed between the type of intervention and complete, qualified success and failure at the last follow-up (p = 0.05), with a higher percentage of complete success for those with standard trabeculectomy but a similar percent of those with complete or qualified success regardless of the type of intervention (Table V). However, the hazard ratio for failure at 4-year follow-up showed no differences between interventions. Moisseiev et al. [17] during an evaluation of 6 months showed a complete success achieved in 62.3% of cases and a qualified success in 24.6% of eyes after trabeculectomy. Among patients who underwent Ex-PRESS mini shunt implantation, complete success was achieved in 66.6% of eyes and qualified success in 17.9% [17]. Liu et al. [19] showed good control of IOP and the qualified (76.5% vs. 75%) and similar complete success rate (47% vs. 43%) at 1-year of follow-up. Similar results were also reported by Maris et al. [11], Good and Kahook [14] and Seider et al. [32]. On the other hand, Beckers et al. [36] reported a success rate of 83.3% for trabeculectomy at 1-year follow-up and a decrease to 60% at 72-month follow-up. Wilensky and Chen [37] observed the same decrease in the rate of success over time regarding trabeculectomy.
The early and late complications in the investigated sample showed a low rate of hypotony in the Ex-P group compared to the T group (Table V). This result could be explained by the fact that the Ex-PRESS P-200 was implanted using only two sutures. Similar results were reported by Liu et al. [19] with a higher rate of total complications in the Ex-PRESS group compared with the trabeculectomy group (37.5% vs. 29%). The higher percent of hypotony in the Ex-Press group was attributed to the choice of the Ex-Press P-200 model [19]. Results similar to those reported in our study were also previously published, showing the advantages of Ex-PRESS shunt regarding the reduced rate of early hypotony, a decreased rate of postoperative intraocular inflammation, and no need for peripheral iridectomy [11, 12, 14, 32, 33]. The complications observed in our sample were only hypo- and hypertony as early complications and cataracts, fibrosis and obstruction as a late complication. Moisseiev et al. [17] reported blebitis (1%), early bleb leaks (7%), overfiltrating blebs (4%), and hypotony with choroidal detachment (9%).
The evolution of corrected visual acuity showed significantly lower values for the ExP group as compared to the T group at 6 weeks (p = 0.0324), 1 year (p = 0.0168), 2 years (p = 0.0162), and 4 years (p = 0.0111) with borderline statistical significance at 3 years (p = 0.0504). The value at 4-year follow-up proved significantly higher in the T group as compared to baseline values (p < 0.007, Figure 5). Good and Kahook [14] reported an increased visual recovery following Ex-PRESS implantation with no significant differences in the visual acuity between the two groups at 1-year follow-up. Maris et al. [11] reported a loss of one or two Snellen lines in Ex-PRESS and standard trabeculectomy both groups. Our results regarding the visual acuity are similar to those reported by Liu et al. [19], and Lee et al. [23] reported the absence of changes in the corrected distance visual acuity regardless of the intervention (Ex-PRESS or standard trabeculectomy, p > 0.20). Gonzalez-Rodriguez et al. [20] reported a faster recovery of visual acuity in the Ex-PRESS group compared with trabeculectomy while Arimura et al. [25] observed no significant differences between the two groups in terms of postoperative visual acuity.
Our study, despite a rigorous methodology, had some limitations. Firstly, the retrospective collection of the data is limited by the accuracy of the medical charts, and a prospective design would permit a more accurate collection of follow-up data. Secondly, no random assignment to the intervention was applied since only the standard trabeculectomy is supported by the National Health Insurance House while the Ex-PRESS intervention is supported by the patient. Despite this limitation, the patients with standard trabeculectomy (probed similar) to those with Ex-PRESS, sustaining the validity of the observed differences. Thirdly, the present study does not offer long-term results (≥ 5 years post-intervention). A longer follow-up could adequately identify the trends in the late complications such as tube erosion or corneal complications (including an increased rate of corneal endothelial cell loss) for the Ex-PRESS implantation [25, 38, 39].
The efficacy and safety of the Ex-PRESS shunt are already known, and the low complication rate compared to standard trabeculectomy as well as good IOP control has already been demonstrated. However, the follow-up of the previous reports is up to 3 years [24–26, 40]. Moreover, all patients received anti-mitotic medication as adjuvant therapy for postoperative IOP control [24–26, 40]. The added value of our study is represented by a longer follow-up of patients with Ex-PRESS intervention without anti-mitotic medication. The evidence of the Ex-PRESS shunt efficacy at 4 years after the intervention in the absence of anti-mitotic medication provides valuable insight to support the clinical significance for the late efficacy of the Ex-PRESS shunt. Relative to the number of investigated eyes, a larger sample could comprise more heterogeneous patients and can better provide insights into this intervention. Furthermore, a longer follow-up could also be beneficial in the evaluation of late Ex-PRESS efficacy, and the expansion of the study as well as the longer follow-up is under consideration by our team.
In conclusion, 4 years of follow-up for the comparison of efficacy and safety revealed that both Ex-PRESS implantation and standard trabeculectomy are effective in the significant reduction of intra-ocular pressure. Furthermore, slightly better results are obtained by Ex-PRESS implantation on visual acuity, the number of required medications, the complete success rate in the first 3 years, less chance of hypotony, and cataract as compared to standard trabeculectomy. However, the observed differences proved not statistically different, the Ex-PRESS showing similar results with the standard trabeculectomy up to 4-year follow-up. From our point a view, both Ex-PRESS and standard trabeculectomy could be used as the first surgical option. The Ex-PRESS device could be a viable solution as a secondary procedure after failed standard trabeculectomy. The advantage of Ex-PRESS shunt is a lower rate of postoperative complications, but its limitation is the higher cost.