Recent advances in airway management led to an increasing frequency of supraglottic airway devices (SAD) being chosen instead of tracheal intubation for laparoscopic procedures. However, there are ongoing arguments regarding the use of SAD due to worries about the risks of insufficient ventilation and pulmonary aspiration [1].
The effectiveness of second-generation SAD such as Auragain, i-gel, Proseal or Supreme has been sought in laparoscopic surgery patients [2–4]. However, there has not been a single SAD advised by demonstrating clear safety in these types of procedures.
The LMA Protector (TeleflexMedical Europe Ltd., Athlone, Ireland) is a second-generation SAD that was put into use recently [5]. Due to its structure and properties, the risk of gastric aspiration is minimised [6]. It has a stable curved form and is intended for single use [7]. The first clinical trials with this device reported a high rate of success of placement in the first attempt and an adequate and reliable airway seal at the same time [8, 9].
This prospective randomised trial investigated whether the LMA Protector was comparable to tracheal tube regarding respiratory parameters. Our primary outcome was to evaluate the oropharyngeal leak pressure (OLP) values for the LMA Protector and compare the peak airway pressure between groups. The secondary outcome was to determine the Brimacombe fibreoptic visualisation scores and compare haemodynamic parameters in patients undergoing laparoscopic surgery.
METHODS
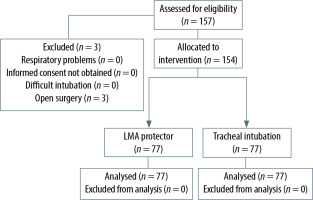
After Institutional Review Board approval from our university (IRB #2017/406) and registration at https://clinicaltrials.gov (NCT03453138), 157 adult patients with informed written consent obtained between 01.03.2018 and 01.05.2018 were enrolled in our study. Three of these were excluded due to conversion to open surgery. Patients who refused to be included in the study, patients with a history or sign of difficult intubation in their preoperative evaluation, and patients with respiratory system disorders such as chronic obstructive pulmonary disease, emphysema, or pulmonary oedema were excluded from the study. The patients were randomised to two groups: Group 1 (tracheal intubation) and Group 2 (LMA Protector). Randomisation was performed using the True Random Number Generator from www.random.org.
Neither of the groups of patients was treated with any preoperative premedications. Standard monitorisation included pulse oximetry, electro-cardiography, and non-invasive blood pressure. Anaesthesia was induced with intravenous propofol (2–3 mg kg-1), fentanyl (1–2 mg kg-1) and rocuronium bromide (0.6 mg kg-1). Achieving adequate depth of anaesthesia, the patients were either intubated, or the LMA Protector was placed. Tracheal intubation time was started as soon as the operator handled the laryngoscope until a proper end-tidal CO2 trace was observed. Tracheal tubes of 8.0–8.5 mm ID were used for male patients, whereas 7.0–7.5 mm ID tubes were used for female patients. In the LMA Protector group, the timer was started as soon as the operator handled the LMA Protector and not stopped until a proper end-tidal CO2 trace was observed. The number of attempts and success rates were recorded. The cuff pressures were maintained in the appropriate pressure range using a cuff manometer. Brimacombe image classification, which was based on visualisation of the vocal cords by a fibreoptic bronchoscope through the SAD, was made; Class 1: Vocal cords cannot be seen, Class 2: Vocal cords and anterior epiglottis can be seen, Class 3: Vocal cords and posterior epiglottis can be seen, and Class 4: Only vocal cords can be seen [10].
An intact patient airway was proven by visualisation of an appropriate end-tidal CO2 trace and a tidal volume of 6–8 mL kg-1. The following was the mechanical ventilation mode that was stan-dardised in the volume-controlled ventilation (VCV) mode: respiratory rate 12 min-1, tidal volume 6 mL kg-1, initial PEEP 5 cmH2O. If necessary, PEEP and respiration rate were modified based on end-tidal CO2. Then, the initial baseline measurements were recorded, including tidal volume, peak inspiratory pressure (PIP), OLP, mean arterial blood pressure (MAP), heart rate (HR), and peripheral oxygen saturation (SpO2). These measurements were repeated and recorded again following pneumoperitoneum and recovery from anaesthesia.
Following surgery, patients were transported to the recovery room. Patients were monitored using the Modified Aldrete Scoring System (MASS), and when they reached a score of 9 points, they were transported to the service. Postoperative recovery duration and presence of complications such as sore throat, dysphonia, and dysphagia were recorded in the recovery room. The complications were evaluated blindly by researchers who were unaware of the groups. Additionally, the number of attempts for placement of a nasogastric cannula through the gastric aspiration channel was recorded in the LMA Protector group.
Statistical analysis
IBM SPSS Statistics 22 program was used to evaluate the findings of this study. Among the numeric data, the independent samples t-test was used for those with a normal distribution, the Mann-Whitney U test was used for those that do not follow a normal distribution, the c2 test was used for discrete variables, and the Kruskal-Wallis H test was used for evaluation of time periods of cuff leakage. The results were evaluated with the 95% confidence interval and the significance level P < 0.05. The sample size was calculated based on a preliminary study of 10 patients in each group. Cuff leak at pre-extubation and cuff leak at 5 minutes were measured in patients in the LMA Protector group and were 30.50 ± 5.89 and 33.60 ± 4.79 mmHg, respectively. We determined that 50 patients in each group would be sufficient with an 80% sample size (a = 0.05, b = 0.2, and confidence interval = 95%), and the study was completed with 77 patients in each group.
RESULTS
Three patients were excluded, and the data analysis of 154 patients in total was performed (Figure 1). While 77 patients with an average age of 52.22 ± 13.90 years were intubated, the LMA Protector was used for the other 77 patients. In terms of age, body weight, height, thyromental distance, the Mallampati and American Society of Anesthesiologists (ASA) scores, the two groups were found to be similar, whereas there was a significant difference in gender distribution (Table 1).
TABLE 1
Demographic data of the groups
The duration of anaesthesia, duration of surgery, the number of attempts at inserting the airway device, and duration of the recovery period were similar between the groups. Likewise, the tidal volumes and PIPs of the groups were similar. However, the duration of airway device insertion and the incidence of sore throat were found to be significantly different between the groups (Table 2). Hoarseness was not observed in any of our patients.
TABLE 2
Perioperative data of the groups
The preoperative HR, MAP, and SpO2 values of the groups were found to be statistically similar. Although the MAP and end-tidal CO2 values were similar following the insertion of the airway device, HR and SpO2 values were significantly higher in the tracheal intubation group. Following pneumoperitoneum, MAP, SpO2, and end-tidal CO2 values were similar. However, HR was higher in the intubation group. Before extubation, HR, MAP, and SpO2 values were similar. Following extubation, although HR and SpO2 values were similar, MAP was statistically significantly higher in the intubation group (Table 3).
TABLE 3
Comparison of vital parameters between groups
Also, in the LMA Protector group, OLP mea -sures were found to be statistically similar (Table 4).
TABLE 4
Oropharyngeal leak pressure (OLP) for LMA Protector group
| Minute 0 | After pneumoperitoneum | At end of operation | P-value | |
|---|---|---|---|---|
| OLP (mmHg) | 32.88 ± 6.11 (30) | 32.73 ± 7.71 (30) | 33.65 ± 8.11 (32) | 0.682k |
The mean Brimacombe fibreoptic visualisation score was 2.12 ± 0.58 (mean ± standard deviation), and the rate of the requirement of optimisation was 15% (n = 12) in the LMA Protector group.
DISCUSSION
Among the adult patients undergoing laparoscopic cholecystectomy, insertion of the LMA Protector resulted in similar findings for ventila-tory parameters; moreover, better results were obtained than tracheal intubation regarding haemodynamic parameters.
Abdominal insufflation during laparoscopic surgery reduces respiratory system compliance. Consequently, the upshift of the diaphragm causes an increase in airway pressure [11]. On the other hand, the resistance of the respiratory system rises due to increased airway pressure. Therefore, the two most important parameters to search for the safety of supraglottic airway devices are OLP and PIP. High PIP carries the risk of barotrauma for the lungs, also causing airway leakage and gastric insufflation if it exceeds OLP [12, 13]. In our study, these values were recorded as soon as the LMA Protector was placed, following pneumoperitoneum, and prior to recovery. PIP values were not found to be significantly different when compared to tracheal intubation.
The mean PIP value not exceeding 20 mmHg, as well as comparable values with tracheal intubation, suggest that this device can be safely used during laparoscopic procedures. Moreover, mean OLP values over 30 mmHg with the LMA Protector were a supporting finding for its safety.
In a meta-analysis including 26 studies with data from a total of 2142 patients, eight SAD were evaluated; the highest OLP values were obtained prior to the pneumoperitoneum period with Ambu Aura Gain, and the highest OLP values were obtained after the pneumoperitoneum period with the i-gel group [14]. The absence of a significant difference between the values obtained before and after the pneumoperitoneum periods in our study also gives information regarding the reliable use of the LMA Protector in laparoscopic procedures.
The LMA Protector has dual gastric access and integrates “Second Seal Technology/second generation LMA” to secure the distal tip at the upper oesophageal sphincter [15]. In this way an oesophageal seal is facilitated, and the respiratory tract is isolated from the digestive tract [7]. Therefore, it becomes possible to reduce the risk of gastric content aspiration. Our findings obtained in this study regarding the OLP and PIP values were in line with current literature. The LMA Protector was recently evaluated in 300 patients undergoing laparoscopic procedures, and the mean OLP was 30.18 ± 5.88 cmH2O [16]. In another study, the OLP for the LMA Protector was more than 5 cmH2O higher than for the i-gel, where higher PIPs were also generated [17].
Because of the pressure due to tracheal cuff insufflation, sore throat and hoarseness may occur in the postoperative period of laparoscopic procedures [18, 19]. In our study, two patients in the LMA Protector group developed a sore throat, whereas this number increased to 12 in the tracheal intubation group. This finding indicated that, when compared with a tracheal tube, the LMA Protector applied less trauma to the vocal cords and trachea and caused less pressure injury on the pharynx. Vocal cord and trachea irritation is expected to be less with supraglottic airway devices due to their placement superior to the larynx. In a review that included 29 randomised prospective studies, the incidence rates of laryngospasm and cough were reported to be increased in the group of tracheal intubated patients undergoing laparoscopic surgery [20]. Moreover, in a meta-analysis including 1433 patients from 17 studies, the rate of successful insertion on the first attempt and the duration of device insertion were not found to be different between tracheal intubation and SAD groups [21].
Due to the increased risk of aspiration of the gastric contents during the pneumoperitoneum period, emptying the stomach with a nasogastric tube is important for patients who undergo laparoscopic surgical interventions [22]. In this study, insertion of a nasogastric tube was mostly possible on the first attempt through the side channel of the LMA Protector.
Haemodynamic changes cause additional risks for the patient during intubation and extubation. Although the basal haemodynamic parameters were similar between the groups in our study, among the haemodynamic values, HR and MAP values were found to be higher in the tracheal intubation group than the LMA Protector group. Both laryngoscopy and tracheal intubation provide noxious stimuli leading to an adrenergic response [23]. Moreover, the receptors located in the upper airway are stimulated during the extubation as in laryngoscopy [24]. This was cited as one of the advantages of the LMA Protector tube.
According to the comparison of ventilation parameters, tidal volume, peak airway pressure, and the number of attempts for insertion were similar. This result may prove that the LMA Protector is as safe and useful as the tracheal tube to obtain an intact airway during laparoscopic surgery.
LIMITATIONS
The main limitation of this study is that, due to the structural properties of the LMA Protector, some parameters could not be compared with tracheal intubation. Therefore, fibreoptic visualisation score, ease of nasogastric insertion, and OLP were recorded as parameters related to the LMA Protector.
Another limitation of our study is the uneven gender distribution, which we believe is due to the fact that gallbladder diseases are more common in women [25]. While the postoperative evaluations were blinded, the practitioners and observers who recorded the intraoperative data were not blind due to the nature of this study.