Introduction
Hydatid disease is a severe zoonotic disease most commonly found in the liver [1], followed by the brain, lungs, bones, and whole body. Hydatid cyst develops worldwide and is endemic in Eastern Europe, the Middle East, South America, Australia, and South Africa, especially in pastoral and farming regions [2]. Two main types of tapeworms causing human hydatidosis are: cystic echinococcosis (CE) caused by Echinococcus granulosus eggs and alveolar echinococcosis (AE) caused by Echinococcus multilocularis eggs. The treatments for liver hydatid are also diverse in clinical practice, such as percutaneous aspiration-injection-respiration (PAIR), medical benzimidazole treatment, and endoscopic treatment [3, 4]. However, surgery remains the only definitive treatment for large, active, symptomatic, or complicated hepatic hydatid cysts (HHC) [4]. Different surgical methods are adopted according to the type of hydatid disease. Cystic echinococcosis (CE) mainly includes total cystectomy, internal cystectomy, subtotal cystectomy, and so on. However, the safety and efficacy of traditional laparotomy and laparoscopy are unclear. This study aimed to explore the advantages and disadvantages of laparoscopy and traditional laparotomy with a meta-analysis.
Aim
This meta-analysis aimed to compare the efficacy and safety of laparoscopic versus traditional laparotomy in hepatic cystic hydatidosis.
Material and methods
Study design and literature search
A literature search was performed with the following online databases: CNKI, WanFang Database, CBM, PubMed, Embase, Medline, The Cochrane Library, Web of Science, and Data Service Platform (from the origin to December 2020). The search terms were “Echinococcosis”, “Hepatic”, “Hydatid Cyst”, “Laparoscopies”, “Laparoscopic Surgical Procedure”, “Peritoneoscopy”, etc. The “related articles” function was used to expand the search, and citations were considered for relevance. This paper is reported according to the PRISMA guidelines (Figure 1) [5].
Inclusion and exclusion criteria
Inclusion criteria were: (i) participants: patients with hepatic cyst hydatids who must undergo laparoscopic surgery or open surgery; (ii) study type is case-control study, prospective or retrospective cohort study comparing laparoscopic surgery and open surgery; (iii) outcomes: studies reporting the operation time, the incidence of postoperative complications (such as bile leakage and residual cavity infection), recurrence rate, postoperative time of abdominal drainage tube removal, recovery time of gastrointestinal function, etc.
Exclusion criteria were: (i) valid outcomes and data cannot be extracted from the studies; (ii) the surgical procedure did not include hepatectomy; in addition to surgery, patients have other interventions such as ultrasound radiofrequency ablation and PAIR; (iii) meta-analysis of recurrence rate was performed excluded without mention about albendazole studies. (iv) literature with a small number of cases (total number of cases ≤ 15); (v) unable to obtain the full text; (vi) repeated literature.
Study selection
Two researchers (ZW HHZ) independently reviewed the titles and abstracts of studies identified by the literature search. In order to improve the sensitivity, records were only deleted if both reviewers excluded records at the title screening level [6]. In case of differences, a third researcher decided. In the case of insufficient data, the original experimental materials were obtained by trying to contact the authors.
Quality assessment
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of included studies. The quality control and bias assessment were performed independently by 2 investigators (ZW and HHZ). NOS score > 7, 7 ≥ NOS score > 5 and NOS score ≤ 5 indicated good quality, fair quality, and poor quality, respectively. Disagreements were resolved through group discussion with another investigator [7] (Table I).
Table I
Risk of bias assessment
| References | Selection | Comparability Comparability of cohorts on the basis of the design or analysis* | Outcome | Score | |||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Assessment of outcome | Was follow-up long enough for outcomes to occur? | Adequacy of follow-up of cohorts | |||
| Gokhan Yagci et al. [9] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| Jian Zhong MA et al. [10] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| Qi Ming Mu et al. [11] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| Peng Yang et al. [12] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| Mehmet Bayrak et al. [13] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| TuerhongJiang Tuxun et al. [14] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| Fatin R. Polat et al. [15] | – | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 6 | |
| Azadeh Jabbari Nooghabi et al. [16] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| K. A. Bhadreshwara et al. [17] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | ⋆ | 9 |
| Nilesh J. Patel et al. [18] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 8 |
| Haitao Li et al. [19] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 7 | |
| Huseyin Kazim Bektasoglu et al. [20] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆⋆ | ⋆ | ⋆ | 8 | |
| Ilhan Ece et al. [21] | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | ⋆ | 7 | |
Data extraction
The following data were extracted from the papers: author, country, year of publication, type of literature, sample size, and age of patients, surgery-related indicators such as time to surgery, the recovery time to gastrointestinal function, complications (bile leak, biliary fistula, incisional wound infection, residual cavity infection), length of stay, hospitalization fee, time to abdominal drainage tube removal, and the number of recurrent cases.
Statistical analysis
This meta-analysis was conducted in accordance with the recommendations of the Cochrane Library and PRISMA guidelines [8]. Statistical analyses of the data were conducted using the RewMan 5.3 software. Two classification variables were expressed by odds ratio (OR) and 95% confidence interval (CI). Continuous variables were expressed by standardized mean difference (SMD) and 95% CI. According to I2 value, the heterogeneity between different studies is low when tested with the fixed-effect model, I2 < 50%; I2 ≥ 50% suggests that the heterogeneity between studies is high. The causes of heterogeneity were analyzed, and the pooled estimates were calculated using random-effects models to take into account potential inter-study heterogeneity and to adopt a more conservative approach [6]. The obvious clinical heterogeneity was treated by subgroup analysis, sensitivity analysis, or descriptive analysis. Statistical significance was considered when p-values < 0.05. A funnel chart was used to evaluate the publication bias, and the biased funnel chart is shown and explained in this paper.
Results
Literature search and selection
A total of 13 cohort studies were included. The flowchart of the literature search and the study selection process is shown in Figure 1.
Study characteristics
Basic characteristics of the included studies are shown in Table II [9–21]. 11 articles were retrospective cohort studies and 2 articles were prospective cohort studies, were published between 2005 and 2020, with sample sizes ranging from 19 to 332.
Table II
Basic characteristics of included studies
| First author | Country | Year | Type | Patients, n | Lap. patients, n | OS patients, n | Male, n | Female, n | Age | Surgical method |
|---|---|---|---|---|---|---|---|---|---|---|
| Gokhan Yagci [9] | Turkey | 2005 | Retrospective | 211 | 30 | 181 | Lap (23) OS (–) | Lap (7) OS (–) | Lap (36.0 ±6.5) OS (34 ±7.833) | Cystotomy/partial cystectomy |
| Jian Zhong Ma [10] | China | 2014 | Retrospective | 76 | 26 | 50 | Lap (16) OS (31) | Lap (10) OS (19) | Lap (59.200 ±6.865) OS (56.730 ±8.793) | Partial cystectomy |
| Qi Ming Mu [11] | China | 2018 | Retrospective | 83 | 43 | 40 | Lap (29) OS (25) | Lap (14) OS (15) | Lap (59.5 ±6.7) OS (58.9 ±7.2) | Partial cystectomy |
| Peng Yang [12] | China | 2020 | Retrospective | 56 | 19 | 37 | Lap (5) OS (18) | Lap (14) OS (19) | Lap (38.8 ±12.9) OS (41.0 ±12.9) | Cystotomy |
| Mehmet Bayrak [13] | Turkey | 2019 | Retrospective | 60 | 37 | 23 | Lap (11) OS (9) | Lap (26) OS (14) | Lap (38 ±15) OS (48.5 ±18.5) | Cystotomy/partial cystectomy |
| Tuerhongjiang Tuxun [14] | China | 2014 | Retrospective | 332 | 50 | 282 | Lap (–) OS (–) | Lap (–) OS (–) | Lap (–) OS (–) | Cystotomy/partial cystectomy |
| Fatin R. Polat [15] | Turkey | 2012 | Retrospective | 19 | 7 | 12 | Lap (3) OS (4) | Lap (4) OS (8) | Lap (31.8 ±9.3) OS (30.7 ±7.7) | Cystectomy |
| Azadeh Jabbari Nooghabi [16] | Iran | 2015 | Prospective | 73 | 37 | 36 | 24 | 49 | Lap (35.03 ±14.04) OS (43.03 ±17.96) | Partial cystectomy |
| K. A. Bhadreshwara [17] | India | 2015 | Retrospective | 42 | 21 | 21 | Lap (7) OS (8) | Lap (14) OS (13) | – | Cystotomy/partial cystectomy |
| Nilesh J. Patel [18] | India | 2016 | Prospective | 36 | 16 | 20 | 20 | 16 | – | Partial cystectomy |
| Haitao Li [19] | China | 2014 | Retrospective | 22 | 15 | 7 | Lap (7) OS (5) | Lap (8) OS (2) | Lap (39.6 ±14.97) OS (38.4 ±13.90) | Cystectomy |
| Huseyin Kazim Bektasoglu [20] | Turkey | 2019 | Retrospective | 71 | 23 | 48 | Lap (11) OS (25) | Lap (12) OS (23) | Lap (39.4 ±19.1) OS (41 ±15.4) | Cystotomy/partial cystectomy |
| Ilhan Ece [21] | Turkey | 2017 | Retrospective | 130 | 38 | 92 | Lap (12) OS (34) | Lap (26) OS (58) | Lap (44.8 ±11.3) OS (48.1 ±12.1) | Partial cystectomy |
Study quality assessment
Risk of bias among the cohort studies was assessed with NOS. The results showed that 10 studies were graded as good quality [8–13, 15–17, 19] and the remaining 3 studies were graded as fair quality. The overall score of the NOS was 101 of 117 (86%), which is considered to represent an overall high quality. Details of the quality assessment are shown in Table I.
Meta-analysis results
Summaries of meta-analysis outcomes are presented in Table III.
Table III
Some conclusions about the meta-analysis
Meta-analysis of operation time
In this study, a total of 9 articles mentioned operation time, involving 868 patients, laparoscopy group (n = 281), and traditional open group (n = 587). The results of the heterogeneity test using standardized mean difference (SMD) were as follows: I2 = 97% > 50%, p < 0.00001. Considering that the source of heterogeneity was related to surgical techniques and proficiency in different countries, random-effect meta-analysis was used. The results showed that SMD = –0.18, Z = 0.36, 95% CI: –1.19–0.83, p = 0.72 > 0.5, which were not statistically significant. No significant difference was found in laparoscopic operation time between the laparoscopic operation group and the traditional open group (Figure 2 A).
Figure 2
Summary of the meta-analysis outcomes comparing laparoscopic and open surgery. A – Operation time. B – Length of hospitalization stay. C – Hospitalization fee. D – Gastrointestinal function recovery time. E – Recurrence rate. F – Postoperative time of abdominal drainage tube removal. G – Total complication rate. H – Biliary leakage and biliary fistula complications. I – Incision infection with complications. J – Residual cavity infection of complications


Meta-analysis of postoperative outcomes
When compared with the traditional open surgery group, the laparoscopic surgery group showed a significantly shorter length of hospital day (p < 0.00001, 95% CI: (–1.06, –0.70), I2 = 18%) (Figure 2 B). However, regarding hospitalization fee (p = 0.04 < 0.05, 95% CI: (0.17, 5.21), I2 = 97%), laparoscopic surgery is higher than that of traditional open surgery (Figure 2 C). Recovery of gastrointestinal function was reported by 3 authors; the laparoscopic surgery group can promote postoperative gastrointestinal function recovery (p = 0.0004, 95% CI: (–2.36, –0.69), I2 = 85%) (Figure 2 D).
Due to albendazole treatment being important for recurrence assessment, we excluded studies that did not mention taking albendazole (Table IV); a total of 6 articles were included finally (p = 0.45, 95% CI: (0.50–4.63), I2 = 0%, OR = 1.53) (Figure 2 E), postoperative time of abdominal drainage tube removal (p = 0.10, 95% CI: (–2.15, 0.19), I2 = 92%) (Figure 2 F).
Table IV
Follow-up time and oral albendazole
| Postoperative follow-up time [months] | |||
|---|---|---|---|
| Study | Laparoscopic | Open | Whether to take albendazole |
| Huseyin Kazim Bektasoglu [19] | 17 | 21.7 | All patients were treated with albendazole (10 mg/kg) 2 to 3 weeks prior to the operation and three to 6 months following the operation |
| Ilhan Ece [20] | 33.2 | 33.2 | Patients received oral 10 mg/kg albendazole for 10 days before surgery. After surgery, albendazole was administered for three cycles in the same dosage. A cycle consisted of a 3-week period of medication and 1-week gap between two cycles |
| K. A. Bhadreshwara [16] | 24.2 | 28.4 | Patients were given albendazole treatment 10 mg/kg/day for 4 days preoperatively |
| Mehmet Bayrak [12] | 21.3 | 21.3 | All patients were treated with albendazole (10 mg/kg), 7 days before surgery, and this medication was continued postoperatively for 2 months |
| Nilesh J. Patel [17] | 15 | 15 | All the patients were given Tab. albendazole in 10 mg/kg dose for 2 weeks before surgery, post operatively for 4 weeks |
| Tuerhongjiang Tuxun [13] | 48 | 48 | Preoperative antiparasitic albendazole with a dosage of 10 mg/kg/day for continuous 7 days was administered |
In postoperative overall complication analysis, we observed that the test for heterogeneity among studies was not statistically significant (p = 0.03, I2 = 48%), so the fixed-effects model was used. The combined results based on the above studies showed that the postoperative total complication rate in the laparoscopy group was significantly lower than that in the traditional open surgery group (p < 0.00001, OR = 0.31; 95% CI: (0.21–0.46)) (Figure 2 G). Nevertheless, the biliary leakage (p = 0.09, OR = 0.60, 95% CI: (0.33–1.09), I2 = 0%) and the biliary fistula (p = 0.79, OR = 0.90, 95% CI: (0.39–2.05), I2 = 23%) showed no significant difference between laparoscopic surgery and traditional open surgery (Figure 2 H).
In addition, we also compared some complications about infections. The results revealed that the probability of incision infection after laparoscopic surgery is lower than after traditional open surgery (p = 0.001, OR = 0.29, 95% CI: (0.14–0.61), I2 = 0%) (Figure 2 I). However, complications of residual cavity infection were not statistically significant (p = 0.40, OR = 0.76, 95% CI: (0.39–1.45), I2 = 0%) (Figure 2 J).
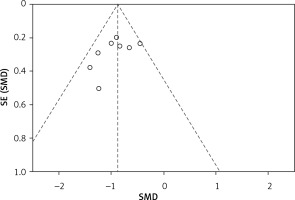
Publication biases
The funnel plot was used to investigate publication bias in this study, and the funnel plot symmetry indicated no publication bias. Taking the length of hospitalization stay funnel chart as an example (Figure 3), the funnel chart is roughly symmetrical, so the conclusion of the meta-analysis is reliable.
Discussion
At present, surgery is the main treatment for hepatic cystic hydatidosis; the objective of surgical treatment for cystic echinococcosis is to remove the parasitic tissue as completely as possible [22]. With the development of surgical techniques, laparoscopy has also been used in the field of liver hydatids. Some authors opine that the efficacy and safety of laparoscopy for hepatic hydatids are unclear [23]. However, at present, most of the published clinical studies are retrospective, and there is a lack of multicenter large-sample RCTs. Hence it is difficult to draw accurate conclusions on the clinical efficacy of laparoscopic surgery for hepatic cystic hydatidosis. Therefore, our meta-analysis was conducted to systematically review the published literature and evaluate the efficacy and safety of laparoscopic versus traditional laparotomy [24]. In our meta-analysis we found that laparoscopy is superior to the traditional open surgery in terms of length of hospital stay, the recovery time of gastrointestinal function, total complications, and the risk of incision infection. In addition, we think laparoscopy can achieve the same clinical effect as laparotomy.
According to our meta-analysis, there was no significant difference between laparoscopic surgery time and traditional open abdomen surgery time. But some authors also mention that open surgery is the main method in the operation of hepatic cystic hydatidosis, which leads to the problem of unskilled laparoscopic procedures. There is a lack of tacit understanding between operators. Therefore, it is necessary to set up a special professional group for laparoscopic surgery for hepatic echinococcosis. Operators must undergo formal laparoscopic training, have some experience in laparotomy, and try their best to master the skills of the ultrasonic scalpel and other instruments. In addition, the heterogeneity between studies is high, making it difficult to generalize their clinical value. In addition, longer surgical times may have little impact on clinical outcomes [25].
The postoperative recurrence rate is an important aspect in evaluating the surgical effect. According to previous articles, some studies [8, 12, 13, 16, 20] conclude that laparoscopy could reduce the recurrence rate of hepatic hydatid, while Hichem Jerraya [26] also pointed out that the risks of intraperitoneal leakage and spread of hydatid cyst rupture in laparoscopic surgery are higher than those in laparotomy. Therefore, this also makes our meta-analysis necessary. It can be seen from our included studies that the recurrence rate of laparoscopic surgery is 3% (6/185), and that of traditional open surgery is 2% (10/486). But our meta-analysis concluded that there was no significant difference in postoperative recurrence between laparoscopy and open surgery. So we concluded that there was no difference in recurrence rates between laparoscopic and open surgery. There are some ways to further reduce the recurrence rate, such as Seven et al. [27] with a special umbrella trocar that allows the cyst to be attached to abdominal walls, thus reducing the risk of spillover. Some studies indicate that at least 4 weeks of albendazole before liver hydatid surgery can reduce the viability of the cyst and the pressure in the capsule [28, 29], further reducing the risks of rupture and spillover during the operation. Kapan et al. [30] also suggested that routine oral administration of albendazole after operations can reduce the postoperative recurrence rate.
Although in terms of the removal time, our study has no statistical significance, from the three articles we included, we can see that laparoscopy has the advantage in the days of postoperative removal of the abdominal drainage tube. Conventional abdominal drainage plays an essential role in collecting postoperative peritoneal effusion, which is helpful to diagnose intra-abdominal bleeding and biliary fistula [31–33]. Combined with the magnification effect of the endoscope, operations can be more refined. Some small blood vessels and the biliary tract can be treated properly, significantly reducing intraoperative bleeding, postoperative biliary fistula, residual cavity effusion, and residual cavity infection after the operation [11].
Brooke-Smith et al. [34] defined bile leakage as fluid with an elevated bilirubin level in the abdominal drain or intra-abdominal fluid on or after post-operative day three or the need for radiological intervention (i.e. interventional drainage) owing to biliary collections or re-laparotomy due to biliary peritonitis. The elevated bilirubin level in the drain or intraabdominal fluid is defined as a bilirubin concentration at least three times higher than the serum bilirubin level measured at the same time. Tuxun et al. [35] found that the incidence of bile leakage in 914 patients with laparoscopy treatment of hepatic echinococcosis was 6.24%. In this study, the bile leakage rate was 5.1% in the laparoscopy group and 9.6% in the open surgery group. Considering that the laparoscopic lens can fully explore the cyst cavity, it is easier to find small bile leakage.
In the formation of the biliary fistula the hydatid cyst can oppress the surrounding liver tissue and then the intrahepatic bile duct when expanding in the liver, pressing part of the bile duct into the cyst cavity for a long time [36]. Saylam [37] mentioned that white blood cells (WBC), direct bilirubin level, alkaline phosphatase (ALP), and cyst diameter are important independent predictors of biliary fistula. An important method to deal with biliary fistula is to find it before and during the operation. Endoscopic retrograde cholangiopancreatography (ERCP) is a safe and effective method to deal with biliary complications of hepatic echinococcosis. Preoperative ERCP can find the obstruction of biliary, bile duct stricture, and an abnormal pathway between the bile duct and cyst, thus reducing the incidence of postoperative biliary fistula. In addition, the size of the cyst has been identified as an important predictor of morbidity and mortality [38].
The management of the residual cavity after the hydatid cyst removal of the liver remains a matter of contention, with most authorities indicating external tube drainage (ETD) and omentoplasty (OP) as the procedures of choice [39]. Because of the high absorptive capacity of the omentum and its ability to fill the residual cavity, omentoplasty is recommended for the treatment of hepatic hydatid cysts, both complicated and uncomplicated [40]. It is considered that residual cavity infection may be related to the inadequate drainage of pus and cyst fluid, the insufficient blood supply of the residual cyst, intraoperative and postoperative biliary leakage and biliary fistula, and the general condition of the patient. Therefore, factors such as setting the personal operation plan for patients according to their conditions, conducting effective postoperative abdominal drainage, and reducing the occurrence of intraoperative and postoperative biliary fistula can reduce the occurrence of residual cavity infection.
Regarding the strengths of our study, firstly, this is probably the first systematic review and meta-analysis for comprehensive analysis of laparoscopic and open surgery for hepatic cystic hydatidosis in English. Secondly, in comparison to a meta-analysis published in 2017 [41], we came to a different conclusion that laparoscopic treatment of liver hydatid is significantly lower than traditional laparotomy in terms of overall post-operative complications (p < 0.00001, OR = 0.31; 95% CI: (0.21–0.46)). Thirdly, the number of available studies and the sample size were large, which make the results more convincing. However, our study still has limitations. Firstly, we found that the operation time, gastrointestinal function recovery time, postoperative time of abdominal drainage tube removal and the hospitalization fee have higher heterogeneity. We attempted to find the source of heterogeneity by subgroup analysis and sensitivity analysis. However, there were many sources of heterogeneity in this analysis, so no sources of heterogeneity were found [24]. We considered the reasons for the heterogeneity, including surgical techniques, local medical conditions, location and size of cystic hydatidosis and so on. Secondly, for hepatic cyst hydatid patients, liver resection is rarely used in clinical practice, cystotomy/partial cystectomy being more common, so there are few clinical comparative studies, and hence we did not include it. In addition, all studies included in this meta-analysis were cohort studies. The lack of randomized trials limits the validity of our findings.
Conclusions
Laparoscopy is superior to traditional open surgery in terms of length of hospital stay, the recovery time of gastrointestinal function, total complications, and the risk of incision infection. No significant difference in postoperative recurrence between laparoscopy and open surgery was found. In addition, we think laparoscopy can achieve the same clinical effect as laparotomy. However, the reliability and validity of our conclusion need to be verified by more RCTs.