Dear Editor,
In recent years, ultrasonography has gained unmatched importance in medical practice. After the initial use for central vascular access placement and regional anaesthesia, its application has expanded to airway, ocular, abdominal, lung and cardiac ultrasound, with the concept of point of care ultrasound (POCUS) gaining acceptability and applicability in the most diverse situations. In fact, it has recently been acclaimed as the fifth pillar to bedside evaluation [1].
Performing a POCUS-guided eva-luation has proved to be of value in emergency medicine, with studies demonstrating improved diagnosis and better outcomes [2]. Similarly, in critical care, systematic ultrasound evaluation has been shown to decrease the use of conventional diagnostic imaging tools and time on mechanical ventilation and improve the management of fluid therapy [3]. Recognition of the benefit of ultrasound evaluation in the perioperative period has been increasing. In fact, the need to master clinical ultrasound evaluation has led the Canadian anaesthesiology academic centres to issue recommendations regarding the scope of practice and required training for perioperative POCUS [4].
Despite numerous studies reporting the usefulness of pre-, intra- and postoperative ultrasound, the decision to use it is considered based on individual patient assessment. However, similarly to what happens in critical care where the addition of ultrasound evaluation for all patients has been shown to be beneficial, the authors suggest that this evaluation should be guided by a protocol and performed in nearly all patients scheduled to undergo surgery, as well as for all patients submitted to urgent surgery. Nevertheless, considering the limited beneficial impact of this protocol’s application to generally healthy patients (ASA I), the decision to do so should be individualized and ultimately made by the anaesthesiologist.
Unlike common POCUS application, where there is a directed question for which the ultrasound assessment is used to answer, we propose the concept of Minute Zero assessment. It consists of an initial ultrasound evaluation, ideally performed in the preoperative setting. This provides an image of the patient’s baseline status, providing a basis for comparison with subsequent evaluations. Moreover, if there is room for patient optimisation, this can be done before the surgical insult, potentially improving surgical outcomes and minimising complications that would have ensued in case of failure to recognise the hindered patient situation. With Minute Zero evaluation we aim to have a global picture of patients’ clinical condition and not only to answer targeted questions.
Minute Zero Protocol (Figure 1)
Lung ultrasound. Evaluate in each hemithorax the presence of:
Cardiac ultrasound. Evaluate:
Abdominal ultrasound. Evaluate:
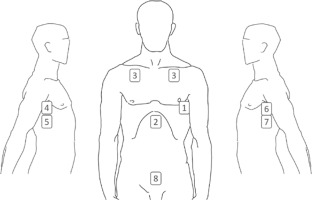
FIGURE 1
1 – Echocardiogram four-chamber view. 2 – Subcostal and IVC. 3 – Lung ultrasound anterior region. 4 – Lung ultrasound – right axillary midline and PLAPS point. 5 – Morrison’s pouch. 6 – Lung ultrasound – left axillary midline and PLAPS point. 7 – Splenic renal pouch. 8 – Pouch of Douglas
There are two critical moments in which patients should be evaluated: upon arrival at the operating room – pre-operative Minute Zero; and upon arrival at the post-anaesthetic care unit (PACU) – PACU Minute Zero. The screening protocol before surgery should include lung, cardiac and abdominal ultrasound, including gastric content evaluation, which can be replaced in the PACU Minute Zero protocol for vesical ultrasound. This simple assessment could help to diagnose cystocerebral syndrome, a commonly forgotten cause of agitation and delirium in the PACU [5].
This is a simple, safe, fast and easily reproducible protocol. This evaluation can and should be repeated whenever deemed necessary by the anaesthesiologist. The findings should be registered for posterior comparison with subsequent evaluations, also preventing the loss of information during the transfer of care (Table 1).
TABLE 1
Minute Zero questionnaire to register evolution of patient’s ultrasound parameters in the perioperative period
LUNG ULTRASOUND
Lung ultrasound is a simple and valuable resource for pulmonary and ventilatory function assessment. In fact, it has an elevated sensibility and specificity for the diagnosis of several entities such as pneumothorax, pleural effusion, alveolar consolidation, atelectasis, pulmonary oedema and alveolo-interstitial syndrome [6].
Numerous systematic approaches to pulmonary ultrasound have been previously reported. The evaluation described by Lichtenstein, the Bedside Lung Ultrasound in Emergency (BLUE) protocol [7], suggests the use of 3 points in each hemithorax: the upper and lower BLUE points and the posterolateral alveolar and/or pleural syndrome point (PLAPS point). The BLUE protocol is a fast approach that warrants identification of the cause of acute respiratory failure considering ultrasound profiles.
Because patients in the preoperative and PACU settings are nearly always in the supine position, the PLAPS point may be difficult to access since it is necessary to place the probe as posteriorly as possible. The pulmonary scan proposed should be applied in each hemithorax and registered.
Lung ultrasound in the periope-rative period, along with cardiac ultra-sound, allows assessment of the causes of respiratory distress, procedural complications or worsening of patient pathologies [8, 9]. This knowledge will allow one to optimise patient status, promptly diagnose possible life-threatening situations such as intraoperative pneumothorax, and guide the therapeutic approach, considering the need for diuretics, respiratory kinesiotherapy or non-invasive ventilation in the PACU [10]. This results in fewer postanaesthetic pulmonary complications and faster recovery of normal lung function, along with earlier recognition of ensuing complications [11, 12].
CARDIAC ULTRASOUND
The peri-operative period can be challenging for a patient who is already hampered. Echocardiography provides a valuable insight to cardiac function and haemodynamic status [13, 14]. In fact, the use of cardiac ultrasound is expanding, with the concept of focus cardiac ultrasound (FoCUS) examination proposed by the European Association of Cardiovascular Imaging being progressively applied by anaesthesiologists, as well as intensivists, emergency medicine physicians and internal medicine [15].
The most widely used views are the parasternal long-axis, parasternal short-axis, subcostal and apical four-chamber (views used in the focus assessed transthoracic echocardiography [FATE] protocol) [15]. The authors suggest the preferential use of the subcostal and apical four-chamber views, given the amount of information provided for the minimum time spent. The evaluation of the IVC during spontaneous ventilation correlates well with intravascular volume status. IVC measurements of < 20 mm with inspiratory collapse correlate with intravascular volume depletion, whilst measurements > 20 mm with almost no respiratory variability indicate possible fluid overload [15].
Hence, cardiac ultrasound in the perioperative period enables one to appraise pre-induction volume status and haemodynamic evolution, assess ventricular function, valvular abnormalities, pericardial effusions, wall motion and contractility. Once more, this information gives the anaesthesiologist an insight into the patient status, allowing tailored therapy.
ABDOMINAL ULTRASOUND
After abdominal or pelvic surgery, most patients will present some amount of free intra-peritoneal fluid. Abdominal ultrasound at PACU Minute Zero is vital to initially evaluate these findings and estimate intra-abdominal fluid volume upon arrival. This makes it possible to monitor clinical evolution and to prematurely detect possible post-surgical complications.
For abdominal ultrasound evaluation, the authors propose three of the classic Focused Assessment with Sonography for Trauma (FAST) protocol windows [16]: hepatorenal recess or Morrison’s pouch, splenorenal recess or Gerota’s pouch and rectovesical recess or pouch of Douglas. The FAST protocol was developed to identify free intra-peritoneal fluid in the context of acute trauma. Similarly, surgical procedures can also be considered a trauma, with possible complications, namely bleeding, behaving similarly to blunt trauma.
For patients submitted to major abdominal or pelvic surgery, the presence or absence of intra-peritoneal fluid should be evaluated in each location and qualitatively measured at PACU Minute Zero by visualising small intraperitoneal fluid (yes or no) or by measuring the column of liquid at each specific location (Figure 2). However, the presence of small quantities of free fluid is normal in the context of surgery. In the context of aggravating haemodynamic status or suspected complication, the initial ultrasound evaluation can be compared with new assessments, conceivably evidencing an eventual increase in intra-abdominal fluid that should elicit intervention.
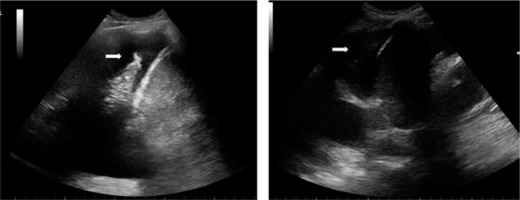
FIGURE 2
Postoperative assessment sonography in Douglas pouch view: the postoperative Minute Zero of an endometrial polypectomy where there was a uterine perforation evidenced by intraperitoneal free fluid. The initial column of fluid was measured and served for comparison with successive measurements and clinical monitoring

As described in many papers, the perioperative point of care ultra-sonography value is particularly evident in emergent cases and in unstable patients, since it provides useful information for decision making [14, 17, 18]. However, its scope of interest lies beyond complications or emergent situations. Perioperative clinical ultrasound can be performed as a complementary process for the initial assessment of surgical patients. Also, the Minute Zero assessment provides the baseline status of the patient to compare with subsequent evaluations.
In fact, a correctly employed Minute Zero evaluation with pulmonary, cardiac and abdominal ultrasound complements the physical examination and gives a global perspective of the patient’s haemodynamic and ventilatory status. Moreover, it can prematurely suggest complications before their clinical manifestation, enabling prompt action and prevention of clinical progression (Figures 3 and 4).
FIGURE 3
Preoperative Minute Zero: dilated IVC (star) and presence of multiple B lines (arrows) in each hemithorax in a patient admitted for cholecystectomy for acute cholecystitis. Restrictive fluid therapy was instituted
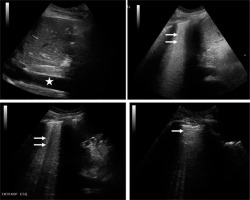
FIGURE 4
PACU Minute Zero: bilateral pleural effusion (arrows). Prompt action and prevention of clinical progression were possible
The Minute Zero protocol proposed is neither locked nor unchangeable. On the contrary, it should be constantly upgraded and open to other measurements. Effectively, in some cases, specific ultrasound parameters integrated in the FATE protocol, such as tricuspid annular plane systolic excursion (TAPSE), mitral annular plane systolic excursion (MAPSE) and ejection fraction (EF), could be calculated and added to the basic protocol to obtain more precise and relevant information [15].
Despite being a basic protocol, the usage of ultrasonography requires practice and knowledge of how certain pathologies translate into an ultrasound image and how to handle the ultrasound machine and the probe to acquire the best image possible. Investments in continuous education and acquisition of technical skills are mandatory for the success of a programme like this.
We believe that the implementation of a practical and routine protocol for ultrasound evaluation upon arrival at the operating room and at PACU admission constitutes a valuable supplement to the physical evaluation in the perioperative period.




