Dear Editor,
A 28-year-old, 152-cm-tall female, with a known prior diagnosis of idiopathic dilated cardiomyopathy (DCMP) was admitted to our institution at 37 weeks of gestation for safe confinement and a planned elective caesarean section (CS) in view of her heart disease. There was a history of aggra-vation of her cardiac symptoms, and she had developed dyspnoea on exer-tion (NYHA III) and pedal oedema in the previous month. A focused history revealed complaints of dyspnoea on exertion with similar aggravation of symptoms 5 years prior, following the vaginal delivery of her first child, when a diagnosis of DCMP was made, and treatment was started by a cardiologist. Her symptoms had been controlled by medication since then. Her detailed past treatment records were unavailable.
Preoperative evaluation revealed pallor and mild pedal oedema with normal systemic and airway examination. Heart rate was 70 min–1, with occasional premature ventricular complexes noted on the ECG. Blood pressure was 120/70 mmHg. She was receiving once daily furosemide 20 mg p.o., metoprolol 25 mg, telmisartan 40 mg in addition to salt restriction. A COVID-19 test was done within 72 hours before the planned surgery, considering the ongoing pandemic. Laboratory investigations revealed borderline hypokalaemia (serum potassium 3.4 mEq L–1). Echocardiography revealed severe left ventricular dysfunction with global hypokinesia and an LVEF of 25%.
The patient was posted for an elective CS in view of her poor functional status. An invasive arterial blood pressure monitoring was established in addition to standard monitors. A combined spinal-epidural anaesthesia (CSEA) set (18G Tuohy/27G spinal needle) was used in the L3–4 space in the sitting position. Four milligrams (0.8 mL) of 0.5% bupivacaine (heavy) with 20 µg fentanyl (total volume 1.2 mL) was injected after confirming a free flow of cerebrospinal fluid. The epidural catheter was then inserted and secured in place without injecting any test dose. The surgeon was asked to proceed only after a sensory level of T6 was achieved (final level was T5), to prevent any patient discomfort and detrimental sympathetic stimulation. Intraoperative vitals remained within normal limits with occasional ventricular premature contractions (< 5 per min). Three units of oxytocin were given as a bolus following delivery followed by a 7.5 U h–1 infusion. Surgery lasted 35 mins, and total fluid administered was 600 mL. Intraoperatively, there was no need for any vasopressors at any point. Following surgery, we realised that the epidural catheter was not properly sited because there was resistance to any injection through it. Hence, a bilateral transmuscular quadratus lumborum block (QLB) was given under ultrasound guidance (curvilinear 2–5-MHz probe, 10-cm insulated Stimuplex needle [BBraun, Melsungen, Germany]) with 15 mL of 0.375% ropivacaine with 4 mg dexamethasone on each side. The block was given with the patient in a supine position with a wedge placed under the hip to facilitate needle insertion. The epidural catheter was removed, and the rest of her post-operative course was uneventful. Her NRS scores remined 0–2 during the first 24 hours, and only the regularly scheduled doses of paracetamol 1 g were administered intravenously every 6 hours, without the need for any rescue analgesia. The following day, she was started on oral analgesics on an on-demand basis. Informed consent was obtained from the patient for publication of her clinical details.
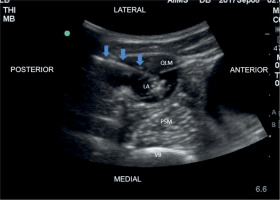
FIGURE 1
Quadratus lumborum block. QLM – quadratus lumborum muscle, PSM – psoas muscle, VB – vertebral body, LA – local anaesthetic. Blue arrows indicate block needle
DCMP in pregnancy is an uncommon entity (2–4/1000), and a challenging scenario because ventricular arrhythmias, heart failure, stroke, and death are found in 39–60% of high-risk patients [1]. The literature advises against pregnancy if the LVEF is < 30% [1]. Pregnancy is associated with significant increases in cardiac output, which is exacerbated by the sympathetic stimulation and autotransfusion in peripartum period, which therefore increases the risk of decompensation. Haemodynamic goals of anaesthetic management include the maintenance of a low-normal heart rate, normovolaemia, and the prevention of myocardial depression. While general anaesthesia has been administered successfully to such patients, we preferred CSEA because it allowed us to administer a low dose of spinal anaesthetic, preventing major haemodynamic changes. Low-dose spinal anaesthesia using 0.5% bupivacaine (6 mg) was used successfully in a case of dilated cardiomyopathy by Singh et al. [2]. QLB is an interfacial block that provides visceral pain relief unlike transversus abdominis plane (TAP) block, and the use of dexamethasone as an adjuvant resulted in prolonged effective analgesia with haemodynamic stability. The latest PROSPECT guideline for elective CS recommends the use of QLB as an alternative to intrathecal morphine [3]. Although intrathecal morphine does provide effective analgesia, it produces dose-dependent side effects like pruritis, nausea, and vomiting. In addition, the use of a QLB may result in longer-lasting analgesia and reduced postoperative opioid consumption when compared to intrathecal morphine [4]. While TAP block is also recommended, a few studies have found that the QLB provides superior and longer analgesia [5]. The ongoing COVID-19 pandemic has also accelerated the use of regional anaesthetic techniques, a trend that is likely to endure. The longer duration of analgesia also helps avert sympathetic hyperactivity related to post-operative pain. Hence, perioperative analgesia should be optimized in DCMP patients in addition to the haemodynamic goals and low-dose spinal anaesthesia combined with a regional nerve block can be an effective modality of anaesthesia in these patients.




