INTRODUCTION
Upper gastrointestinal bleeding (UGIB) is a common reason for hospital admission. It is estimated to account for 300,000 admissions per year in the USA, with 23–34% admitted to an intensive care unit (ICU) for further management [1]. It remains one of the most common medical emergencies with an average mortality rate around 10% [2].
A number of risk assessment scoring systems are used in UGIBs to predict a variety of clinical endpoints such as mortality, need for intervention, risk of rebleeding and length of stay. The most widely used of these are the Glasgow-Blatchford Score (GBS), pre-Rockall score (PRS), complete Rockall score (CRS) and AIMS65 [3–5]. The ABC score is a relatively new scoring system that has been validated to predict mortality in both upper and lower GI bleeding and its purpose is to be used as a pre-endoscopy score to identify low and high risk patients [6].
While these scoring systems were originally validated for a particular clinical endpoint such as need for intervention in the case of GBS, risk of rebleeding in Rockall or inpatient mortality in the case of AIMS65, subsequent studies have evaluated the role of these scoring systems in predicting various other clinical outcomes [7–13]. However, none of these studies has focused exclusively on UGIB patients admitted to an ICU. A recent poster in the journal Gut demonstrated a superior predictive value of AIM65 when compared with GBS and PRS in predicting ICU admission; however, this study did not look at ICU mortality specifically [14].
In this single-centre retrospective study of UGIB patients admitted to the ICU, we compared the ability of four risk assessment scores to predict mortality and length of stay. We then compared their performance to that of two established critical illness severity of illness scores, APACHE II and SOFA [15–18].
METHODS
This was a single-centre retrospective study undertaken at St James’s Hospital (SJH), Dublin. The clinical endpoints were ICU and hospital mortality as well as ICU length of stay (LoS) longer than seven days. Patients were included if they presented to the ICU with evidence of upper gastrointestinal bleeding defined by haematemesis, coffee-ground vomiting, or melaena. We excluded patients who developed upper gastrointestinal bleeding while an inpatient for another reason. This research was approved by the department of research and innovation at St James’s Hospital.
Data collection
Data were collected for all patients attending the ICU in SJH between October 2018 and September 2020. A search of the hospital in-patient enquiry (HIPE) was conducted to collect the list of patients. The HIPE system is the principal source of demographic, clinical and administrative information from publicly funded acute hospitals in Ireland and is managed by the national Healthcare Pricing Office (HPO). The electronic patient record (EPR) for each patient was used to collect data including patient characteristics as well as haemodynamic and laboratory variables at presentation necessary to calculate the GBS, PRS, CRS, AIMS65, ABC, APACHE II, and SOFA scores. The hospital length of stay was recorded. The majority of data collected for this study were primary. However, secondary data included the APACHE II and SOFA scores, which are calculated on admission to the ICU for all patients and were therefore included in the data provided by the ICU audit nurses.
Statistical analysis
We compared the scores’ ability to predict mortality and LOS using calculation of area under the receiver operating scores (AUROC) and 95% confidence intervals. All comparisons were based on patients in whom all the compared scores could be calculated. Data analysis was undertaken using SPSS.
RESULTS
Patient characteristics and baseline scores
A total of 44 patients were included in the study. The median age was 67 with a range of 28 to 97. 26 (59%) were male and 18 (41%) were female.
Endoscopic treatment was performed in 37 patients (84%), 3 (7%) required IR embolization, and 4 (9%) died prior to endoscopy. Table 1 outlines the endoscopic findings, with the commonest cause for bleeding being peptic ulcer disease, which accounted for more than one third (n = 19) of patients, and the second most common being variceal bleeding (n = 7).
TABLE 1
Source of upper gastrointestinal bleeding (n = 44)
The median length of stay in the ICU was 10.6 days. In total, 10 (22.7%) died while in the ICU and a further 7 patients died after being transferred to the ward. Total inpatient mortality was 17/44 patients (38.6%).
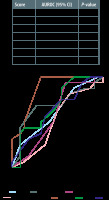
Mortality in ICU
The APACHE II score had the best discriminate value in predicting mortality in the ICU with an AUROC of 0.87 (95% CI: 0.75–0.99; P = 0.003) while the SOFA score had a reasonable predictive ability with an AUROC of 0.71 (95% CI: 0.50–0.93; P = 0.08). The UGIB scoring systems had poor predictive value with AUROCs ranging from 0.52 to 0.66 (Figure 1).
Mortality in hospital
The APACHE II score was also the best scoring system in predicting mortality for the whole inpatient episode with an AUROC of 0.87 (95% CI: 0.76–0.98; P < 0.01) while the other scoring systems had poor discriminative value, with AUROCs of 0.52–0.69, as outlined in the table in Figure 2.
ICU length of stay
All scoring systems had poor discriminative value in predicting ICU LoS of more than seven days. The AUROCs were 0.56 for GBS, 0.67 for PRS, 0.55 for CRS, 0.71 for AIMS65, 0.63 for ABC, 0.58 for APACHE II, and 0.61 for SOFA (Figure 3).
DISCUSSION
Mortality
This small study of ICU patients with UGIB yielded some interesting albeit expected results. Although scores for AIMS65, GBS, ABC, PRS and CRS have been shown to have high predictive value for mortality in hospital patients with UGIB, this small study shows that among the ICU cohort of patients, these scoring systems fail to demonstrate this same predictive value. Two papers in the last year have given the edge to AIM65 in predicting mortality for these scoring systems. For example, a study of 463 patients by Ak et al. [19] demonstrated an AUROC of 0.71 for AIM65 in predicting mortality in hospital patients compared with an AUROC of 0.54 for the GBS. Another study in 2021 also showed an increased predictive value of AIM65 for mortality compared with GBS and CRS [20].
Unsurprisingly, APACHE II had the best predictive value of mortality and to a lesser extent the SOFA score. APACHE II was primarily designed to predict mortality in ICU patients and therefore we expected it to perform well, as it incorporates multiple parameters specific to ICU patients such as organ failure as well as background medical history and chronic illness, all of which contribute to mortality. The SOFA score, while originally designed to describe a sequence of complications of critical illness and not to predict outcome, has ultimately been shown to be a predictor of mortality and it incorporates six different organ systems into its score. The UGIB scoring systems on the other hand were mostly designed to predict clinical endpoints other than mortality. For example, the GBS was primarily designed for risk stratification in order to determine need for intervention while the Rockall score was designed to assess rebleeding risk in these patients. While the UGIB scoring systems evaluated in this study have ultimately been shown in prior studies to predict mortality in hospital patients, ICU patients are a much more selective cohort and the results of this study demonstrate that only specific critical care scoring systems were accurate in predicting mortality for these patients. This is most likely due to the fact that they incorporate other parameters specific to ICU patients, particularly organ failure.
Length of stay
AIMS65 is the only scoring system so far which has been shown to predict hospital length of stay [5]. Although our study demonstrated that AIMS65 was the best predictor among the scoring systems, this did not come close to the 0.8 threshold in AUROC analysis. The other scoring systems showed no discriminative value in predicting ICU length of stay. Larger studies looking at all hospital patient cohorts also failed to demonstrate a predictive value of UGIB scoring systems in determining hospital length of stay [13]. For the ICU scoring systems, our results are in keeping with other small studies which have assessed the predictive value of APACHE II and SOFA with length of stay [21–23].
CONCLUSIONS
In this small cohort study, we were unable to demonstrate discriminative value for any of the UGIB scoring systems to predict mortality or length of stay in ICU patients. This study supports the validation of APACHE II as a clinical tool for predicting mortality in ICU patients with UGIB.