Introduction
Stroke is a sudden neurological deficit due to various causes. It can be ischaemic as in large vessel occlusions or haemorrhagic as in rupture of arteriovenous malformation (AVM) or cerebral venous sinus thrombosis (CVT). Stroke related to CVT is rare, accounting for < 1% of cases [1]. It can affect a wide range of populations, mainly neonates and young adults (third decade), and especially females, due to multiple risk factors [2]. Clinical diagnosis is difficult, and a high level of suspicion with appropriate imaging can make an accurate diagnosis in most cases. Systemic anticoagulation with neuroprotection is the first line of management [3,4]. Cases resistant to systemic anticoagulation can opt for endovascular management. Endovascular options include intraarterial thrombolysis with or without mechanical thrombectomy (MT) and thromboaspiration. Multiple techniques for thrombectomy are available: direct catheter directed aspiration only, mechanical thrombectomy using a stent retriever, rheolytic catheter-directed thrombectomy, and balloon-assisted thrombectomy [1].
Our study aimed at describing the outcome of this novel technique of MT for CVT in cases not responding to the medical line of management. This is the first of its kind single-centre experience in this part of the country.
Styczen et al. in their study conducted in 2011-2018 described endovascular management as possible, safe, and effective with a highly successful recanalization rate [1]. Shui et al. in their study described balloon dilation and aspiration of an occluded sinus to be a safe and effective treatment for cerebral venous sinus thrombosis [5,6].
Material and methods
We report a tertiary-centre experience of outcomes of patients who underwent mechanical thrombectomy for CVT between December 2017 and December 2022 in our institute by retrospective analysis. Of the total 70 patients presenting with CVT in this period, 8 patients (11.4%) underwent mechanical thrombectomy and were included in this study. Patient details related to the CVT risk score, imaging features, endovascular procedure details, their associated complications, and the patient’s neurological status at the time of discharge were noted. The details are provided in Table 1.
Table 1
Patient characteristics
Imaging
All the patients suspected of having CVT underwent appropriate imaging by either contrast-enhanced computed tomography (CT) or magnetic resonance imaging (MRI) with venography. Radiological features like the number of sinuses involved, location of thrombus (superficial or deep), and presence of haemorrhage were noted.
Patient selection for MT
All the patients received intravenous heparin as per the advice of the attending neurologist. Appropriately selected patients who responded poorly to the anticoagulation were evaluated combinedly by neurologists and an interventional neuro-radiologist. Poor prognostic factors like the progression of symptoms despite systemic anticoagulation with heparin, involvement of deep veins, seizures, and altered mental status were documented, and the CVT risk score was assessed. Patients were stratified according to the CVT risk score. A score of < 3 points was regarded as a good outcome of treatment while any score > 3 indicated a patient having poor outcomes. These patients subsequently underwent mechanical thrombectomy. Post-procedure control CT was done after 24 hours regularly in all patients to assess the outcome of the procedure and rule out any complications. Clinical outcomes were assessed with the modified Rankin Scale (mRS, Table 2) at the time of discharge. Five patients had a CVT risk score of 3 (63%), 2 patients had a risk score of 4 (25%), and one patient had a risk score of 5 (12%). All the patients in the study were in a high-risk group and had a poor outcome if not treated (Table 3).
Table 2
Modified Rankin Scale (mRS) score
Endovascular methods
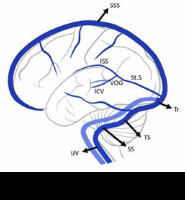
Mechanical thrombectomy was carried out under general anaesthesia in all 8 patients. With all aseptic precautions and with USG guidance, first the femoral arterial access was taken and secured with a 5F short sheath, followed by selective cannulation of the internal carotid artery ipsilateral to the venous lesion. The diagnosis was confirmed by angiogram. Subsequently, the femoral venous access was taken, and with the help of a 6F long sheath, access to the cerebral venous vasculature was obtained. The tip of the long sheath was located in the internal jugular bulb, and then an aspiration catheter was inserted. In some patients, only mechanical thromboaspiration was done, with the help of any one of the aspiration catheters (ACE 68, pe-numbra INC USA; REACT 71, Medtronic plc, Ireland; or AXS CATALYST 7, Stryker neurovascular, USA). The tip of the catheter was placed just proximally to the thrombus and aspiration via syringe (60-ml vacuum lock), the vacuum pump was started, and the aspiration catheter was moved from a proximal to a distal manner. Intermittent angiograms were obtained via arterial access catheter to assess the state of recanalization of veins. In cases where stent retrievers were used for thrombectomy, a microcatheter/microwire combination was used to reach the distal part of the thrombus with along with aspiration catheter and long sheath. Subsequently, the microwire was removed, and the stent retriever was passed and deployed across the thrombus and left for a few minutes. The aspiration catheter was passed under continuous aspiration along the stent retriever wire. Then, the aspiration catheter and stent retriever were withdrawn under continuous aspiration as a single unit. In one of our cases, balloon venoplasty was done in addition to mechanical thromboaspiration. Once the antegrade flow was noticed, the procedure was terminated irrespective of degree of recanalization. The use of different techniques, devices, and number of attempts was left to the attending interventionalist according to the circumstances. The pictorial representation is shown in Figure 2 with brief cerebral venous anatomy presented in Figure 1.
Figure 2
Pictorial representation of a setup for thrombectomy with left-side image showing only aspiration and right-side image showing stent retriever thrombectomy with aspiration
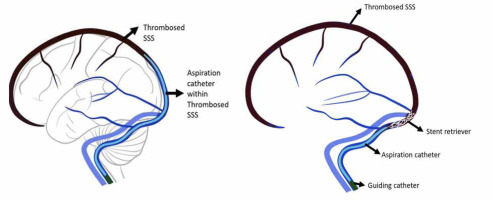
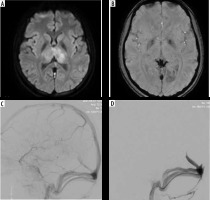
Figure 3
19-year-old female with deep cerebral venous thrombosis: (A) diffusion-weighted image shows bilateral thalamic infarcts; (B) susceptibility weighted image shows blooming in deep veins suggestive of thrombosis; (C) and (D) shows mechanical thrombectomy of deep veins with partial recanalization
Results
In our study a total of 8 patients (3 females and 5 males) were included, with ages ranging from 18 to 50 years (mean age 34 years). The most common symptom was headache in all the patients (n = 8; 100%) followed by seizures (n = 5; 62.5%), disorientation/coma (n = 5; 62.5%), and focal neurological deficits (n = 4; 50%). All patients had a new-onset headache with an average duration of 4 days; 50% (n = 4) of patients had neurological deficits at the time of presentation.
The most common identifiable risk factor for CVT was iron deficiency anaemia (50%, n = 4) in this study. One patient was identified to have evolving lupus (12.5%), and another patient had associated congenital heart disease, but there were no identifiable causes in the rest of the patients. Sinus thrombosis was confirmed in the superior sagittal sinus in 75% of the cases (n = 6), transverse sinus in 62.5 % (n = 5), and deep veins in 50% of the cases (n = 4).In 75% (n = 6) of the cases, 2 or more sinuses were involved. All involved sinuses showed > 75% of thrombosis. Initial haemorrhage was noted in 62.5% (n = 5) of the cases; non-haemorrhagic infarcts were noted in 25% (n = 2).
All the patients received intravenous heparin for anticoagulation in a weight-adjusted dose. After the acute phase, at the time of discharge, the patients received oral anticoagulants to prevent recurrence. Six patients (75%) worsened neurologically while 2 patients showed no improvement with intravenous heparin. All patients had a risk score ≥ 3 CVT for poor outcome.
Among 8 patients, 3 (37.5%) underwent thrombectomy within 24 hours and were comatose at presentation; 4 out 8 underwent endovascular procedure within 48 hours; and one patient underwent the procedure on 4th day because of stable neurological status but with no improvement despite systemic anticoagulation.
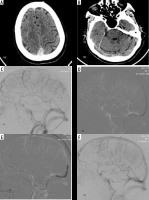
Among all 8 patients, thromboaspiration alone (Fig-ure 3) was used in 5 (62.5%) cases, a combined approach of aspiration with stent retriever thrombectomy was used in 2 patients (25%), and thromboaspiration combined with venoplasty (Figure 4) was done in one patient (12.5%).
Figure 4
43-year-old female with cerebral sinovenous thrombosis involving superior sagittal sinus and right transverse sinus with SAH in right frontal lobe (A and B – CT images). Image C (venogram – digital subtraction angiography) shows non-opacification of superior sagittal sinus and torcula with irregularity of right transverse sinus – s/o thrombosis. Images (D) and (E) show mechanical thromboaspiration and venoplasty, respectively, followed by complete recanalization as seen in image (F)
Successful recanalization was achieved in all 8 patients (100%). Complete recanalization was achieved in 5 out of 8 patients (62.5%), and partial recanalization was achieved in 3 out of 8 patients (37.5%). Mechanical thromboaspiration alone achieved complete recanalization in 3 patients (60%) and partial recanalization in 2 patients (40%). Combined procedures achieved complete recanalization in all cases (2 out of 2 cases, 100%).
Intraprocedural complications were observed in 2 cases (25%) with cortical vein rupture, contrast extravasations, and SAH; however, in both patients, recanalization was successful and kept under systemic anticoagulation. During hospital stay, they improved neurologically and discharged with an mRS of 0.
One patient showed an increase in intracranial haemorrhage (12.5%) in the post-procedure period but was managed conservatively. One patient (1/8 = 12.5%) with congenital heart disease and CVT died on the second day post procedure despite recanalization of occluded dural venous sinuses and systemic anticoagulation.
Discussion
Cerebral venous thrombosis is an uncommon cause of stroke with variable and nonspecific clinical presentation from headache to coma [1,2]. According to our study, iron deficiency anaemia was a commonly identifiable risk factor for CVT. According to our study, coma/altered mental status at presentation, deep venous system involvement, and ICH were identified as risk factors for poor neurological outcome. Large thrombus burden with thrombosis involving a long segment of the dural sinuses was commonly noted in these patients. which in turn resulted in a dramatic increase in intracranial pressure and increased risk for ICH, infarction, and cerebral oedema [3]. Like in arterial stroke, MT with the restoration of antegrade venous flow in addition to systemic anticoagulation could be an effective management strategy in severe CVT/CVT resistant to systemic anticoagulation [5,6].
In this study, the recanalization rate was higher (100%) than described in recent literature reviews [1,2]. Our results were comparable with a study done by Siddiqui et al. [7], who showed a recanalization rate of 95% and new or worsening ICH of 10%, compared to 100% and 12.5% in this study, respectively. The degree of recanalization was slightly better than our study (74% vs. 62.5% of complete recanalization). The small sample size of our study may account for this low rate of complete recanalization. However, our study is comparable with the study done by Ilyas et al. [8] in terms of complete recanalization (i.e. 69% vs. 62.5%, respectively). Mechanical irritation by venous thrombus might increase the heparin’s anticoagulant effect, leading to rapid recanalization; hence, patients treated only with heparin also show recanalization of approximately 60-70%, but after a few weeks to a few months [3].
The transvenous approach for thrombectomy and access to dural venous sinuses is a safe and effective technique due to avoidance of the deep cerebral veins. In our study, dural sinus perforation did not occur (0%), in contrast to previous studies [8] that showed 0.1 to 2.1% of sinus perforation. The periprocedural complications (including ICH) vary between 9% and 13% according to previous literature [7, 8], which is comparable with our study results (12.5%).
The study by Siddiqui et al. [7] showed a higher rate of ICH if patients were treated with MT and intrasinus thrombolysis (11%) compared with only MT (7%). But this is not statically significant, due to the small sample size of the study. Intrasinus catheter-directed thrombolysis was not used in this study.
Recent studies in the literature showed mortality rates of 4% to 14% for severe CVT patients undergoing MT (12.5% in our study). These studies also revealed that 72% showed excellent outcome with mRS 0 to 1 and 84% showed a favourable outcome with mRS 0 to 2. Our study showed ~75% excellent and ~87.5% favourable outcomes with good correlation, despite a lower rate of complete recanalization. This may be explained by various factors including variable thrombus burden, presence or absence of deep cerebral vein thrombosis, variable presentation at baseline, different time points between mechanical thrombectomy and symptom onset, and spontaneous resolution of venous thrombi due to good collateralization of the cerebral venous system compared to the arterial system.
According to the literature [7,9,10], Angiojet is used most frequently (26-47%) for thrombectomy, despite a lower rate of complete recanalization and less favourable outcomes. The stiffness of the Angiojet device and the penetrating risk of the water jet may account for these negative results. In contrast, stent retriever thrombectomy and direct aspiration with aspiration catheter was infrequently reported in the literature (stent retriever 0-12%; aspiration 7-9%).
In the present study, we used all the latest-generation aspiration catheters (ACE 68, REACT 71, CAT 7) with greater internal diameter and aspiration power [4,5]. The interventionalist used different stent retriever devices/aspiration systems in our study, but in all cases the largest size available was deployed. Large-vessel ischaemic stroke thrombectomy devices have improved the safety profile of devices used for CVT [5-7].
Large prospective studies could be done in the future with broader inclusion criteria to add severe CVT patients to ascertain the benefits of endovascular therapy, as well as randomized control studies to compare the different thrombectomy methods/devices.
The small sample size, retrospective approach, inhomogeneity of thrombectomy methods/devices, and the lack of a control group are limitations of this study. Catheter-directed thrombolysis was not used in our study, which may be another limitation; however, high risk of post-procedural haemorrhage and less favourable outcomes were reported with thrombolysis in the literature [7,10].
Conclusions
To conclude, the mechanical thrombectomy (MT) appears to be a safe and effective treatment for severe (risk score ≥ 3) and refractory CVT to systemic anticoagulation. However, further prospective studies are necessary to determine the predictors and effective endovascular techniques as well as formulation of selection criteria for mechanical thrombectomy for successful treatment of CVT.