Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
CORONARY ARTERY DISEASE / CLINICAL RESEARCH
Gender-related disparities in the treatment and outcomes in patients with non-ST-segment elevation myocardial infarction: results from the Polish Registry of Acute Coronary Syndromes (PL-ACS) in the years 2012–2014
Marcin Sadowski
1,5
1
The Faculty of Medicine and Health Sciences, The Jan Kochanowski University, Department of Anatomy, Kielce, Poland
2
2nd Department of Cardiology, Świętokrzyskie Cardiology Centre, Kielce, Poland
3
3rd Department of Cardiology, School of Medicine with the Division of Dentistry in Zabrze, Medical University of Silesia in Katowice, Silesian Centre for Heart Disease, Zabrze, Poland
4
Department of Cardiology, University Hospital, Institute of Medicine, University of Opole, Poland
5
Catheterisation Laboratory, Świętokrzyskie Cardiology Centre, Kielce, Poland
Submission date: 2017-11-03
Final revision date: 2018-01-09
Acceptance date: 2018-01-14
Online publication date: 2020-02-28
Publication date: 2020-05-26
Arch Med Sci 2020;16(4):781-788
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Gender-related differences in the treatment of patients with non-ST elevation myocardial infarction (NSTEMI) have been reported in many previous studies despite the fact that an equal approach is recommended in all current guidelines. The aim of the study was to investigate whether gender-related discrepancies in the management of NSTEMI patients have changed.
Material and methods:
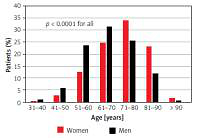
Between 2012 and 2014 a total of 66,667 patients (38.3% of whom were women) with the final diagnosis of NSTEMI were included into the retrospective analysis of the Polish Registry of Acute Coronary Syndromes (PL-ACS). Differences in clinical profile, treatment, and outcomes were analysed.
Results:
Women were older than men and more often had comorbidities. They were less likely to undergo coronary angiography (88.4% vs. 92.1%, p < 0.05) as well as percutaneous coronary intervention (59.6% vs. 71.9%, p < 0.05). In the general population women had also significantly worse in-hospital prognosis as well as in 12-month follow-up. After the age adjustment the outcomes in women were at least as good as in men. In multivariate analysis females had the same risk as men in-hospital RR = 1.02 (95% CI: 0.97–1.08, p = 0.45) and lower in 12-month observation RR = 0.94 (95% CI: 0.92–0.97, p < 0.0001).
Conclusions:
In comparison with previous reports on NSTEMI patients, gender-related disparities in the treatment and outcomes were radically reduced. Unadjusted mortality rates were still higher in women as a consequence of their older age. After the age adjustment, mortality ratios were similar in both genders. The long-term prognosis seems to be even better in women.
Gender-related differences in the treatment of patients with non-ST elevation myocardial infarction (NSTEMI) have been reported in many previous studies despite the fact that an equal approach is recommended in all current guidelines. The aim of the study was to investigate whether gender-related discrepancies in the management of NSTEMI patients have changed.
Material and methods:
Between 2012 and 2014 a total of 66,667 patients (38.3% of whom were women) with the final diagnosis of NSTEMI were included into the retrospective analysis of the Polish Registry of Acute Coronary Syndromes (PL-ACS). Differences in clinical profile, treatment, and outcomes were analysed.
Results:
Women were older than men and more often had comorbidities. They were less likely to undergo coronary angiography (88.4% vs. 92.1%, p < 0.05) as well as percutaneous coronary intervention (59.6% vs. 71.9%, p < 0.05). In the general population women had also significantly worse in-hospital prognosis as well as in 12-month follow-up. After the age adjustment the outcomes in women were at least as good as in men. In multivariate analysis females had the same risk as men in-hospital RR = 1.02 (95% CI: 0.97–1.08, p = 0.45) and lower in 12-month observation RR = 0.94 (95% CI: 0.92–0.97, p < 0.0001).
Conclusions:
In comparison with previous reports on NSTEMI patients, gender-related disparities in the treatment and outcomes were radically reduced. Unadjusted mortality rates were still higher in women as a consequence of their older age. After the age adjustment, mortality ratios were similar in both genders. The long-term prognosis seems to be even better in women.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.