The results observed when using non-invasive mechanical ventilation (NIV) in the management of acute respiratory failure are variable [1–3]. This variability can be attributed to the heterogeneity of the different groups of subjects, in which greater success is demonstrated when NIV is used in those with chronic obstructive pulmonary disease (COPD) and/or congestive heart failure exacerbated by infection [4, 5].
In daily practice, NIV has become a common treatment method for patients with acute respiratory failure (ARF), independent of the given aetiology [6, 7]. In clinical settings, when NIV is initiated in subjects with ARF, the ventilatory parameters have classically been determined based on clinical evaluation, blood gas measurement variations, tidal volume, minute volume, and, in some cases, flow and pressure monitoring from the mask to the ventilatory circuit [8]. In most cases, the conventional strategy for programming and setting ventilatory parameters has been based on elevations in pressure support levels with the individual titration of inspiratory pressure according to each subject [9, 10].
The bilevel positive airway pressure-spontaneous/timed (BiPAP S/T) with average volume-assured pressure support (AVAPS) ventilation strategy allows the use of a fixed preprogrammed volume, and this tidal volume remains fixed by specific changes in inspired pressures [11]. The ventilator approximates the volume delivered and adjusts its parameters in order to ensure the predetermined destination volume.
Only a few studies have demonstrated the applicability of this strategy in subjects with ARF and the results in these studies varied depending on the series and outcomes evaluated, such as tolerability, relief of dyspnoea, quality of life, and comfort [12, 13]. Therefore, this study was designed to evaluate the usage of BiPAP S/T – AVAPS in patients with ARF. The primary objective was to determine the percentage of success and failure (percentage of intubation) associated with the use of the BiPAP S/T – AVAPS ventilatory strategy. The second objective was to determine mortality, days of mechanical ventilation, length of hospital stay (in days), as well as predictors of success or failure.
METHODS
This is a single-centre prospective study and its methodology is based on a protocol originally developed by the authors [11]. All subjects included in the study were admitted between December 1, 2010 and January 1, 2014. This human study was approved by the Teaching and Research Committee of Santa Maria Clinic and received institutional approval: N/REF: 01/12/2010. Protocol/serial number 2011.14 (1). It adheres to the STROBE statement guidelines and was performed in accordance with the Declaration of Helsinki. The study’s clinical trial was registered at http://www.isrctn.com/10.1186/ISRCTN96455367 and the registry number is ISRCTN96455367, DOI: 10.1186/ISRCTN96455367. An informed consent form was signed by a surrogate if the subject lacked the autonomy necessary to consent.
Inclusion criteria
The subjects included were those who met the following criteria: (1) eighteen years old or older; (2) admitted to an intensive care unit (ICU); (3) diagnosed with ARF due to exacerbation of asthma, exacerbation of COPD, pneumonia, interstitial lung disease, congestive heart failure, and/or acute respiratory distress syndrome (ARDS).
The defining criteria for ARF were as follows: (a) ventilatory failure secondary to hypercapnia (PaCO2 > 45 mmHg, pH 7.35 or less); (b) inadequate oxygenation (PaO2 < 60 mmHg) breathing ambient air (SaO2 < 92%) with PaO2/FiO2 < 300 (mmHg) and severe dyspnoea (RR > 25 breaths per minute) with the use of accessory muscles [11].
Exclusion criteria
We excluded patients who presented any of the following: (1) face deformities; (2) upper airway obstruction resulting from trauma and/or surgery; (3) central nervous system alterations unrelated to hypercapnic encephalopathy; (4) pneumothorax, embolism, septic shock, or haemoptysis; (5) urgent intubation due to cardiorespiratory arrest and haemodynamic instability with systolic pressure less than 80 mmHg [11]; and (6) subjects with haemodynamic instability, excessive respiratory secretions, uncooperative or with agitated conduct, and recent upper airway surgery as well as those who were unable to use the interface device or who received NIV with do-not-resuscitate orders [11].
Clinical characteristics
Age, sex, and severity of disease were assessed using the APACHE II scoring system [11]. The main diagnosis that led to NIV and the number of affected lung quadrants according to chest X-ray were registered.
The subjects were categorised according to the aetiology of ARF: COPD, bronchial asthma, pneumonia, ARDS, congestive heart failure, and interstitial disease. The patients were also categorised according to the type of ARF: (1) hypercapnic ARF: obstructive diseases such as COPD and bronchial asthma; (2) de novo hypoxaemic ARF: pneumonia, ARDS, congestive heart failure, and interstitial lung disease.
Measurements
Arterial blood gases (ABG) were measured at baseline and then after 1 hour, 12 hours, and 24 hours of NIV use. The subjects were evaluated by a medical team with proper training and expertise in NIV.
We reported data on systolic blood pressure (SBP, mmHg), heart rate (HR), diastolic blood pressure (DBP, mmHg), respiratory rate (RR), programmed tidal volume, maximum programmed inspired positive airway pressure (IPAP, cmH2O), IPAP level (cmH2O), inspiratory time (IT) (s), expired positive airway pressure (EPAP) level (cmH2O), exhaled tidal volume (VTE) (mL), minute volume (Vmin), leakage, FiO2 (%), and number of affected lung quadrants (according to patients’ chest X-rays).
Programmed ventilator parameters
The methodology for this research is based on a protocol originally developed by the authors in 2013 [15]. The authors initially programmed the ventilatory parameters in the BiPAP S/T mode with AVAPS, using a maximum programmed IPAP of 20 cm H2O, a minimum IPAP of 12 cm H2O, and an EPAP of 6–8 cm H2O [11].
The researchers programmed the tidal volume considering 6–8 mL kg−1 of the ideal body weight (PBW) as follows: 55.5 ± 2.3 (height – 60 inches) = kg (PBW) for men and 45.5 ± 2.3 (height – 60 inches) = kg (PBW) for women. Additionally, the respiratory rate (RR) was 14–20 rpm, rise time was 300–400 ms, and inspiratory time (IT) was 0.8–1.2 s. Oxygen supplementation was added using a mask adapter to maintain the SaO2 above 90%.
Vmin, VTE, maximum IPAP, and leaks were managed using the ventilator’s software [11]. We used BiPAP Synchrony with AVAPS, as well as the Autotrak (Respironics Inc., Murrysville, Pennsylvania, USA) and a Mirage IV series of facemasks (Resmed, San Diego, California, USA) [11].
Decisions regarding adjustments of ventilator parameters were made at the discretion of the physician responsible for the patient and according to the degree of patient-ventilator asynchrony, respiratory frequency and comfort.
The following were the criteria for failure of NIV and need for intubation: (a) persistence of hypercapnic ventilatory failure as evidenced by an increase in basal PaCO2 and persistence of low pH; (b) persistent hypoxaemia as evidenced by PaO2 < 70 mmHg with SaO2 < 90%; (c) severe dyspnoea with tachypnoea (30–40 breaths per minute) and use of accessory respiratory muscles.
Discontinuation of NIV therapy
Ventilation was given continuously during the first 24 hours and in 3-hour periods afterwards, with periods without NIV depending on the tolerability of the patient. During these periods, the patient received therapy with an oxygen face mask.
Subjects were weaned off NIV when they reached clinical stability, which our team defined as: respiratory rate of less than 24 rpm, HR of 90 bpm, and SaO2 > 90% with inspired FiO2 percentage less than 35–40%.
NIV withdrawal
In accordance with the 2013 protocol, clinical stability was defined as: (1) RR < 25 rpm, (2) HR < 90 bpm, and (3) compensated arterial pH with SaO2 > 90% in ambient air or with a low flow of oxygen (< 3 L per minute) [11]. These parameters were measured during the periods without NIV and for a period of 24 hours.
Outcome measures
The primary outcome, which was either the success or failure (defined as endotracheal intubation) in the usage of NIV, was expressed as a percentage. The secondary outcomes included length of hospitalization (days), need for endotracheal intubation (percentage), mortality (percentage), and predictors of success or failure.
Statistical analysis
In accordance with the protocol, data with a Gaussian distribution and similar variance were analysed using Student’s t test for independent samples. The χ2 test or Fisher’s exact test was used for categorical variables with a non-normal distribution [11].
To establish the variables that are predictors of the failure of NIV. First, a multiple logistic regression analysis was used, with need for intubation as the dependent variable (the variable was dichotomous) [11]. Second, analysis of variances (ANOVA) with repeated measures within subject factors was used to establish the relationship between failure versus success of the different variables in the de novo hypoxaemic ARF groups. To determine the statistical significance a P-value of < 0.05 was used.
Statistical analysis was performed using MedCalc Statistical Software version 16.4.3 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2016).
RESULTS
Sixty-eight subjects were included in our study. The mean age of presentation was 71.1 ± 18.9 SD. The average programmed tidal volume AVAPS was 478.6 ± 69.6 SD. The mean APACHE II score was 15.4 ± 2.2 SD, and the mean number of affected lung quadrants according to chest X-rays was 1.7 ± 0.8 SD. The main comorbidities were as follows: no comorbidities 61 (89.7%), arterial hypertension 4 (5.8%), non-Hodgkin lymphoma 1 (1.4%) and diabetes mellitus type II plus arterial hypertension 2 (2.9%). The initial characteristics of the subjects are presented in Table 1.
TABLE 1
Characteristics of the study population (n = 68)
[i] Baseline characteristics of the study population. Values are presented as incidence (percentage) or mean ± standard deviation.
[ii] ARDS – acute respiratory distress syndrome, ARF – acute respiratory failure, BiPAP S/T – AVAPS – bilevel positive airway pressure-spontaneous/timed with average volume-assured pressure support, COPD – chronic obstructive pulmonary disease, EPAP – expired positive airway pressure, IPAP – inspired positive airway pressure, NIV – non-invasive ventilation, S/T – spontaneous/timed, Vmin – minute volume
The multiple logistic regression analysis showed that the variables predictive of failure (percentage of intubation) were as follows: number of affected lung quadrants on chest X-ray (OR: 4.23, 95% CI: 4.17–4.31; P < 0.001) and ARF precipitating disease (OR: 4.46, 95% CI: 4.43–4.51; P < 0.001). Data are presented in Table 2.
TABLE 2
Predictors of non-invasive mechanical ventilation failure
| Independent variables | OR | 95% CI | P-value |
|---|---|---|---|
| Number of affected lung quadrants on chest X-ray | 4.236 | 4.17–4.31 | < 0.001 |
| ARF precipitating disease | 4.465 | 4.43–4.51 | < 0.001 |
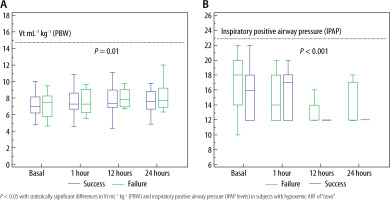
We found significant differences related to success or failure of NIV when data of the novo hypoxaemic ARF subjects were examined (ANOVA test). Data were analysed starting at baseline, at 1 hour, at 6 hours, and at 12 hours. A statistically significant difference was found in pH (P = 0.003), HCO3 (P = 0.008), HR (P = 0.008), and PaO2/FIO2 (P = 0.001), as seen in Table 3. Additionally, a significant difference was found in Vt mL−1 kg−1 (PBW) and inspired positive airway pressure (IPAP levels) (P < 0.05) (Figure 1).
TABLE 3
The variables predictive of success (n = 37) and failure (n = 20) of non-invasive mechanical ventilation, in patients with de novo hypoxaemic acute respiratory failure. Physiological and ventilatory parameters at baseline, 1 hour, 6 hours, and 12 hours
| Parameter | Baseline | 1 hour | 6 hours | 12 hours | P-value |
|---|---|---|---|---|---|
| pH | |||||
| Failure | 7.39 ± 0.07 | 7.38 ± 0.07 | 7.38 ± 0.08 | 7.37 ± 0.06 | 0.003* |
| Success | 7.43 ± 0.06 | 7.44 ± 0.07 | 7.44 ± 0.06 | 7.44 ± 0.05 | |
| pO2 (mmHg) | |||||
| Failure | 81.64 ± 13.3 | 94.17 ± 27.7 | 105.1 ± 27 | 102.6 ± 29.9 | 0.014* |
| Success | 76.1 ± 11.3 | 114.5 ± 34.3 | 118.2 ± 34.2 | 115.0 ± 34.5 | |
| HCO3 (mmol L−1) | |||||
| Failure | 22.8 ± 5.1 | 22.76 ± 5.5 | 23.1 ± 6.1 | 22.2 ± 4.9 | 0.008* |
| Success | 22.8 ± 4.3 | 24.1 ± 4.4 | 24.5 ± 4.3 | 26.3 ± 4.2 | |
| FiO2 (%) | |||||
| Failure | 0.42 ± 0.1 | 0.42 ± 0.1 | 0.46 ± 0.1 | 0.49 ± 0.1 | 0.001* |
| Success | 0.42 ± 0.1 | 0.40 ± 0.1 | 0.38 ± 0.1 | 0.36 ± 0.1 | |
| HR (heart rate) | |||||
| Failure | 97.8 ± 14.7 | 95.7 ± 17.1 | 90.2 ± 16.2 | 103.3 ± 20.7 | 0.008* |
| Success | 95.6 ± 16.5 | 86.1 ± 16.8 | 84.2 ± 14.2 | 86.4 ± 14.5 | |
| PaO2/FiO2 (mmHg) | |||||
| Failure | 199.7 ± 44.6 | 234.9 ± 98.7 | 228.3 ± 93.8 | 234.1 ± 112.7 | 0.001* |
| Success | 181.3 ± 33.7 | 289.4 ± 91.6 | 318.4 ± 106.4 | 321.6 ± 102.3 | |
| Levels of IPAP (cm H2O) | |||||
| Failure | 17.0 ± 3.5 | 14.7 ± 3.1 | 12.9 ± 1.3 | 14.1 ± 2.6 | 0.001* |
| Success | 15.7 ± 2.9 | 16 ± 3.2 | 12.1 ± 1.5 | 12.3 ± 1.7 | |
| Vt mL−1 kg−1 (PBW) | |||||
| Failure | 6.9 ± 1.6 | 7.7 ± 2.2 | 8.2 ± 1.5 | 8.6 ± 2.1 | 0.01* |
| Success | 7.0 ± 2.1 | 7.9 ± 2.5 | 8.0 ± 2.5 | 8.0 ± 2.6 | |
Furthermore, the total percentage of failure of NIV was 30.9% and the mortality rate was 20.6%. Subjects with the highest percentage of therapy failure belonged to the hypoxaemic ARF group or had pneumonia, ARDS, congestive heart failure, and/or interstitial lung disease, whereas patients with obstructive diseases such as COPD and bronchial asthma had a lower percentage of therapy failure. The duration of NIV therapy, length of stay in the ICU, length of hospital stay, and mortality are described in Table 4.
TABLE 4
Primary and secondary outcomes with acute respiratory failure of various aetiologies
DISCUSSION
In this study, BiPAP S/T – AVAPS was used in subjects with acute respiratory failure. To our knowledge, our study is the first to use the BiPAP S/T – AVAPS strategy in subjects with different types of ARF, which is an area that lacks broad descriptions of ARF management. Our results show that patients with hypercapnic ARF due to obstructive diseases (COPD and bronchial asthma) who receive therapy with BiPAP S/T – AVAPS present better outcomes than those with de novo hypoxaemic ARF who receive the same ventilation strategy.
The percentage of failure to NIV with BiPAP S/T – AVAPS in the group with hypercapnic ARF due to obstructive diseases (COPD and bronchial asthma) was 9% and 35% in those with de novo hypoxaemic ARF. Previous studies have demonstrated the usefulness of this ventilatory mode, especially in subjects with COPD and hypercapnic encephalopathy, where this mode was able to avoid the risk of reduced tidal volume and minute ventilation in some patients [11].
Other studies have obtained different results when using this ventilatory mode. Cao et al. [12]. reported positive results in their multicentre randomised controlled trial including 58 subjects with exacerbations of chronic pathologies such as COPD, asthma, bronchiectasis, and obstructive sleep apnoea syndrome. Ciftci et al. [13] reported a 76.4% success rate of NIV when this ventilatory mode was used in patients with COPD exacerbation.
As mentioned above, we found that the percentage of failure was greater in patients with de novo hypoxaemic ARF than in hypercapnic ARF. Moreover, the number of affected lung quadrants on chest X-ray and the ARF precipitating disease were both determinant factors of failure, particularly in patients with de novo hypoxaemic ARF. Consequently, we found a high percentage of failure, especially in subjects with de novo hypoxaemic ARF due to congestive heart failure (50%), pneumonia (42.4%), and ARDS (40%). Some studies report similar results in patients with de novo hypoxaemic ARF and NIV [14, 15].
The direct therapeutic options for hypoxaemic ARF are limited and mainly focus on minimizing ventilator-induced lung injury (VILI) [16]. Hence, the use of lower tidal volumes is the cardinal strategy to minimise this risk. However, it is difficult to maintain a low expiratory tidal volume in patients receiving NIV for hypoxaemic ARF, which is generally associated with NIV failure [17].
In this context, some aspects of the biomechanical properties of the respiratory system should be considered. Even though conduction pressure is currently a target to limit lung over-distension [18], it requires calculation of the plateau pressure or trans-pulmonary pressure. This is not convenient as it requires a stable inspiratory pause, and thus paralysis of the patient, for a correct measurement [19]. Some ventilator models allow plateau pressure to be measured by an inspiratory pause in pressure support or neurally adjusted ventilatory assist (NAVA) modes [20]. However, the plateau pressure within the airway does not consider the effect of the thoracic wall pressure on the distensibility of the lung. In this instance, the determination of the trans-pulmonary pressure, which is the pressure difference between the airway opening and the pleural space, would be the most appropriate, thus requiring the use of an oesophageal manometer [21]. In our management, we used BIPAP ST – AVAPS mode with the ventilator model BiPAP Synchrony with AVAPS, as well as the Autotrak (Respironics Inc., Murrysville, Pennsylvania, USA) in which the patient keeps breathing spontaneously and the inspiratory effort with pleural pressure drops during inspiration. Consequently, the conduction pressure measurement may not be active in respiration [22]. Ultimately, conduction pressure may not be helpful in patients who maintain active respiration and in those who have decreased pleural pressure due to active inspiratory efforts, which in turn causes high trans-pulmonary pressures.
Nowadays, it is fully demonstrated that lungs suffering from hypoxaemic respiratory failure are physiologically small (baby lungs) with a VT of 6–8 mL−1 kg−1 as the standard for mechanical ventilation in ARDS [16]. Moreover, values above this threshold have the potential of causing overdrive and ventilator-induced lung injury (VILI), even in patients with spontaneous breathing. Additionally, some authors have demonstrated that high tidal volumes above 9.5 mL kg−1 are predictors of NIV failure, especially among ARF patients with moderate to severe hypoxaemia [17, 23].
In our study, we evidenced that patients with VTE levels above this threshold had a higher percentage of ventilatory failure and death. Furthermore, we found that high inspired pressures have a high percentage of NIV failure. These peak pressures increased with constant volumes and could cause a significant reduction in compliance with an increase in lung elastance, causing alveolar damage, especially in de novo hypoxaemic ARF: pneumonia, ARDS, congestive heart failure, and interstitial lung disease. Additionally, in subjects with de novo hypoxaemic ARF due to congestive heart failure, the excessive increase in inspired pressures could increase intrathoracic pressure and reduce venous return with significant reduction of the cardiac index [24, 25]. In our research, subjects with congestive heart failure had an increased percentage of NIV failure, which could be associated with high inspiratory pressures.
Some authors have pointed out the potential increase in cases of myocardial infarction due to high inspiratory pressures. The presence of coronary ischaemic injury could be associated with coronary vasoconstriction due to a rapid correction of PaCO2 and the inspiratory effort of the patient [26, 27].
The results obtained in our group of patients with acute hypoxaemic respiratory failure are similar to those reported by other studies in which NIV is used with other ventilatory modes [28, 29]. Nevertheless, we must take into account that the use of AVAPS could require greater ventilatory surveillance with constant monitoring and expertise, since it can increase the inspiratory pressures in situations of low compliance. In this context, elevated inspired pressures and exhaled tidal volumes could be a guide to avoid lung damage. In contrast, the utility of AVAPS differs significantly in patients with hypercapnic respiratory failure due to obstructive pulmonary diseases, in which the significant improvement in minute volume and alveolar ventilation seems to have favourable results [13, 30].
Another important aspect of our study is the significant differences found while comparing the success and failure of treatment in patients with de novo hypoxaemic ARF. We found that pH, HCO3, pO2, PaO2/FiO2, FiO2 (%), tachycardia, and Vt mL−1 kg−1 (PBW) were predictors of success or failure. We were able to identify the critical value of inspired pressure levels. Furthermore, our study included observations made not only an hour after the therapy but even those up to 12 hours after, thus making our results beneficial in predicting possible decision-making alternatives and responses to an early and undisturbed intubation.
Our study has limitations: (1) it is a monocentric study; (2) we do not have data on haemodynamic parameters in patients with congestive heart failure; (3) other types of interfaces should be evaluated or an approach in which NIV is used with a helmet as an interface with high levels of positive end expiratory pressure in ARF; (4) it is not a randomised controlled trial; (5) subjects with hypoxaemic ARF did not use an oxygen blender; we used instead an O2 adapter and indirect measurements of FiO2; (6) the number of subjects with failure of NIV in hypercapnic ARF is low. Therefore, we were not able to reliably compare predictors of success or failure with BIPAP S/T AVAPS in this subgroup of subjects.
Nonetheless, this study provides important data, as it is the first to evaluate this mode in different ARF scenarios and allow the identification of groups at risk of failure with the determination of critical factors such as hypoxaemia, values of expiratory tidal volume and IPAP [31]. Regardless, a large-scale randomised controlled study is necessary to assess and compare this approach with other strategies, such as continuous high-flow nasal oxygen therapy [32].
In conclusion, the results of this study suggest that the use of BiPAP S/T – AVAPS in subjects with hypercapnic acute respiratory failure has a more favourable response than in those with de novo hypoxaemic ARF.