Introduction
Sacrococcygeal pilonidal sinus (SPS) is a common condition caused by the invagination of hair follicles leading to inflammation and abscess formation in the sacrococcygeal region. It is an acquired condition with local inflammation and infection of hair follicles, causing abscesses and fistula tract. Various surgical techniques are available to manage pilonidal sinus, but there is still controversy concerning the optimal surgical approach [1]. Furthermore, despite the many defined operation methods, there is still a high risk of recurrence. Thus, new methods continue to be tried to achieve optimal treatment.
As in other surgical operative diseases, new noninvasive techniques are also being investigated in pilonidal sinus. For example, in 2013, Meinero et al. proposed a new minimally invasive procedure for treating SPS with a fistuloscope called endoscopic pilonidal sinus treatment (EPSIT) [2]. The technique utilizes a specially designed optical fistuloscope inserted through a small circular incision around the pilonidal sinus opening. Once defined under direct vision, sinus debridement is performed with an endograsper and endobrush. Then a monopolar electrode is inserted through the fistuloscope to enable electrocautery of the sinus tracts [2–4].
After this operation step, laser therapy is offered as an adjuvant treatment option. Recently, Pappas et al. hypothesized that laser energy delivered using a radial emitting fiber could successfully ablate the epithelium of a pilonidal sinus, promoting the production of new granulation tissue with consequent healing of the sinus [5]. They named this relatively new therapeutic approach sinus laser therapy (SiLaT).
EPSIT is an effective treatment, but there still needs to be a consensus on whether applying the laser to this method improves outcomes.
Aim
This study aimed to compare our EPSIT and SiLaT cases to evaluate the efficiency of laser therapy.
Material and methods
Our study retrospectively analyzed 73 patients (aged 12–46) with sacrococcygeal pilonidal sinus and treated with either EPSIT or SiLaT between September 2019 and September 2021. All primary pilonidal sinus patients within these 2 years were included in the study. Patients with concurrent abscess formation and recurrent pilonidal sinus were excluded. The patients were randomized to the EPSIT group (n = 36) or SiLaT group (n = 37) consecutively by an independent person using patient admission numbers. The two groups were compared in terms of the average number of fistulas, location of the fistulas, mean follow-up period, operative time, intraoperative complications, early complications (bleeding), pain score, duration of analgesia use, mean postoperative time of total wound healing, time to return to daily life, and late postoperative complications (recurrence).
The advantages and disadvantages of each technique were explained to each patient. Written informed consent was taken from all of the patients. All patients were given antibiotic treatment before the procedure and treated after the resolution of the inflammatory process. Patient information was recorded retrospectively, including age, body mass index (BMI), gender, and operative time.
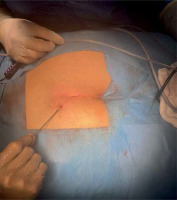
The EPSIT procedure was performed under general anesthesia. Pre-operative antibiotic prophylaxis was administered, patients were placed prone, and the buttocks were separated. EPSIT included a small circular incision of 0.5 cm around the fistula opening to insert a fistuloscope, an eight-angled eyepiece equipped with an optical channel and a working and irrigation channel, with a diameter of 3.2 × 4.8 mm and an operative length of 18 cm, as developed by Meinero et al. [2]. After hair removal and cleaning of the infected area, the walls and external openings of the sinus were electrocoagulated (Photo 1). The first part of the operation, cleaning hair and debris away from the sinus and the secondary tracts using a brush or punch biopsy forceps and curetting the inflammatory tissue and epithelium lining of the tracts is common in both techniques. In the SiLaT method, a diode laser fiber adequate at 360° is inserted and introduced into the sinus tract afterwards [5]. Energy is transferred continuously to destroy the granulation. Every other pit is treated this way (Photo 2). It is postulated that laser energy causes progressive shrinkage of the pilonidal tracts.
Photo 1
In EPSIT, after hair removal and cleaning of the infected area, the walls and external openings of the sinus were electrocoagulated
The postoperative evaluation was performed every week. Pain score (visual analog scale), need for analgesia, day of discharge, and wound healing time were recorded. Visual follow-up was scheduled at 3, 6, and 12 months postoperatively.
Statistical analysis
The statistical analysis of this study was performed using the package program SPSS for Windows 15.0 (SPSS Inc., Chicago, USA). Descriptive statistics were given as numbers and percentages for categorical variables, as mean, standard deviation, minimum, and maximum for numerical variables. The χ2 test was applied to the difference between the groups. A comparison of numerical variables was made with the Mann-Whitney U test in two independent groups since the normal distribution could not be met. P-values lower than 0.05 were accepted as significant.
Results
We analyzed 73 cases of patients who underwent EPSIT or SiLaT with a mean age of 23.4 ±8.4 (12–46) years and body mass index (BMI) of 25.5±4.5 (18–38) kg/m2. Among them, 36 patients (26 males, 10 females) underwent EPSIT, and 37 (27 males, 10 females) underwent SiLaT. The median number of fistulae from the sinus was 1 (1–3). The localization of the fistula was midline in thirty-four and lateral in two of the patients in the EPSIT group, whereas it was midline in thirty-five and lateral in two of the patients in the SiLaT group. The mean follow-up period was 13.5 ±9.5 months (0–36). The operative time was similar for both groups (32.3 ±14.8 vs. 31.0 ±14.8; p = 0.757). No major intraoperative complications were reported. Early complications (bleeding and fat necrosis) were recorded in 2 patients in the SiLaT group. The duration of analgesia use was significantly shorter in the EPSIT group compared to the SiLaT group (1.3 ±0.5 (1–3) vs. 1.9 ±1.1 (1–5) days; p = 0.005; Table I). The mean postoperative time of total wound healing was similar for both groups: 23.6 ±14.7 (12–90) vs. 25.2 ±14.5 (14–90) days (p = 0.385). There was no significant difference regarding the average time of return to total daily activity – 3.4 ±0.9 (2–5) vs. 3.6 ±1.2 (2–7) days (p = 0.679). There was no significant difference between the groups regarding late postoperative complications (recurrence: 7; p = 0.05). Four patients experienced recurrence (11.1%) after EPSIT, while there were three recurrences (8.1%) after SiLaT (p = 0.711). Of the 7 patients in whom recurrence was detected, the average presentation time for recurrence was 5.8 months (1–10). For two of the 7 patients with recurrence, open surgery with a Karydakis flap, and 5 patients under local anesthesia, crystallized phenol was applied as described by Şengül et al. [6].
Table I
Comparison between EPSIT and SiLaT procedures
| Parameter | EPS (mean ± SD) | SiLaT (mean ± SD) | P-value |
|---|---|---|---|
| Operative time [min] | 32.3 ±14.8 (10–80) | 31.0 ±14.8 (8–60) | 0.757 |
| Duration of analgesic use [days] | 1.3 ±0.5 (1–3) | 1.9 ±1.1 (1–5) | 0.005* |
| Wound healing [days] | 23.6 ±14.7 (12–90) | 25.2 ±14.5 (14–90) | 0.385 |
| Return to total daily activity [days] | 3.4 ±0.9 (2–5) | 3.6 ±1.2 (2–7) | 0.679 |
| Early complication – bleeding (%) | 0 (0.0%) | 2 (5.4%) | 0.878 |
| Late complication – recurrence (%) | 4 (11.1%) | 3 (8.1%) | 0.711 |
Discussion
Pilonidal sinus is a common disease, and an optimal surgical treatment method has not yet been determined [7]. The treatment objectives are simple, requiring local anesthesia, minimum hospitalization, short recovery and quick return to daily activities, less postoperative pain, a high success rate, and low cost [8]. Conservative methods are either primary or secondary closure, and flap techniques entail a high risk of recurrence arising from the pathophysiology of pilonidal sinus disease [9–11]. Recently, as in other branches of surgery, minimally invasive methods such as EPSIT and SiLaT have been described in this field [12, 13]. These methods promise shorter wound healing time and time to return to work, and improved pain control and cosmesis. Endoscopic procedures can also be used in adolescent patients, and these methods also reduce the sense of embarrassment that patients experience [14, 15]. EPSIT is a minimally invasive method described by Meinero et al. [2]. Esposito et al. adapted EPSIT to the pediatric population as PEPSIT (pediatric EPSIT) and presented it in 2018 [16]. Dotlacil et al. reported one of the largest series on PEPSIT, in which they achieved 87% healing after the first PEPSIT and confirmed minimal invasiveness, short hospital stay, and low requirement of analgesics [15].
SiLaT was described by Pappas and Christodoulou [5]. The idea depends on the fact that high laser energy destroys the sinus tracts and shrinks the tissues around them without affecting the overlying skin. The first parts of both EPSIT and SiLaT procedures are similar and include careful endoscopic cavity cleaning to reduce the risk of recurrence. In the SiLaT method, the laser energy is delivered to the cavity, and the obliteration of the cavity is assumed. No studies have yet compared the effects of these two methods. Our study is the first to evaluate the impact of adding laser therapy to the endoscopic procedure.
The present study compared the outcome of two surgical techniques in managing pilonidal sinus EPSIT and SiLaT. EPSIT is similar to SiLaT, in which the sinus is thoroughly curetted under the laparoscopic vision and then ablated using cautery. In SiLaT a laser probe is used afterward. According to the existing literature, both techniques have achieved promising results in terms of successful sinus healing and minimal complications [5, 12, 13].
Our study included 73 patients with a male-to-female ratio of 2,5, concomitant with the study of Abdelnaby et al. with male predominance [4]. There were no significant differences between groups regarding operative time, returning daily activity, and wound healing.
Only the duration of analgesic use was significantly shorter in the EPSIT group. The early complication was minimal bleeding in 2 patients in the SiLaT group, but there was no significant difference in early complications between the groups.
The postoperative recurrence rate of the SiLaT group was 8.1%, and this was in line with the previous report of Abdelnaby et al. [4]. Regarding EPSIT, our postoperative recurrence rate (11.1%) is comparable to the rate of 10.5% reported by Sequeira et al. [1]. However, there was no significant difference in recurrence rate between the two groups in our study.
This raises questions about the necessity of laser treatment that requires extra effort by the surgeon, requiring the surgeon to rely on external sources. There is also a significant difference between the two methods regarding analgesic usage. This calls into question the superiority of EPSIT and the necessity of the laser part. The limitation of this study is the relatively low number of patients.
Conclusions
Both EPSIT and SiLaT are minimally invasive methods that are painless, easy to perform, and include short hospital stays for patients, with a quick return to normal daily activities. Laser therapy is not an essential part of endoscopic treatment, as it does not affect the complication and recurrence rates, even increasing postoperative analgesic usage. However, more comprehensive studies are needed, with more patients included.










