Mortality risk remains high in septic shock due to Staphylococcus aureus, which renders correct identification and treatment of the focus of infection mandatory for saving lives. While this organism frequently causes cardiac device infections and infective endocarditis [1], rare presentations are easily overlooked and require special attention.
An 82-year-old woman presented to our emergency room with clear signs of infection (C-reactive protein and procalcitonin elevated > 10× upper limit of norm). Her medical history was negative for any kind of infectious disease or implanted device, but she suffered from insulin-dependent diabetes. In spite of routine screening for the focus of infection (clinical exam, chest-X-ray, urine sampling) and early initiation of empiric antibiotic therapy (piperacillin/tazobactam) according to guidelines of the surviving sepsis campaign [2], she developed progressive circulatory deterioration and was admitted to our intensive care unit in septic shock later that day. Antibiotic therapy was escalated to combination therapy (+ ciprofloxacin) for septic shock, but again, screening for a focus of infection turned out negative. The next day, blood cultures returned positive for S. aureus – although without echocardiographic signs for endocarditis or a compatible thoracoabdominal infection on computed tomography (CT) scans. Antibiotic therapy was changed again to piperacillin/tazobactam and vancomycin with respect to the identified pathogen.
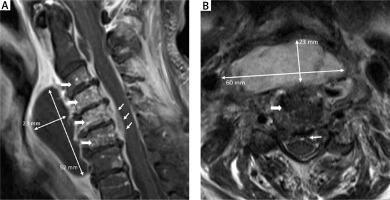
On careful secondary examination that second day, the patient’s hoarse voice prompted pharyngeal endoscopy. A considerable submucosal pharyngeal swelling was further evaluated using magnetic resonance imaging (MRI). Cervical MRI scans (Figure 1) revealed a 60 × 23 × 52 mm parapharyngeal abscess, multi-segment spondylodiscitis (wide arrows) and spinal cord compression (thin arrows). As a consequence of the focus identification, the patient underwent emergency neurosurgery with abscess drainage and laminectomy the same day – but unfortunately died 3 weeks later from this disease in spite of maximum therapy.
Figure 1
Cervical magnetic resonance imaging illustrating the dimensions of infection: T1-weighted gadoliniumenhanced sagittal section (A), T2-weighted cross-section at C4 (B). Wide arrows indicate spondylodiscitis (C3–C7), thin arrows demonstrate abscess dimensions (60 × 23 × 52 mm) and spinal cord compression (C4–C6) ↑ T2-weigted cross-section at C4, → T1-weigted gadolinium enhanced sagittal section.
Spondylodiscitis – especially of the cervical spine – is very rare, with an estimated incidence of 0.4–2.4/100,000 [3]. As in infectious endocarditis, hematogenic dissemination of S. aureus from other entry points (respiratory or urogenital tract, skin) is the most common pathogenesis [4], but often eludes identification. Diabetes mellitus is a common risk factor. Mortality risk is considerable at > 10% and especially high in patients with S. aureus bacteremia and septic shock [4].
Thus, this case highlights the importance of the quest for the focus of infection in septic shock caused by S. aureus. When an obvious focus is nonexistent, careful examnination of every abnormal clinical feature – such as a hoarse voice – can make the difference for any patient.



