Current issue
Archive
Manuscripts accepted
About the Journal
Editorial office
Editorial board
Abstracting and indexing
Subscription
Contact
Ethical standards and procedures
Most read articles
Instructions for authors
Article Processing Charge (APC)
Regulations of paying article processing charge (APC)
UROLOGY / CLINICAL RESEARCH
Prediction of the risk of surgical complications in patients undergoing monopolar transurethral resection of bladder tumour – a prospective multicentre observational study
1
Department of General, Oncological, and Functional Urology, Medical University of Warsaw, Warsaw, Poland
2
Department of Urology and Oncological Urology, Wrocław Medical University, Wrocław, Poland
3
Department of Urology and Urological Oncology, Pomeranian Medical University, Szczecin, Poland
4
1st Department of Urology, Medical University in Łódź, Łódź, Poland
5
Department of Urology, University of Warmia and Mazury, Olsztyn, Poland
6
Department of Urology and Urologic Oncology, Medical University of Lublin, Lublin, Poland
7
Social Medicine Department, Wrocław Medical University, Wrocław, Poland
8
Chair of Statistics and Econometrics, Faculty of Economic Sciences, University of Warsaw, Warsaw, Poland
9
Maria Sklodowska-Curie Memorial Cancer Centre and Institute of Oncology, Krakow Branch, Krakow
Submission date: 2019-02-24
Final revision date: 2019-04-06
Acceptance date: 2019-04-21
Online publication date: 2019-10-07
Publication date: 2020-05-26
Arch Med Sci 2020;16(4):863-870
KEYWORDS
bladder cancertransurethral resection of bladder tumorpostoperative complicationsintraoperative complicationsresidencytransurethral resection of bladder tumour
TOPICS
ABSTRACT
Introduction:
The aim of the study was to identify predictors of surgical complications of transurethral resection of bladder tumour (TURBT).
Material and methods:
We prospectively recruited 983 consecutive patients undergoing TURBT within 7 months in six academic institutions. All patients were followed up from the surgery up to 30 days postoperatively with at least one telephone contact at the end of the observation. The primary study endpoint was any intra- or postoperative surgical complication. For the identification of predictors of complications, univariate and multivariate logistic regression models were used. Trial registration: ClinicalTrials.gov (NCT03029663). Registered 24 January 2017.
Results:
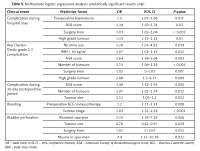
Surgical complications were noticed in 228 (23.2%) patients, including 83 (8.4%) patients with more than one complication and 33 cases of Clavien-Dindo grade 3 complications (3.3%). The most common in-hospital complications were bleeding (n = 139, 14.1%) and bladder perforation (n = 46, 4.7%). In a multivariate analysis, nicotine use, high ASA score, and the presence of high-grade tumour were the most significant predictors of high-grade complications. The stage of the disease was the strongest predictor of bleeding, while the presence of muscle in the specimen and resident surgeon were the strongest predictors for bladder perforation.
Conclusions:
TURBT poses a significant risk of surgical complications, the majority of which are of low grade.
The aim of the study was to identify predictors of surgical complications of transurethral resection of bladder tumour (TURBT).
Material and methods:
We prospectively recruited 983 consecutive patients undergoing TURBT within 7 months in six academic institutions. All patients were followed up from the surgery up to 30 days postoperatively with at least one telephone contact at the end of the observation. The primary study endpoint was any intra- or postoperative surgical complication. For the identification of predictors of complications, univariate and multivariate logistic regression models were used. Trial registration: ClinicalTrials.gov (NCT03029663). Registered 24 January 2017.
Results:
Surgical complications were noticed in 228 (23.2%) patients, including 83 (8.4%) patients with more than one complication and 33 cases of Clavien-Dindo grade 3 complications (3.3%). The most common in-hospital complications were bleeding (n = 139, 14.1%) and bladder perforation (n = 46, 4.7%). In a multivariate analysis, nicotine use, high ASA score, and the presence of high-grade tumour were the most significant predictors of high-grade complications. The stage of the disease was the strongest predictor of bleeding, while the presence of muscle in the specimen and resident surgeon were the strongest predictors for bladder perforation.
Conclusions:
TURBT poses a significant risk of surgical complications, the majority of which are of low grade.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.