Introduction
Nowadays, cardiac surgery still deals with the problem of excessive postoperative bleeding. The consequences of bleeding after surgery can be dramatic, so new methods to diminish bleeding are constantly tested. Aortic valve replacement is the most widely used surgical procedure for aortic valve disease. Although the risk of death is low (3.1% (2.3–4.2%)) the risk of re-exploration for bleeding is high (5.1% (2.5–12%)) according to a meta-analysis [1, 2]. Heparin, extracorporeal circulation usage with its consequences, and hypothermia contribute to dysfunctional coagulation. Local hemostatics can be helpful, especially when the surgeon must deal with bleeding from the suture line or tissue bleeding. Our study aimed to assess the efficacy of a local hemostatic, consisting of human thrombin and fibrinogen, which was applied on the aortotomy suture line.
Material and methods
The study involved 93 patients undergoing elective aortic valve replacement. The procedures were conducted as follows: propofol, fentanyl and rocuronium were used for general anesthesia, median sternotomy, and two-stage right atrial and ascending aortic cannulation; all procedures were performed in normothermia. Three surgeons were involved in this project. Patients were randomized to one of two groups. The first group comprised 41 patients, in whom a hemostatic patch was used additionally. A local hemostatic, composed of a double collagen layer coated with human thrombin and fibrinogen (Tachosil), was applied on the aortotomy suture line and aortic cannulation site. The second group comprised 52 patients in whom Tachosil was not applied. All patients were taking aspirin 75 mg daily; low molecular weight heparin if necessary was canceled 12 h before surgery.
Both groups were comparable regarding age, morphology and coagulation parameters (Table I). In the Tachosil-treated group the fibrinogen concentration was higher, and preoperatively there were more often pleural and pericardial effusions observed. Patients from the Tachosil group suffered from pulmonological disorders more often, but there were fewer patients with chronic renal disease and diabetes.
Table I
Preoperative characteristics
[i] Hct – hematocrit, Hb – hemoglobin, RBC – red blood count, EF – ejection fraction, LVDd – left ventricle diastolic diameter, LVSd – left ventricle systolic diameter, PWs – posterior wall thickness in systole, PWd – diastolic posterior wall thickness, Ao – ascending aorta diameter, DM – diabetes mellitus, AH – arterial hypertension, AF – atrial fibrillation, APTT – activated partial thromboplastin time, PLT – platelets.
We assessed morphological parameters on the 2nd and 4th postoperative days in both groups (Table II). Besides the total drainage after 24 and 48 h, the number of rethoracotomies and postoperative pleural and pericardial effusions was assessed. The two time points of drainage assessment (24 and 48 h) resulted from the study design, but of course for clinical reasons, e.g. the decision of rethoracotomy, we followed hourly drainage and patients’ state. The total number of blood product transfusions and the additional usage of protamine and tranexamic acid were also evaluated. We evaluated patients in the postoperative period, and this included mechanical ventilation time, intensive care unit (ICU) stay and hospitalization time. Postoperative renal injury prevalence and mortality in the early postoperative period were assessed. All parameters before and after procedures are presented in Tables I and II.
Table II
All parameters in both groups after surgery
Number of Trial: RNN/229/13/KE 16.07.2013 with acceptance by local ethical committee. Patients have signed a consent form for participating in this study.
Statistical analysis
The choice of the statistical test depends on data distribution. In case of normal data distribution parametric tests can be used; otherwise one is forced to apply a nonparametric test. Observing histograms performed for analyzed variables, we could not assume normality of the data distribution. That is why for comparing two groups we decided to apply the Mann-Whitney test, which is a nonparametric one.
We also investigated the dependence between one result variable (volume of drainage 48 h) and three explanatory variables (red blood cell concentrate (RBCC) volume, hemoglobin (Hb) level on day 4, level of erythrocytes (RBC) on day 4), separately for each of the two groups. As a model for this dependence one could use linear regression. However, this model also requires normality of data distribution, but this condition was not satisfied in the case of our data. For this reason we decided to use the nonparametric model of the regression based on the k nearest neighbor rule (k-NN rule). It operates in the following manner. In the computer memory the sets of explanatory variables (i.e. explanatory vectors) and associated response variables are stored. So, a scalar response variable corresponds to each explanatory vector. The response explanatory vector and the corresponding response variable form a record describing 1 patient. The set of such records creates a reference set.
The predictive value of the response variable for the given explanatory vector can be found as the mean value of response variable values corresponding to the k nearest explanatory vectors. The single predictive error is calculated as err = (predictive value – original value/original value). The reference set can be used to estimate the mean predictive error using the “leave-one-out” method. For each record in the reference set we can calculate the predictive value of the response variable although its true value is known, removing only for the moment the real value. Thus, for each record we can find the predictive error and then the mean predictive error.
The parameter k is found by reviewing all possible values and choosing the one that offers the smallest predictive error. The significance level for the dependence between a single response variable and the explanatory vector (i.e. set of variables) can be found by calculating the significance of Spearman correlation between the real and predictive value of the response variable. For each of the two groups the predictive errors were calculated for all explanatory variable combinations. In this way we could find the best variable combinations. The analyzed data did not meet the conditions of the linear regression as a result of the lack of normality.
Results
The subject of interest was the dependence of the variable drainage volume at 48 h on the variables Hb levels, erythrocytes on day 4 and volume of RBC transfusions. The analyzed data, in both groups, differed significantly from the normal distribution, which could be determined using histograms. Therefore, it was not possible to apply parametric tests, either linear correlation or linear regression.
For group 1 (Tachosil), only the volume of drain-age at 48 h from the RBC transduction volume was found, but at a significance level of 0.0613 with an average value of the Spearman correlation coefficient R = 0.365 (N = 27), which is the test nonparametric. There was also a non-parametric correlation based on the k-NN rule (k nearest neighbors), while taking into account 3 explanatory variables (volume of transfusions, Hb level and number of erythrocytes on the fourth day), but it did not show for group 1 a statistically significant relationship of drainage volume at 48 h with any combination of the above three variables.
In the case of group 2 (control) using a Spearman rank correlation, a statistically significant correlation was found between the drainage volume at 48 h and both the Hb level on the fourth day (p = 0.0109, N = 44) and the number of erythrocytes on the fourth day (p = 0.0048, N = 44) with the mean correlation coefficients R = –0.380 and R = –0.418 respectively. The non-parametric multivariate k-NN regression did not lead to a more statistically significant relationship with any combination of the three variables (i.e., the lower p-value for the k-NN regression was 0.0359). For the dependence of the drainage volume at 48 h on the RBC volume, the significance level p = 0.1262 and the average correlation coefficient R = 0.268 were obtained. The data analyzed did not meet the conditions of linear regression because of the lack of normal distribution.
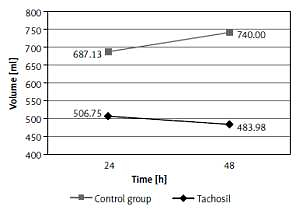
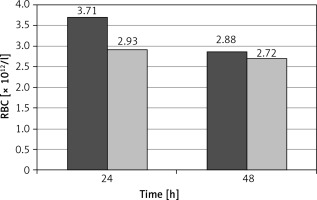
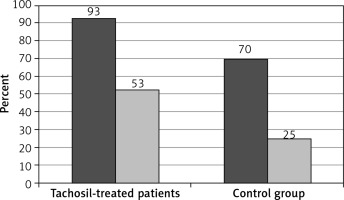
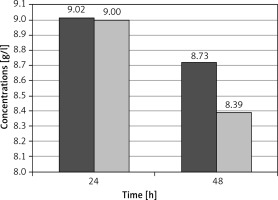
The postoperative drainage after 48 h was significantly lower in the group of patients where the local hemostatic patch (Tachosil) was additionally used, compared to the control group (p = 0.0335). The 24-hour drainage was also lower in Tachosil-treated patients, but the difference did not reach statistical significance (Figure 1). The prevalence of rethoracotomies was twice as high in the control group compared to the Tachosil group (5% vs. 10%), but the statistical analysis did not show a significant difference. As a consequence, both measurements of hemoglobin concentration revealed significantly higher hemoglobin in Tachosil-treated patients than the control group (p < 0.001, p = 0.0002). Red blood cell count (RBC) was also significantly higher in the Tachosil group in both measurements, after 24 and 48 h (Figures 2 and 3). However, the incidence of pericardial and pleural effusions, assessed with transthoracic echocardiography (TTE), was considerably higher in patients in whom Tachosil was used (Figure 4). There were no differences in the perioperative use of tranexamic acid or protamine. The difference in perioperative blood loss between the two groups resulted in a difference in postoperative acute renal injury or renal failure. The prevalence of this complication was non-significantly higher in the control group and accounted for 15% of patients compared to 3% of patients from the Tachosil group. The prevalence of postoperative respiratory failure was similar in both groups of patients (15% in Tachosil-treated patients vs. 8% in control patients). The rate of infection within the early postoperative period was also comparable between the groups, although slightly higher in the Tachosil group (23% vs. 18%). The perioperative mortality was higher in the control group, but did not reach statistical significance (3% in the Tachosil group vs. 5% in the control group). The stay in the intensive care unit (ICU) was longer for the Tachosil group (4.6 vs. 3.3 days). The hospitalization time was also slightly longer in Tachosil-treated patients and was 15.1 days compared to 13.98 days in the control group.
Figure 1
Comparison of the drainage volume in TachoSil and control groups after 24 and 48 postoperative hours
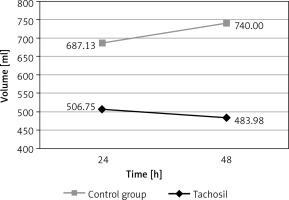
Figure 2
Hemoglobin concentrations in Tachosil (first column) and control (second column) groups after 24 and 48 postoperative hours
Discussion
Cardiac procedures conducted with extracorporeal assist and complete heparinization, when hemodilution cannot be avoided, are associated with excessive blood loss. Not only blood loss itself, but also transfusions, are risk factors for postoperative complications. The adverse effect of transfusions is associated with their immunomodulatory role and volume load. Pneumonia, deep sternal wound infection and sepsis have been identified as transfusion-related postoperative complications [3, 4]. In addition, the cutoff of hemoglobin, at which transfusions should be performed, is still an issue of discussion and confusion [5]. Karkouti et al. [6] found that massive blood loss within the operative day, followed by massive transfusions, increases postoperative mortality similarly to low output syndrome. Surgenor et al. [7] found even 1 to 2 U of RBCs to increase mortality after cardiac surgery in a 5-year follow-up. They also found that patients receiving perioperative blood transfusions have more comorbidities. Similarly, Whitson et al. [8] proved chronic obstructive pulmonary disease (COPD) and smoking to be associated with perioperative blood product transfusions. Among our patients, COPD and smoking were more common in Tachosil-treated patients. Despite this discrepancy, we observed a decreased number of transfusions.
Hemostats are contemporarily available materials that can provide fast, sutureless hemostasis and, what is most important in the context of the presented data, reduce the need for transfusions.
A collagen double layer coated with human fibrinogen and thrombin (Tachosil) has been used with satisfactory results in many clinical situations. Repair of acute aortic dissection [9], postinfarction cardiac rupture [10], and penetrating cardiac injury [11] are the possible application sites of the collagen/fibrinogen/thrombin patch. Local hemostatics can also be used during standard surgical revascularization to reduce bleeding from the bed after harvesting the left internal thoracic artery [12]. Usage of Tachosil during primary cardiac surgery proved to decrease pericardial adhesion formation, which is crucial in the case of an increasing number of reoperations [13]. Additionally, Tachosil can be very helpful in the case of lung lesions. Lorusso et al. [14] reported a case of dangerous lung erosion, associated with severe hemorrhage and air leakage, which was eventually repaired with Tachosil. We described a good result of the additional coverage of an aortotomy suture with a hemostatic patch after aortic valve replacement.
In conclusion, Tachosil use decreased postoperative drainage considerably, which had an important influence on renal complications after aortic valve replacement.