Introduction
Hirschsprung’s disease (HD) is one of the most common and severe diseases treated with pediatric surgery [1]. The incidence is approximately 1/5000. Surgery is the only effective treatment method. Since the introduction of the laparoscopic technique into pediatric surgery, laparoscopic-assisted radical surgery for HD has demonstrated unique advantages, especially for long-segment HD [2, 3]. From May 2012 to May 2018, 31 cases of the laparoscopic Soave procedure for long-segment HD were completed in our hospital.
Material and methods
From January 2013 to May 2018, children with long-segment HD in our hospital were enrolled; the patients received rectal irrigations for 7–10 days after admission, and oral antibiotics were given for bowel preparation 1 day before the operation. All children underwent the laparoscopic Soave procedure. A 5-mm trocar was placed at the umbilicus for the laparoscope. The other two trocars for the forceps and ultrasonic scalpel were placed at the lateral right and the left rectus abdominis muscle at the umbilical level. A full-thickness rectal sample of the upper rectum was cut as an intraoperative frozen biopsy to confirm the diagnosis. The aganglionic segment was mobilized distally to 1–2 cm below the peritoneal reflection circumferentially and proximal to the bowel with a size similar to that of the normal bowel. Seromuscular samples of the proximal bowel with normal appearance were taken for frozen biopsy until ganglion cells were found. This procedure was continued for the proximal ganglionic bowel, which could be pulled deep into the pelvis without tension. Then, the procedure was continued with the anus operation. An oblique circumferential incision of the rectal mucosa was made, as follows: the incision of the posterior wall was 0.8 cm proximal to the dentate line, and the incision of the anterior wall was 1.5 cm proximal to the dentate line. Endorectal dissection was continued until the level of the laparoscopic dissection. A circumferential incision of the muscular cuff was made, and “V” resection of the posterior wall was performed. Then, the proximal bowel was pulled out of the anus without tension or torsion. The pneumoperitoneum was established again to check that there was no active bleeding and no torsion of the pulled colon. The aganglionic segment was removed. Coloanal anastomosis was performed. A tube approximately 5 cm in length was inserted into the anus for drainage and was retained for 3 to 7 days after the operation. Anal dilatation began 14 days after the operation and lasted for 3 months.
Results
In total, 31 cases were successfully treated, 25 males and 6 females. All the children had a history of delayed excretion of meconium and long-term constipation. Anorectal manometry indicated HD, and the barium enema study showed long-segment HD. No case had stoma before radical surgery. 1 patient underwent radical operation at the age of 1 month for difficulties with cleansing enemas, and 1 patient had frequent ventricular premature beats and required drugs for control and stabilization until the patient reached 2 years of age; the ages of the other 29 patients ranged from 4 months to 8 months.
The aganglionic segment was located in the sigmoid or descending colon in 17 patients, in the transverse colon in 7 patients, and in the ascending colon in 7 patients. The operation time was 150–240 min, with an average of 180 min; and the volume of bleeding was 3–12 ml, without blood transfusion. The length of the resected intestine was 26–48 cm, with an average of 37 cm.
Twenty patients excreted and defecated within 12–24 h after the operation, and 11 patients excreted and defecated within 24–48 h after the operation. The average hospitalization time was 8.7 days after the operation, and no immediate postoperative complications occurred. The daily defecation frequency was 10 times within 1 month, 3–5 times within 6 months and 1–2 times after 6 months postoperatively.
The patients were followed up for 12 to 36 months. There was almost no scar after the abdominal incision healed. There was no recurrence of constipation. There were 6 (19.3%) patients who had complications of HD-associated enterocolitis in the first 3 months postoperatively; 5 (16.1%) patients had soiling in the first year, which did not affect their daily life. There were 0 cases of adhesive bowel obstruction, 0 cases of anastomotic stenosis, and 0 cases of constipation.
Discussion
The laparoscopic approach in colorectal surgery has been widely used [4]. Smith et al. [5] first reported the laparoscopic-assisted Duhamel radical operation in 1994; Georgeson et al. [6] carried out the laparoscopic Soave operation in 1995, and then various HD radical operations under laparoscopy were reported successively. Since long or total colons are difficult to pull out through the anus, long-segment and total-colon HD are the best indications for laparoscopic-assisted surgery [7]. Our experience with the treatment of these cases is summarized here.
In this study no case had stoma before radical surgery. This may be mainly due to our technique of rectal irrigation. Rectal irrigation is an important part of the preoperative preparation [8] and should be emphasized, especially for long-segment HD. The aganglionic bowel is so long that intubation is difficult, which makes the procedure time-consuming and labor-intensive. Parents often fail to defecate daily, which results in the accumulation of feces. Therefore, after admission, daily rectal irrigation by experienced professionals is necessary until the old feces or fecal stones in the bowel are completely removed. Anal tubes can be retained if intubation is difficult. If the fecal stones are not easy to lavage, the patients can be injected with a 3 : 2 : 1 liquid (10 ml magnesium sulfate, 20 ml glycerol, 30 ml distilled water) into the anus, which can not only lubricate the bowel but can also soften the feces to gradually wash the fecal stone out. Guidance for the family members to massage the child’s abdomen in a clockwise pattern during the lavage can not only divert the child’s attention to reduce their discomfort but also promote the excretion of feces.
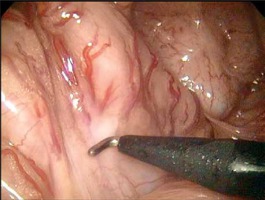
The following are our main experiences with the operation: (1) Trocar position: The abdominal wall of children is thin, and the supporting force is insufficient; thus, it is easy for the trocar to slip or be positioned too deep, which can greatly affect the operation. After inserting the trocar, suturing it on the abdominal wall can not only fix the trocar in place but can also help retract the abdominal wall to enlarge the operative field of view according to the need of the surgeons [9]; the whole colon can be easily freed by changing the position or changing the main surgical field (Photo 1). (2) Determining the extent of resection: Radical resection of the aganglionic segment and anastomosis of the ganglionic segment at the anus play a radical role in reducing the recurrence of constipation and HD-associated enterocolitis [10]. Before the operation, the colonography should be reviewed carefully, and the regions with narrow segments, transitional segments and dilated segments should be preliminarily judged (Photo 2). Intraoperative, laparoscopic examinations of the bowel including dilatation to near-normal thickness, intestinal wall changing from rough and thickened to thin and soft, changes in luster and elasticity, and the presence of a colonic pouch can be considered normal. A frozen biopsy of intestinal tissue with a normal appearance in the proximal transitional segment was performed. If the pathological reports indicated ganglion cells, the resection level could be determined. (3) Dissociation of the bowel: Placing the operating table in a head-down right-leaning position helps to fully expose the rectum, sigmoid colon and descending colon. The relevant anatomy begins at the junction of the rectum and sigmoid colon to 5 to 10 cm above the peritoneal reflection. When the rectosigmoid junction is lifted, the important bilateral structures, such as the ureter, vas deferens and iliac vessels, can be directly visualized, and the sigmoid mesocolon is flattened at the same time (Photo 3). Then, a hole was created in the mesocolon by electrocoagulation or an ultrasound scalpel. Along the hole, the mesocolon should be cut to closely hug the intestinal wall and extend downward to 1–2 cm below the peritoneal reflection (Photo 4), so as not to damage the ureter. The mesocolon cut should continue upward along the vascular arch until the expected resection level. Attention should be paid to protect the marginal artery. (4) Deloyer’s procedure: Long-segment HD often needs to be resected to the level of the hepatic flexure or the ascending colon. The remaining ascending colon is only approximately 10 cm long. It is not feasible to pull the normal bowel directly from the left lower abdomen to finish the coloanal anastomosis since it will lead to ischemic necrosis and anastomotic leakage due to excessive traction of the mesocolon. With Deloyer’s procedure for inversion, the ascending colon can be easily pulled into the pelvic space from the right lower abdomen and anastomosed to the rectum without tension [11]. Under laparoscopic direct vision, the bowel can be pulled outward and rotated counterclockwise to ensure that the extracted bowel is not twisted.
Photo 2
Barium enema of long-segment Hirschsprung’s disease, and the regions with narrow segments, transitional segments and dilated segments could be preliminarily judged

The drainage tube was wrapped with Vaseline gauze and was inserted into the anus immediately after the operation. The tube can dilate the anus, oppress pelvic hemostasis, reduce exudation, drain intestinal contents, ensure excretion of intestinal gases and stool, reduce contact with the anastomotic stoma, avoid anastomotic infection and enterocolitis, promote early healing of the anastomotic stoma, facilitate postoperative care, and avoid perianal erosion. The tube should be maintained for 3–7 days after the operation.
Long-segment HD is an independent risk factor for postoperative enterocolitis. Six cases of enterocolitis occurred within 3 months after the operation. Enterocolitis can manifest as fever, diarrhea, abdominal distention and even septic shock. Early diagnosis and timely treatment can effectively improve the prognosis of enterocolitis. Therefore, for patients with fevers after the operation, the occurrence of enterocolitis should be vigilantly monitored to eliminate problems such as anastomotic stoma. Anti-infection and infusion drugs are important treatments [12]. The defecation function recovered well and satisfactorily during the follow-up period.
The operation results of this study are satisfactory. The main limitation of this study is that the series is small, making detailed statistical analyses inappropriate. The follow-up time is short.