Introduction
The use of preoperative localization using computed tomography (CT) for guiding wedge resection (WR) of lung nodules (LNs) under video-assisted thoracoscopic surgery (VATS) has been described [1–3]. Other methods of localization include the use of coils, hook-wire, radio-labeling, and a variety of liquid materials [4–6]. Each material has its specific benefits and disadvantages. However, whichever material is used, LNs that are blocked by bone are difficult to localize. When faced with bone-blocked LNs, the pathway of the needle requires adjustment to avoid the bone structures. However, if the target LNs are blocked by the scapula, it is difficult to find an alternative pathway due to the size of the scapula.
Some researchers have used a trans-scapular approach for scapula-blocked lung lesions [7–9]. This approach is also convenient when used with CT-guided localization for scapula-blocked LNs (SBLNs) [10].
Recently, a novel use of a Sens-cure needle (SCN) (Senscure pulmonary nodule localization needle (Ningbo Senscure Biotechnology Co., Ltd.) China has been proposed. This is based on the previously described hook-wire technique [11]. However, the effectiveness of SCN localization for SBLNs is still unclear.
Aim
The feasibility, safety, and effectiveness of preoperative CT-guided SCN localization for SBLNs were evaluated.
Material and methods
This was a retrospective single-center study and was approved by our Institutional Review Board. Due to the retrospective nature of the study, the requirement of written informed consent was waived.
Study design
One hundred and eighty patients with LNs who had undergone CT-guided SCN localization before VATS were enrolled from January 2018 to December 2021. Ten (5.6%) of these patients had SBLNs and localization was performed using the trans-scapular approach.
The inclusion criteria were: (a) SBLNs observed on CT; (b) SBLNs with diameters ≤ 15 mm; (c) an SBLN-pleura distance ≤ 20 mm; (d) LNs with an intermediate-to-high risk of malignancy, determined by clinical and radiological findings [12].
The exclusion criteria were: (a) SBLNs with diameters < 5 mm; (b) SBLNs that could be localized without using the trans-scapular approach; (c) calcified SBLNs; (d) the presence of active bleeding, abnormal coagulation, or limited cardiopulmonary reserve.
The SBLNs were assessed by chest CT (120 kV, 100–200 mAs, 1–1.25 mm thickness). The sizes of the SBLNs were measured by the maximal transverse diameter. SBLNs were classified into solid nodules, ground-glass nodules (GGNs), and mixed GGNs. The risk of malignancy was assessed using previously published guidelines for LNs detected by CT [12, 13].
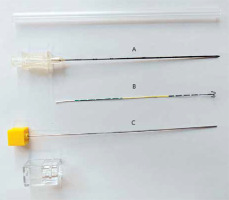
SCN device
The diameter of the SCN (Jiekang, Ningbo, China, Photo 1) was 19G with a length of 100 or 150 mm. The SCN comprised four sections, namely, the coaxial needle, pusher, anchor claw, and suture.
CT-guided trans-scapular SCN localization
The procedures were performed under local anesthesia with a 16-row CT (Philips, Cleveland, OH, USA). CT was performed before the procedure to determine the pathway of the needle (Photo 2 A). The scapula was punctured using a 17G introducer needle (DuoSmart, Modena, Italy). When the needle made contact with the bone, the puncture was completed using a drill with steady pressure. The thoracic cavity was not penetrated during the procedure (Photo 2 B).
Photo 2
The procedures of CT-guided SCN localization for SBLN (arrow) via the trans-scapula approach. A – CT image showing an SBLN at the left upper lobe. B – The scapula was punctured under CT guidance. C – The tip (long arrow) of the SCN was moved near the nodule (short arrow). D – The anchor claw (arrow) of the SCN was released near the SBLN. E – The marked line (arrow) was detected during the VATS procedure
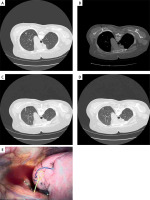
Once the 17G introducer needle was through the scapula, the 19G SCN was introduced and smoothly pushed until it reached a distance of approximately 5 mm from the LN (Photo 2 C). After removal of the release buckle, the pusher was further extended to reach the marked line. After the release of the anchor claw close to the LN (Photo 2 D), the pusher was removed before retraction of the tip to a point between the lung and the thoracic wall. The pusher was then reintroduced into the needle, forcing the tri-color suture from the needle, and both the pusher and the needle were withdrawn.
Postoperative CT was conducted to verify the position of the SCN claw and to determine any issues associated with its localization.
VATS procedures
The VATS resection was conducted within 24 h of the localization under general anesthesia. A single 3–5 cm incision was made in the chest wall. WR was performed according to the visualization of the marked line (Photo 2 E). The range of WR was at least 2 cm from the localization area on the lung. A rapid intra-operative pathological analysis of the resected LN was performed and, if there was evidence of invasive adenocarcinoma, lobectomy and lymph node resection were undertaken.
Endpoints
The technical success of the localization was set as the primary endpoint while the secondary endpoints were the time taken for localization, complications, the technical success of the WR, types of surgery used, blood loss, and the final diagnosis.
The technical success of the SCN localization was defined as the visualization of the marked line without dislodgement [14], while the technical success of the WR was defined as the confirmation of the targeted LN in the resected tissue.
Results
Patients
The study included 10 patients with 10 SBLNs (Table I). The patients included three men and seven women with an average age of 49.6 ±8.6 years. The average diameter of the 10 SBLNs was 7.7 ±1.3 mm with the average lesion-pleura distance of 6.8 ±5.0 mm. There were 2 solid nodules and 8 GGNs.
Trans-scapular SCN localization
The technical success rate of the scapular puncture was 100%. There were no complications associated with the scapula. The technical success rate of SCN localization was also 100% (Table II). The average duration of SCN localization was 12.5 ±4.0 min. One (10%) patient experienced pneumothorax after localization. There was no incidence of lung hemorrhage.
Table II
Details of CT-guided localization, VATS procedures, and final diagnoses
VATS
The WR technical success rate was 100% (Table II). Three patients were diagnosed with invasive adenocarcinoma and underwent additional lobectomy. The average duration of the VATS procedure was 97.0 ±56.0 min with an average blood loss of 44.0 ±35.0 ml. The final diagnoses of the 10 SBLNs are shown in Table II.
Discussion
The current study investigated and verified the feasibility, safety, and effectiveness of CT-guided SCN localization for SBLNs using a trans-scapular approach. The results were positive. All the SBLNs were successfully localized with a low rate of pneumothorax. These findings indicated that trans-scapular SCN localization is both effective and safe for localizing SBLNs.
The trans-scapular SCN localization comprised two procedures, namely, the scapula and lung punctures. Scapular puncture is feasible as the bone is relatively thin. In most cases, bones should be avoided and alternative routes used when performing lung interventions. However, in contrast to other types of lung intervention, such as ablation or biopsy, CT-guided SBLN localization requires the shortest possible lesion-pleural needle pathway to guarantee the success of VATS-guided WR [15]. Thus, the trans-scapular approach may be preferred for SBLN [10, 16].
Some researchers have used CT-guided coil localization for SBLNs with the trans-scapular approach [10, 16]. However, coil localization requires significant technical skill as part of the coil is localized in the lung parenchyma while the remaining section remains on the lung surface [17]. Compared with coil localization, SCN localization is simpler as the SCN is linear [14] and, compared with the hook-wire, the SCN is less rigid as part of the SCN is formed by the suture. Because of this feature, the SCN may have a lower rate of complications than the hook-wire. Here, pneumothorax occurred in only 10% of cases, lower than the rates (18.9–33.8%) reported in studies using hook-wire localization [18–20].
None of the patients in this study experienced lung hemorrhage after SCN localization. This may be the consequence of, firstly, the small sample size and, secondly, the relatively short nodule-pleura distance of only 6.8 mm. Localization of sub-pleural LNs may also reduce the incidence of lung hemorrhage.
Here, the VATS-guided WR was found to be 100% successful. This finding indicated that the use of preoperative CT-guided SCN localization results in a high WR success rate while also preserving maximal lung function and is also consistent with the findings of previous studies on CT-guided localization of LNs in normal positions [2, 14, 17]. The success of the WR is thus dependent on the successful localization of the LNs, regardless of their position.
This study had some limitations. First, the major limitation was being a retrospective study from a single center, leading to a higher risk of selection bias. Second, the sample size was limited due to the rarity of SBLNs. Third, the study did not include a control group and we were unable to compare SCN localization with other localization methods. Randomized controlled trials should be undertaken in the future.