Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CARDIAC SURGERY / CLINICAL RESEARCH
Early and late outcomes after transcatheter versus surgical aortic valve replacement in obese patients
1
Department of Cardiac Surgery, Glenfield Hospital, University Hospitals of Leicester NHS Trust, Leicester, United Kingdom
2
Department of Cardiovascular Sciences, University of Leicester, Leicester, United Kingdom
3
Center for Global Health, Istituto Superiore di Sanità, Rome, Italy
4
Heart Center, Turku University Hospital, Turku, Finland
5
Department of Surgery, University of Turku, Turku, Finland
6
Department of Surgery, University of Oulu, Oulu, Finland
7
Department of Cardiovascular Sciences, Cardiac Surgery Unit, S. Camillo-Forlanini Hospital, Rome, Italy
8
Division of Cardiology, Ferrarotto Hospital, University of Catania, Catania, Italy
9
Department of Cardiovascular Anesthesia and Intensive Care, IRCCS Policlinico San Donato, San Donato Milanese, Milan, Italy
10
Ospedale Careggi di Firenze, Florence, Italy
11
Department of Epidemiology, Lazio Regional Health Service, Rome, Italy
Submission date: 2018-08-29
Final revision date: 2018-11-25
Acceptance date: 2018-12-12
Online publication date: 2019-05-21
Publication date: 2020-05-26
Arch Med Sci 2020;16(4):796-801
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Data on the early and late outcome following transcatheter aortic valve implantation (TAVI) and surgical aortic valve replacement (SAVR) in obese patients are limited. We investigated whether TAVI may be superior to SAVR in obese patients.
Material and methods:
Obese patients (body mass index ≥ 30 kg/m2) who underwent either SAVR or TAVI were identified from the nationwide OBSERVANT registry, and their in-hospital and long-term outcomes were analysed. Propensity score matching was employed to identify two cohorts with similar baseline characteristics.
Results:
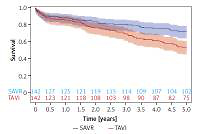
The propensity score matching provided 142 pairs balanced in terms of baseline risk factors. In-hospital and 30-day mortality did not differ between SAVR and TAVI obese patients (4.6% vs. 3.3%, p = 0.56, and 5.2% vs. 3.2%, p = 0.41, respectively). Obese SAVR patients experienced a higher rate of renal failure (12.4% vs. 3.6%, p = 0.0105) and blood transfusion requirement (60.3% vs. 25.7%, p < 0.0001) in comparison with TAVI patients. A higher rate of permanent pacemaker implantation (14.4% vs. 3.6%, p = 0.0018), and major vascular injuries (7.4% vs. 0%, p = 0.0044) occurred in the TAVI group. Five-year survival was higher in the SAVR group compared to the TAVI patient cohort (p = 0.0046), with survival estimates at 1, 3 and 5 years of 88.0%, 80.3%, 71.8% for patients undergoing SAVR, and 85.2%, 69.0%, 52.8% for those subjected to TAVI procedures.
Conclusions:
In obese patients, both SAVR and TAVI are valid treatment options, although in the long term SAVR exhibited higher survival rates.
Data on the early and late outcome following transcatheter aortic valve implantation (TAVI) and surgical aortic valve replacement (SAVR) in obese patients are limited. We investigated whether TAVI may be superior to SAVR in obese patients.
Material and methods:
Obese patients (body mass index ≥ 30 kg/m2) who underwent either SAVR or TAVI were identified from the nationwide OBSERVANT registry, and their in-hospital and long-term outcomes were analysed. Propensity score matching was employed to identify two cohorts with similar baseline characteristics.
Results:
The propensity score matching provided 142 pairs balanced in terms of baseline risk factors. In-hospital and 30-day mortality did not differ between SAVR and TAVI obese patients (4.6% vs. 3.3%, p = 0.56, and 5.2% vs. 3.2%, p = 0.41, respectively). Obese SAVR patients experienced a higher rate of renal failure (12.4% vs. 3.6%, p = 0.0105) and blood transfusion requirement (60.3% vs. 25.7%, p < 0.0001) in comparison with TAVI patients. A higher rate of permanent pacemaker implantation (14.4% vs. 3.6%, p = 0.0018), and major vascular injuries (7.4% vs. 0%, p = 0.0044) occurred in the TAVI group. Five-year survival was higher in the SAVR group compared to the TAVI patient cohort (p = 0.0046), with survival estimates at 1, 3 and 5 years of 88.0%, 80.3%, 71.8% for patients undergoing SAVR, and 85.2%, 69.0%, 52.8% for those subjected to TAVI procedures.
Conclusions:
In obese patients, both SAVR and TAVI are valid treatment options, although in the long term SAVR exhibited higher survival rates.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.