Introduction
Minimally invasive surgery and the ERAS (Enhanced Recovery after Surgery) protocol revolutionized perioperative care for gastrointestinal surgical procedures [1–4]. While the most extensive research involved colorectal diseases, ERAS was found to be beneficial in other branches of surgery [5, 6]. Its application diminished postoperative morbidity and reduced hospital length of stay [6]. In 2014 the ERAS Society published its guidelines for perioperative care after gastrectomy [7]. Many versions of the ERAS protocol, however, are still being used in different surgical departments [6, 8]. Nevertheless, the main elements of the ERAS protocol remain common [6]. Many authors report that introduction of the ERAS protocol improves the short-term outcomes as well as compliance to its elements [9]. However, the ERAS protocol is not as commonly used in gastric surgery. Studies on long-term outcomes in this field are lacking, too [10]. The advances in surgical technique currently are marginal; therefore we should investigate meticulously other items contributing to final outcomes of gastric cancer surgery [11]. Recently, several papers revealed that compliance to the ERAS protocol may affect long-term survival in patients with cancer [12, 13], which is the most objective benchmark in assessment of oncological treatment. The reason for this association is still under investigation. So far, no such influence has been investigated regarding gastric cancer surgery.
Aim
To evaluate whether adherence to the ERAS protocol affects survival in patients undergoing gastric cancer surgery.
Material and methods
We performed a retrospective analysis of a prospective collected database of patients treated for gastric cancer between 2013 and 2016. In 2012 laparoscopic total gastrectomy became the method of choice in gastric cancer. Qualification for preoperative chemotherapy was performed based on ESMO guidelines [14]. All patients were treated perioperatively with a 14-item ERAS protocol (Table I).
Table I
ERAS protocol used in our department
Every patient underwent regular follow-up every 3 months for 3 years after surgery. It included general check-up and computed tomography imaging for recurrence and distant metastasis evaluation.
Operative technique
All patients underwent D2 gastrectomy with spleen preservation in the laparoscopic approach. Reconstruction of the digestive tract was done with the Roux-en-Y approach. The esophago-jejunal anastomosis was carried out with a linear 45 mm GIA stapler and jejuno-jejunal anastomosis. In both anastomoses the common orifice was closed by a hand-sewn suture. No routine drainage of the peritoneal cavity was used.
Inclusion criteria
Inclusion criteria were: 18 years old, histologically confirmed gastric adenocarcinoma, procedure performed with a laparoscopic approach (gastrectomy with D2 lymphadenectomy), and follow-up of at least 12 months. Patients with stage IV cancer according to the AJCC classification, patients operated initially with an open approach and patients after conversion, patients who died within 30 days after the initial procedure, and patients requiring multivisceral resections and patients with locally inoperable cancer were all excluded from the analysis.
Outcome measures
For the study purposes, patients were divided into two groups depending on their compliance to the ERAS protocol. Patients with compliance of equal to or more than 80% formed group 1. Patients with compliance of less than 80% represented group 2. We did not include postoperative elements of the ERAS protocol in the adherence calculation. As a result, compliance to the ERAS protocol was calculated by dividing the number of components fulfilled by 11.
The primary outcome was 3-year overall survival. The secondary outcomes were perioperative complications, length of stay, and recovery parameters.
Ethical approval
The study was approved by the local Ethics Review Committee (approval number 1072.6120.225.2017). All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Statistical analysis
All data were analyzed with StatSoft Statistica v.13 (StatSoft Inc., Tulsa, OK, USA). The results are presented as mean ± standard deviation (SD), median and interquartile range (IQR), and hazard ratio (HR) with 95% confidence intervals (CI) when appropriate. The study of categorical variables used the χ2 test of independence. The Shapiro-Wilk test was used to check for normal distribution of data and Student’s test was used for normally distributed quantitative data. For non-normally distributed quantitative variables, the Mann-Whitney U test was used. For the purposes of further analysis, the entire group of patients was divided into subgroups depending on compliance with the ERAS protocol (< 80% and ≥ 80%). This was the target compliance with the ERAS protocol in our department. Survival data were analyzed according to the Kaplan-Meier method. The log-rank test was used to detect differences between groups. Univariate and multivariate analysis was performed using Cox proportional hazards. The variables with p < 0.05 were included in the model. Results were considered statistically significant when the p-value was found to be less than 0.05.
Results
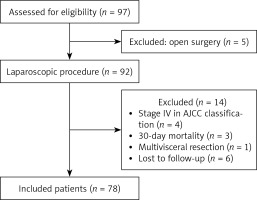
During the study period, 97 patients with gastric cancer underwent total gastrectomy. Eventually, 78 patients were included in the analysis (51 males and 27 females). Mean age was 61.2 ±10.7 years. Mean compliance to the ERAS protocol in the whole group was 75.6%.
Group 1 (patients with compliance > 80%) included 34 patients and group 2 (patients with compliance < 80%) included 44 patients. The groups did not differ in terms of sex, age, BMI, ASA class and comorbidities. Both groups were also similar in terms of stage of the disease. Forty-six (58%) patients required adjuvant chemotherapy; the number of individuals was not statistically different between groups. The data are summarized in Table II.
Table II
Demographic analysis of patient group
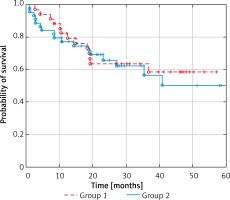
A subgroup analysis demonstrated that the patients in group 1 and group 2 did not statistically differ in terms of 3-year overall survival (Figure 1).
Patients in group 1 required shorter length of stay in the hospital (mean: 6.0 ±4.1 days vs. 10.4 ±13.3 days; p = 0.0052). However, multivariate regression analysis revealed that only complications were a risk factor for prolonged hospitalization (β = –0.68; 95% CI: (–0.95, –0.42); p < 0.001). Patients with high compliance had a lower complication rate (20.6% vs. 29.5%), although the result did not reach statistical significance.
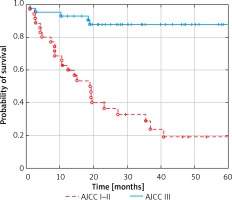
Univariate analysis of overall survival identified only stage III AJCC as a risk factor of poor prognosis in patients operated on due to gastric cancer (HR = 7.89, 95% CI: 2.96–20.89; p = 0.0001; Table III).
Table III
Univariate analysis of overall survival
According to Kaplan-Maier curves, probability of 3-year overall survival for group 1 was 63% and 56% (12/44) for group 2 (Figure 2). These two groups did not differ statistically significantly (p = 0.75).
Kaplan-Maier curves show decreased probability of overall survival in patients with stage III AJCC, which is 28 in 3-year observation (Figure 3). In patients with stage I and II overall survival was 87% (p < 0.001).
We also analyzed the influence of complications on overall survival. There were no statistically significant differences between groups of patients with no complications, patients with Clavien-Dindo I–II complications and patients with Clavien-Dindo III–IV complications (p = 0.22).
Discussion
Our study showed that compliance to the ERAS protocol positively impacts short-term outcomes, but it does not influence 3-year survival. The only factor that worsens the patient’s prognosis is the stage of the disease. This is to our best knowledge the first study investigating this problem.
Compliance to ERAS seems not to influence patient survival. Our findings are contrary to Gustafsson et al., who observed improved long-term outcomes in colorectal cancer surgery in patients with high compliance to the ERAS protocol [12]. Pisarska et al. also found benefit of adherence to the ERAS protocol, observing better overall survival in patients with at least 80% compliance [13]. However, it is not easy to explain the why ERAS could possibly improve oncological outcomes. Asklid et al. reported that balanced fluid therapy in the perioperative course also could improve 5-year survival [15]. The topic is still under investigation, and it is highly likely that better survival is a consequence of many marginal gains in the perioperative period.
The ERAS protocol improves short-term outcomes, diminishing the rate of postoperative complications [16–18]. Some authors suggest that complications may negatively impact long-term survival [19]. Wang et al. performed a meta-analysis in which they found that postoperative complications correlate with poor survival in patients with stage II and III of the disease [20]. However, in patients with stage I complications it had no impact on the oncological outcomes [20]. On the other hand, Climent reported the following risk factors for worse survival: male gender, stage III of the disease and D1 lymphadenectomy; complications however were not associated with worse long-term prognosis [21]. In our study, only stage III cancer was a risk factor for poor survival. However, we did not assess the type of lymphadenectomy, because D2 lymphadenectomy in our unit is performed routinely.
Patients with high compliance had a significant shorter length of stay in comparison to those with low compliance. This result are in line with many other studies, as shortening of LOS is one of the main benefits of the ERAS protocol reported in the literature. Li et al. in their meta-analysis of 6 randomized control trials confirmed the benefit also for patients undergoing gastrectomy for gastric cancer [22].
What is important is that the ERAS protocol has many different modifications. Implemented protocols vary, including between 12 and 25 elements [23–25]. In our department we use a 14-element protocol for gastric cancer, and 16 elements for colorectal procedures [13, 26]. However, most of the elements are common for all ERAS protocols.
In our study we decided not to include postoperative elements in ERAS adherence calculation. Also, in our high compliance group, we observed a significantly shorter length of hospital stay. Moreover, we observed fewer Clavien-Dindo II–IV complications in the high compliance group, although the data did not reach statistical significance. On the other hand, Aarts et al. found that postoperative components have the strongest impact on overall result [27]. Having said that, they still underline the significance of preoperative elements. Kehlet also stresses that core elements of ERAS improve the final outcomes [28]. We focused on pre- and intraoperative elements of ERAS, because they are mostly staff-dependent. Moreover, these elements influence the compliance with postoperative elements, which in this situation could be regarded as an outcome. It is also worth remembering that not only perioperative care but also proper surgical technique with D2 lymphadenectomy and neoadjuvant treatment are the basis of a good final outcome.
There are some limitations of our study. Firstly, our sample size is fairly small and some subgroups might be underpowered for adequate statistical analysis, especially in patients with Clavien-Dindo grade III and IV complications. Secondly, we also used the national personal identification number database to gather data on overall survival, which allows us to access only date of death but not information whether the death was cancer-specific. Next, the impact of the learning curve of laparoscopic gastrectomy has to be taken into consideration due to the complexity of the procedure requiring a significant number of cases for proficiency [29]. That could be a possible source of bias in the early stages of the study. Finally, we do not have complete information about adjuvant therapy, since some of our patients chose the treatment in other oncological centers.