Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
UROLOGY / CLINICAL RESEARCH
Laparoscopic versus open pyeloplasty in children: experience of 226 cases at one centre
1
Department of Paediatric Surgery and Urology, Medical University of Wroclaw, Wroclaw, Poland
2
Department of Endocrinology, Diabetology and Isotope Therapy, Medical University of Wroclaw, Wroclaw, Poland
Submission date: 2019-02-14
Final revision date: 2019-03-30
Acceptance date: 2019-04-08
Online publication date: 2019-04-12
Publication date: 2020-05-26
Arch Med Sci 2020;16(4):858-862
KEYWORDS
laparoscopychildrenMinimal invasive surgeryhydronephrosisPediatricureteropelvic junction obstructionpyeloplastyUPJlumbotomyminimally invasive surgerypaediatric
TOPICS
ABSTRACT
Introduction:
The aim of the study was to compare the efficacy of laparoscopic versus open dismembered pyeloplasty in children.
Material and methods:
Two hundred and twenty-six Anderson-Hynes pyeloplasties were performed, out of which 131 by open access (OP) and 95 by laparoscopic access (LP). Retrospective analysis of data was performed. The median follow-up was 3 years for LP patients and 6 years for OP patients (p < 0.05).
Results:
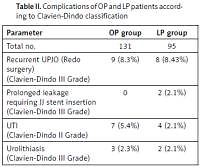
Success was achieved in 87 (91.57%) patients who had LP surgeries and in 121 (91.7%) patients who had OP (p > 0.05). Eight patients in the LP group and nine in the OP group required another surgery because of recurrent UPJO, and one patient in the OP group required a nephrectomy. The median operating time was 125 min (range: 70–225) for LP surgeries and 90 (40–200) for OP surgeries (p < 0.05). In the last 30 LP procedures, operation time decreased to a median of 95 min. Improvement in ultrasound analysis of the kidney was achieved in 89.06% of patients who had LP and 82.35% of patients who had OP. A stable or better function of the kidney in diuretic renography was achieved in 87.5% of patients in the LP group and 96.15% of patients in the OP group.
Conclusions:
Laparoscopic and open pyeloplasty is a highly efficient procedure employed to treat UPJO in children with comparable success rates in both groups. In experienced hands, it is possible to reduce the LP operation time to that comparable to the OP group.
The aim of the study was to compare the efficacy of laparoscopic versus open dismembered pyeloplasty in children.
Material and methods:
Two hundred and twenty-six Anderson-Hynes pyeloplasties were performed, out of which 131 by open access (OP) and 95 by laparoscopic access (LP). Retrospective analysis of data was performed. The median follow-up was 3 years for LP patients and 6 years for OP patients (p < 0.05).
Results:
Success was achieved in 87 (91.57%) patients who had LP surgeries and in 121 (91.7%) patients who had OP (p > 0.05). Eight patients in the LP group and nine in the OP group required another surgery because of recurrent UPJO, and one patient in the OP group required a nephrectomy. The median operating time was 125 min (range: 70–225) for LP surgeries and 90 (40–200) for OP surgeries (p < 0.05). In the last 30 LP procedures, operation time decreased to a median of 95 min. Improvement in ultrasound analysis of the kidney was achieved in 89.06% of patients who had LP and 82.35% of patients who had OP. A stable or better function of the kidney in diuretic renography was achieved in 87.5% of patients in the LP group and 96.15% of patients in the OP group.
Conclusions:
Laparoscopic and open pyeloplasty is a highly efficient procedure employed to treat UPJO in children with comparable success rates in both groups. In experienced hands, it is possible to reduce the LP operation time to that comparable to the OP group.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.