Introduction
Coronary computed tomography angiography (CCTA) has been well validated as a non-invasive tool for the evaluation of coronary artery disease (CAD) with high sensitivity and negative predictive value [1,2]. However, the accuracy of CCTA to assess coronary luminal stenosis is typically reduced in the case of moderately to severely calcified coronary lesions [3,4].
On the other hand, CCTA is valuable for the characteri-zation of moderately and heavily calcified coronary lesions to predict the use of rotational atherectomy before percutaneous coronary intervention (PCI) or stent implantation [5].
The CAD Reporting and Data System (CAD-RADS) is a new collaborative standardized reporting effort of various societies. It is an attempt to decrease the variability among computed tomography (CT) readers, enhance the communication between the referring and interpreting physician, and facilitate uniform recommendations for further management. However, it has some limitations [6]. One of the important challenges is quantifying luminal stenosis with the densely calcified lesion, which usually causes overestimation of stenosis due to the blooming and beam-hardening artifacts [7].
Therefore, we assessed a group of quantitative CCTA parameters of moderately and severely calcified coronary lesions diagnosed as moderately (50-69% diameter stenosis) and severely stenosed lesions (70-99% diameter stenosis) by invasive coronary angiography (ICA). We investigated the cut-off values of these quantitative parameters with the highest accuracy to differentiate between moderate and severe stenosis, which will help to designate CAD-RADS 3 and 4 in the future.
Material and methods
Patients
Eighty-four patients with 150 calcified coronary lesions, who underwent CCTA and ICA with one-month intervals, were included retrospectively in our study. The inclusion criteria of the study lesions were [1] moderately (calcification arc angle [CAA] = 90-179°) or severely (CAA = 180-360°) calcified coronary lesions on CCTA, and [2] ICA-diagnosed cases as moderately stenosed (50-69%) or severely stenosed (70-99%) lesions. We excluded the following lesions from our study: ICA-diagnosed lesions as mildly stenosed lesions or occluded lesions, vessel segments of diameter < 1.5 mm, tortuous vessel segments, distal vessel segments, vessel segments distal to occlusion, stenotic lesions due to mixed plaques. Also, we excluded cases with prior coronary arteries bypass surgery (CABG) and patients with renal dysfunction glomerular filtration rate (GFR) < 45 ml/min. Each patient gave written informed consent. Institutional Ethics Committee approval was obtained for the study.
Method
CT Image acquisition CT was performed on a multidetector CT scanner (Philips Ingenuity Core 128, Philips Healthcare, Netherlands). Patients with heart rate > 65 bpm were given oral β-blockers (25-75 mg metoprolol) before the examination. Before CCTA, coronary artery calcium scoring (CAC) was performed with prospective electrocardiography (ECG)-triggered 3-mm-thickness axial slices in the diastolic phase without overlapping or gaps on the cardiac region using a medium-sharp convolution Kernel. All patients received an intravenous bolus dose of 80 to 120 cc of contrast agent (Iodixanol 350 mg iodine/ml) according to each patient’s weight and scan time. The contrast flow rate was 5 ml/s. Contrast injection was followed by a 40 cc saline bolus. A bolus tracking technique was used to trigger scanning with the proper time delay (100 Hounsfield unit [HU] threshold in ascending aorta ROI, and 4 s after the peak). Prospectively, ECG-triggered CCTA was performed with detector collimation of 64 × 0.625 mm with a z-flying focal spot, rotation time of 300 ms, temporal resolution of 150 ms, and reconstructed slice interval of 0.5 mm. The tube current was modified automatically with the patient-specific size and attenuation of the body region via the CARE dose system. The ECG-dependant dose modulation technique with full current dose was applied in the R-R interval of 40-70%. The tube voltage was adjusted to 100 kV for patients having body mass index (BMI) < 26 kg/m2 and 120 kV for those having BMI > 26 kg/m2.
Computed tomography image reconstruction
Images were post-processed on a dedicated workstation (IntelliSpace Portal V5, Philips Healthcare). We calculated the segmental coronary calcium score (SCCS) and the segmental calcium volume (SCV) on CAC scoring. According to the Agatston method [8], calcification is considered if its area is > 1 mm2 and the peak CT number (CTN) is > 130 HU. We determined the SCCS by multiplying the calcification area by the peak CTN for each included calcified coronary lesion. The SCV also was calculated automatically for each included calcified lesion.
From CCTA, axial images were reconstructed with 0.6 mm slice thickness and an increment of 0.5 mm using a medium-sharp kernel. The coronary vessels were then evaluated on curved planar reformations (CPR), interactive oblique multiplane reformations (MPR), and cross-sectional planes.
The calcified lesion length (LL) was measured on each lesion’s best long-axis plane from its proximal to distal end. On coronary vessel cross-sectional images we calculated the CT-diameter stenosis percentage (CT-DS %), calcification remodelling index (CRI), and calcification arc angle, as shown in (Figure 1), using the following formula:
CT-DS% = normal proximal/distal reference diameter
– vessel diameter at the most severely stenosed point.
Figure 1
Coronary computed tomography angiography-derived measurements of a severely stenosed calcified left anterior descending artery (LAD) lesion. Axial oblique maximal intensity projection (MIP) (A). Axial oblique MIP with coloured plaque characterization (B). CT-calcium scoring (C). LAD-cross sectional multiplanar reformates (MPR) (D-G). LAD-curved MPR (H). Invasive coronary angiography (ICA) cranial left anterior oblique (LAO) view. ICA shows proximal LAD severely stenosed lesion appears as a heavily calcified lesion on CCTA (F). Image illustrates calcification arc angle (CAA) measurements (E and G). Images demonstrate the calculation of calcification remodelling index (CRI). SCS – segmental calcium score, AU – Agatston units, SCV – segmental calcium volume

The normal vessel reference was selected manually. CRI was calculated as the luminal cross-sectional area ratio at the most severely calcified site (including the calcium) to that of the proximal reference. CAA was measured as the central angle subtended by the calcification arc in the cross-sectional plane.
Invasive coronary angiography
ICA was performed within a 30-day interval from CCTA via femoral access using conventional techniques on our fluoroscopy unit (Axiom, Siemens Medical Systems). The main coronary vessels were displayed in the multiple standard projections. An expert interventional cardiologist blindly and independently estimated the stenosis extent semi-automatically. A coronary lesion of ≥ 70% luminal diameter narrowing was defined as severe stenosis, while moderate stenosis was defined for the lesions of 50-69% diameter reduction.
Statistical analysis
Data were analysed using Statistical Package for the Social Sciences software version 26 (SPSS, Inc., Chicago, IL, USA). The Shapiro-Wilk test was used to assess normality of distribution of data. Data were presented as median and interquartile range (IQR). The Mann-Whitney test was used to compare the 2 groups (moderate and severe stenosis) with quantitative nonparametric data. Univariate and multivariate logistic regression was used to detect predictors of stenosis extent. The sensitivity and specificity of CT-DS, CRI, SCS, SCV, CL, and CAA to differentiate between moderate and severe stenosis groups were examined at different cut-off points using receiver operating characteristic (ROC) curve analysis to determine the best cut-off point as well as the diagnostic power of each test. P-values less than 0.05 were considered statistically significant.
Results
A total of 84 patients with 150 calcified coronary lesions were included in the present study; 99 (66%) were ICA-diagnosed as moderately stenosed lesions, and 51 (34%) were severely stenosed. The study population included 58 men (69%), mean age: 70.6 ± 8.3 years, mean BMI: 28.5 ± 5.4 kg/m2. Table 1 summarizes the detailed clinical characteristics of the study populations. Most of the included coronary lesions involved the left anterior descending (LAD) artery, and the proximal vessel segments were involved more than the middle vessel segments.
Table 1
Study demographic and clinical characteristics
As shown in Table 2, and Figure 2, severe coronary stenotic lesions (≥ 70% luminal stenosis by ICA) displayed significantly larger CT-DS%, SCS, SCV, and CL as well as smaller CRI. CAA was larger with severely stenotic lesions, but not statistically significantly.
Table 2
Coronary computed tomography angiography – parameters of severe versus moderate stenosis
Figure 2
Box plot of coronary computed tomography angiography (CCTA)-derived parameters in moderate stenosis versus severe stenosis. *Significance < 0.05

Table 3 shows the results of univariate and multivariate regression analysis of CCTA-derived quantitative data in both ICA-based stenosis degrees. As regards the univariate analysis, CRI was significantly lower in severely stenosed calcified coronary lesions, while the remaining CT-derived quantitative parameters were significantly higher in severely stenosed coronary lesions. In multivariate regression analysis, CRI was the only independent determinate of ICA-diagnosed stenosis degree (p < 0.001).
Table 3
Univariate and multivariate analysis of coronary computed tomography angiography (CCTA) parameters in severe coronary stenosis versus moderate stenosis
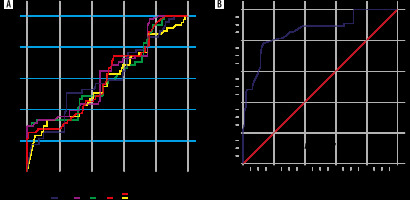
ROC analysis and the diagnostic performance of CTA-derived parameters to predict ICA-diagnosed, severely stenosed, calcified coronary lesions are displayed in Table 4 and Figure 3. The highest diagnostic performance appertained to CRI with an area under the curve and 95% confidence interval (AUC [95% CI]) of 0.857 (0.79-0.91). CRI ≤ 0.84 had the highest sensitivity (77.78%) and specificity (86.46%).
Table 4
Performance of coronary computed tomography angiography (CCTA) parameters in discrimination of severe coronary stenosis
Discussion
Many previous studies investigated the diagnostic accuracy of CCTA in the evaluation of coronary stenosis extent caused by calcified plaques [3,4,9-11]. Blooming artifacts have always been the supposed main hindering factor of accurate assessment of the vessel stenosis [12].
The accurate prediction of severe coronary stenosis in moderately to severely calcified coronary lesions is still challenging. In their study, Qi et al. concluded that CCTA showed higher diagnostic accuracy for coronary artery stenosis when the ratio of calcium plaque volume to the vessel circumference (RVTC) was ≤ 50%, while it displayed significantly decreased accuracy with larger RVTC [4]. Krub et al. stated in their study that a mean lumen diameter of ≤ 2.8 mm along with a total calcium arc of ≥ 47° predict the lumen underestimation by CCTA [11]. We included in our study moderately and severely calcified coronary lesions having CAA ≥ 90°.
Few studies have investigated quantitative CCTA parameters that could predict the extent of stenosis with the calcified coronary lesions [13]. We investigated different quantitative CCTA parameters measured in ICA-diagnosed moderately (50-69%) versus severely (70-99%) stenosed coronary lesions.
The CAD-RADS terminology was first introduced in 2016 by Cury et al. as the first scoring system facilitating standardized CAD classification with the potential to improve contact between referring physicians and CCTA imagers [14]. Since then, the score’s widespread endorsement has not been established and is still in an early phase of implementation into routine daily clinical practice [15]. CAD-RADS requires CCTA-derived information about the stenosis extent. In an attempt to get quantitative predictors of the stenosis extent, i.e. moderate stenosis (corresponding to CAD-RADS 3) versus severe stenosis (corresponding to CAD-RADS 4) in moderately and severely calcified coronary lesions, we analysed some CCTA-derived quantitative parameters.
In the current study, ICA-diagnosed severe coronary stenosis caused by calcified plaques was significantly associated with smaller CRI than moderate coronary stenosis, while CT-DS%, SCS, SCV, and CL were significantly larger in severe stenosis. Among all CT-derived quantitative parameters, CRI was the only statistically significant independent predictor of severe stenosis. CRI ≤ 0.84 was the best cut-off value predicting severe coronary stenosis, with 77.78% sensitivity, 86.46% specificity, and AUC (95% CI) 0.857 (0.79-0.91). Yu et al. reported similar results, but they reported a larger cut-off value (≤ 0.94). We thought that this difference could be due to the inclusion of mildly stenosed lesions (< 50%) in their study, in contrast to our research, including only more than moderately stenosed lesions [13].
Previously a reasonable explanation was reported of inversely correlated stenosis extent with CRI: it was suggested that calcified coronary lesions with negative remodelling (small CRI) could have intimal locations with more encroachment on the lumen with a subsequently greater degree of stenosis [5,13].
The study limitation was that we did not perform the fractional flow reserve (FFR) for most of the lesions to determine the lesions’ haemodynamic significance. However, the study strength was that the inclusion criteria were remarkably selective, allowing optimization of the study sample’s homogeneity, reduction of confounding, and increased probability of getting a real association between the study variables.
As a clinical implementation of our study, CRI may help to estimate severe versus moderate stenosis in coronary lesions with moderate to severe calcification at the current stage. Therefore, it can help to assign calcified coronary lesions CAD-RADS 4 versus CAD-RADS 3.