Introduction
Malignant bile duct obstructions (MBO) are usually asso-ciated with advanced stage tumoural pathologies (biliopancreatic tumours, hepatocellular carcinoma, metastasis, etc.). In most cases, curative surgical treatment is not an option at the time of diagnosis, and biliary drainage is performed to palliate associated symptoms and decrease bilirubin levels to allow oncological treatment [1]. Biliary stents are safe and effective options to be used as a part of these palliative decompression interventions, and endobilliary stenting has become a standard procedure for symptomatic palliation of those who are unfit for surgery. Self-expandable metallic stents (SEMS) are the most commonly used method and provide longer patency than other biliary drainage devices [2]. However, even these stents may become occluded due to several factors [3]. Stent patency is a determinant of the cost-effectiveness of the procedure in these patients with low life expectancy and quality of life. In that context, endobilliary radiofrequency ablation (EB-RFA) is a novel and important adjunct to alleviate obstruction and to increase the efficacy of stents [4]. EB-RFA can be used prior to stent placement to provide longer patency. It has been proven to be a safe and effective method in cases with relatively rare complications [5,6]. Two types of EB-RFA systems have been developed: power- and temperature-controlled systems. Temperature-controlled catheters are relatively new and allow temperature monitoring during ablation [7]. Thus, complications related to thermal injury that may develop due to excessive energy can be prevented. This approach is relatively novel, and the number of published cases is still insufficient to determine the full value of percutaneous temperature-controlled EB-RFA regarding patency rates [8].
The purpose of this study was to evaluate the efficacy and safety of temperature-controlled EB-RFA followed by SEMS placement percutaneously in patients with non-resectable malignant biliary obstruction, compared with stenting alone.
Material and methods
Patient population and study design
The study was approved by the Institutional Review Board (approval no. 17073117_050.06_050.06 on 27.10.2020, 20202/11). Informed consent was obtained for the study and all patients were informed about the procedure.
The data of 18 patients who were diagnosed with malignant biliary obstruction and treated with SEMS w/o EB-RFA via percutaneous transhepatic approach were retrospectively reviewed. Nine patients who underwent metallic biliary stenting alone were selected as the control group (non-EB-RFA group). Nine patients treated with EB-RFA followed by metallic stenting were included in the study group (EB-RFA group). The pre-procedural evaluation of all patients was made by the oncologist and surgeon, and they were referred to interventional radiology. Before the procedure, all patients were evaluated clini-cally, biochemically (complete blood count, coagulation parameters, and blood biochemistry), and with imaging modalities (computed tomography, magnetic resonance imaging, ultrasound [US]).
These patients were enrolled between May 2017 and March 2021; all patients had clinical and laboratory findings of biliary obstruction at referral. Malignant biliary obstruction was caused by cholangiocarcinoma, pancreatic cancer, hepatocellular cancer, and metastasis. The criteria for inclusion in this study were as follows: (i) age > 20 years, histopathologically proven malignancy, (ii) clinical and laboratory findings for biliary obstruction, and (iii) surgically unresectable or medically unfit for surgery [9] with life expectancy more than 3 months. Exclusion criteria included uncorrectable coagulopathy (international normalized ratio > 1.5 or platelet count < 50,000 /mm3), clinical instability, surgical operability potential, and life expectancy less than 3 months. Endobilliary RFA stenting was preferred primarily in patients with a diagnosis of cholangiocarcinoma, considering the biliary ductal origin.
Procedural steps
All patients had percutaneous transhepatic cholangio-graphy under fluoroscopy guidance to visualize the biliary tree and evaluate the location and length of the obstructed lumen a week before the stenting procedure. During the same session an 8F, 25 cm long internal-external biliary drainage catheter (Flexima APDL Catheter, Boston Scientific) was inserted for pre-procedural decompression and left in place for 48 to 72 hours until the treatment session.
In the study group, the stenting-ablation procedure was performed under general anaesthesia. A specifically designed temperature-controlled endobilliary RF cathe-ter (ELRA, STARmed) and RF energy generator (VIVA combo RF Generator System, STARmed) were used for ablation. The bipolar electrodes at the terminal portion of the catheter were stainless steel rings (3 mm in width and 18 mm in length) connected to an RF energy generator. After the RF catheter was inserted above the 0.035-inch stiff guidewire, radio-opaque rings were positioned fully across the obstruction. This system operates in temperature mode, which enables continuous maintenance of the chosen electrode temperature during the RF procedure so that excessive heating is avoided. Each ablation procedure was performed at 10 W for 120 s, and the target temperature was set to 80°C. The ablation was started at the distal part of the stricture. Consecutive ablations were performed on strictures longer than the length of the ablation zone of the RFA probe. The RFA probe was removed after ablation and cholangiogram was immediately performed to rule out thermal injury-related complications such as bleeding or perforation. Afterward, balloon dilatation (Powerflex Balloon Catheter, Cordis) was applied up to the original size of the lumen to remove the intra-luminal necrotic tissue. Following balloon dilatation, SEMS (Wallstent, Boston Scientific) with appropriate size (4-12 cm) and diameter (4-12 mm) were inserted in the study group. Following the stent placement, a control cholangiogram was performed to check whether the stent was opened sufficiently, and if necessary, balloon dilation was performed after the procedure (Figures 1-5). The diameters of the stenotic segments before and after the procedure were measured and recorded on fluoroscopy images. An 8 F internal biliary drainage safety catheter was placed over the guidewire and left closed. The safety catheter was then removed a week later after confirming the presence of adequate patency on the control cholangiogram. In patients with tumours involving bilateral hepatic biliary ducts, all procedural steps were repeated on each side and more than one stent was implanted.
Figure 1
73-year-old male patient with a diagnosis of pancreatic head cancer (adenocarcinoma). Cholangiography before the procedure showed occlusion of the common bile duct

Figure 3
After the ablation balloon dilatation was applied at 12 atm to remove the intra-luminal necrotic tissue

Figure 4
Self-expanding metallic stent (SEMS) was inserted over the 0.035- inch guidewire, and control cholangiography showed contrast passage

In the control group, SEMS were inserted at the stricture level with the same stent placement protocol (size [4-8 cm] and diameter [6-10 mm]) as the study group. In the same way, an 8F biliary drainage catheter was inserted for control cholangiography and removed after the demon-stration of free bile flow. First-generation cephalosporine (Cefazoline, 1 g IV) prophylaxis was administered to all patients periprocedurally.
Post-procedural follow-up
In the EB-RFA group, patients were followed up overnight in the hospital, and the non-EB-RFA group was discharged on the same day as the procedure. They were re-examined for clinical success and short-term complications regarding remission of jaundice, biochemical tests, and US findings at the end of the first week. The safety catheter was also removed at the end of the first week following the demonstration of bile flow under fluoroscopy.
Stent patency and patient survival were followed up at regular intervals (first month, third month, and at three-month intervals). When laboratory parameters or clinical findings suggested cholestasis or cholangitis, patients were checked with fluoroscopy for suspected stent occlusion. Patients who were found to have insufficient patency or stent occlusion during follow-up were further treated with RF ablation, balloon dilatation and/or biliary drainage catheter insertion, or second stent placement as appropriate.
The primary outcome of this study was safety and stent patency. Stent patency time was defined as the interval between the first stent placement and the recurrence of obstruction symptoms. The secondary endpoints were overall survival, technical and clinical success, and complication rate. Overall survival was calculated as the time from the first stenting to the last follow-up or death. Technical success was defined as the placement of the stent in the appropriate position and subsequent biliary drainage. Clinical success was defined as an improvement of clinical symptoms of biliary obstruction and a decrease in serum total bilirubin levels of more than 25% of the initial value [10]. Procedure-related complications were defined according to the clinical practice guidelines of the Society of Interventional Radiology Standards of Practice Committee [11].
Results
Of the 18 patients, 15 (83.3%) were men and 3 (16.6%) were women. The RF ablation and control groups were closely matched in terms of age, gender, and co-therapy regimen (p > 0.05). Patient demographic data and clinical features are summarized comparatively in Table 1. Clinical success was achieved in all patients. The EB-RFA and stenting procedure was technically successful in all patients. For patients in the study group who were diagnosed with klatskin tumour, EB-RFA was performed in 3 different localizations, right, left, and main hepatic duct, and they underwent bilateral stenting. Additionally, 2 patients from the control group underwent bilateral stenting.
Table 1
Demographic and baseline clinical characteristics of patients
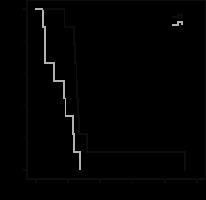
In the study group, the mean pre-ablation luminal dia-meter was 2.3 ± 1.1 mm (range: 1.0-3.5 mm) and the mean post-ablation luminal diameter was 7.9 ± 2.1 mm (range: 5.0-11.0 mm). In the control group, the mean pre-ablation luminal diameter was 1.1 ± 0.9 mm (range: 0-1.2 mm), and the mean post-ablation luminal diameter was 5.5 ± 1.6 mm (range: 3.5-7.0 mm). There was a statistically significant difference between the groups for pre-procedural (p = 0.011) and post-procedural luminal diameter (p = 0.20). Stent patency was calculated as the time from the day the stent was inserted to the day that occlusion was proven or the patient died. In the study group, the median stent patency was 128 days (95% CI: 122.2-133.8), and in the control group it was 86 days (95% CI: 1.2-170.7). It was significantly longer in the EB-RFA group (p = 0.012). Stent patency curves according to Kaplan-Meier analysis are shown in Figure 6. Although the stent patency in each group was comparable to that reported in previous studies, a difference was found in the mean luminal diameter before and after the procedure because patients in our study had a variety of stenosis sites.
Figure 6
Patency comparison with Kaplan-Meier analyses. Curves showing a significant difference in stent patency time between the EB-RFA group and the control group (patency – stent patency)
Clinically, jaundice was resolved in all cases at the end of the first week following the procedure. The pre-procedural total bilirubin level was 8.75 ± 4.26 mmol/l in the study group and 5.73 ± 5.22 mmol/l in the control group. The direct bilirubin level was 6.82 ± 3.34 mmol/l in the study group and 4.53 ± 4.34 mmol/l in the control group. The post-procedural total bilirubin level on the 7th day was 3.83 ± 2.61 mmol/l in the study group and 2.84 ± 2.77 mmol/l in the control group, and direct bilirubin level was 2.78 ± 1.99 mmol/l in the study group and 1.36 ± 1.29 mmol/l in the control group. The difference in total (p = 0.01) and direct bilirubin (p = 0.00) levels was statistically significant in both groups. Clinical success was not significantly different between the groups. Procedural results are summarized in Table 2.
Table 2
Comparison of outcome
In both groups, no procedure-related major complications such as bile duct perforation, peribiliary sepsis, haemorrhage, or pancreatitis were observed. Six patients (4 [44.4%]: study group, 2 [22.2%]: control group, p = 0.620) experienced cholangitis within the first week and were successfully treated with antibiotherapy. Six patients (3 [33.3%]: study group, 3 [33.3%]: control group) had abdominal pain after the procedure; all of them responded to analgesic therapy. No late (7-30 days) complications were reported in either group.
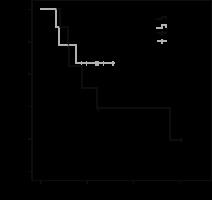
The mean follow-up time was 211.4 ± 144.3 days (range, 81-558 days) in the study group and 192.8 ± 83.4 days (range, 66-310 days) in the control group. Data analyses were performed at 6 months of follow-up. At the end of this period, 5 patients (55.5%) in the study group and 3 patients (33%) in the control group had died. Survival curves according to Kaplan-Meier analysis are shown in Figure 7. The log-rank test showed there was no statistically significant difference in overall survival rates between the study group and the control group (p = 0.302). The mean survival was 267.7 ± 68.5 days (95% CI: 133.3-402.2) in the study group and 239.6 ± 33.9 days (95% CI: 173.1-306.2) in the control group.
Figure 7
Survival comparison with Kaplan-Meier analyses revealed no difference in survival between the EB-RFA group and the control group
Patients with stent occlusion during follow-up were further treated with RF ablation (2 in the study group), balloon dilatation (7 in the study group, 5 in the control group), and biliary drainage catheter insertion (all patients). Additional stenting was required in 2 patients (1 in the study group, 1 in the control group).
Discussion
In patients with malignant biliary obstruction, surgical resection remains the only treatment method for cure. Even with surgical treatment, the 5-year overall survival rate is between 18% and 35% [12]. Most patients with MBO are found have locally advanced stage or metastatic disease. In these patients, palliative interventions to establish and preserve adequate biliary drainage are necessary to prolong survival and to increase the quality of life [13]. In that context, SEMS is accepted as the definitive decompression option for resolving malignant stenosis compared to plastic, covered-metal, and drug-eluting stents [14]. Nevertheless, in the literature, SEMS occlusion rates of up to 50% have been reported within 6–8 months of insertion due to tumoural or non-tumoural (epithelial hyperplasia and/or sludge formation) causes [15,16]. Therefore, alternative management modalities that can prolong stent patency and potentially prolong patient survival were explored. EB-RFA may be a less invasive option to establish stent patency [17]. This relatively novel technique is based on the induction of coagulative necrosis in neighbouring tissues with a thermal effect, and the target is to delay tumour ingrowth and outgrowth. This could prolong the duration of stent patency. RFA can be delivered endoscopically or percutaneously, and previous studies demonstrated the efficacy and safety of these devices with both methods [13,18,19].
In the literature, SEMS was reported to remain patent for periods ranging from 3 to 6 months alone, whereas median stent patency was 4-9 months with the use of the EB-RFA procedure [20,21]. Two types of EB-RFA systems were developed, and most reports are about power-controlled RFA catheters and most are in retrospective nature. In these studies, median stent patency was reported as 4 to 9 months, as mentioned above. There are few studies that were conducted to compare the efficacy and safety of percutaneous EB-RFA and SEMS placement with stent placement alone. In a retrospective study, Cui et al. reported there was significantly higher primary stent patency time in the study group (p = 0.006) [20]. In another study, in which temperature-controlled ablation systems were used, the median stent patency was reported to be significantly longer in the RFA group than in the control group, similarly to our study (p = 0.016) [18]. Wang et al. also stated that RFA adjunct to stenting prolongs stent patency. In our study, the mean stent patency was statistically significantly longer in the RFA group than in the control group (p = 0.012). Additionally, Cui et al. explained differences in outcomes among studies with subgroup analyses. Compared with non-cholangiocarcinoma, cholangiocarcinoma that originates from the bile duct was reported to respond better to EB-RFA [20]. In this context, EB-RFA was primarily chosen before stenting in stenoses of biliary origin. The effect of RFA on overall survival is a more controversial issue, and the results must be interpreted cautiously. Both studies showed no survival benefit in patients with non-resectable malignant biliary obstruction [4,20]. On the other hand, Yiannis et al. and Uyanık et al. reported significantly longer overall survival in the ablation group [18,22]. In our study, there was no significant difference in overall survival between EB-RFA combined treatment and stenting alone (p = 0.302). This may be because many patients die due to progression of malignant disease, not due to stent obstruction and incomplete tumour ablation, as stated above by Wang et al. The effect of endobilliary RFA on survival remains controversial, and prospective studies with aetiological subgroup analyses in larger study groups are needed.
Several complications could be associated with uncontrolled high-temperature power-controlled catheters. The ablation of perihilar MBO in particular is considered to involve a high risk of complications. In the literature, Tal et al. and Dolak et al. reported various major complications that are thought to be due to uncontrolled high temperature, such as liver infarction and hepatic coma [23,24]. Moreover, Zhou et al. reported 2 cases of biliary perforation, one resulting in mortality [25]. On the other hand, the previous prospective randomized study on the endoscopic usage of temperature-controlled ELRA showed that this novel device was safe and there were no unintended thermal injury-related complications in the ablation group [10]. In this study, we used a temperature-controlled EB-RFA system percutaneously, and there were no major complications in either group. The low complication rate in our study may be associated with the newly developed system we used. Control of temperature in the ablation zone offers reduced risk of biliary complications, and in our study there was no statistically significant difference between the 2 groups in terms of cholangitis rate, a minor complication (p > 0.05).
This study had some limitations. Firstly, it was designed retrospectively with a limited number of patients. Prospective studies including different aetiologies in more homogeneous and specific patient groups will help to more clearly determine the effect of endobilliary ablation.




