Dear Editor,
During invasive mechanical ventilation, the physiological mechanisms of clearing secretions from the bronchial tree are impaired. Factors affecting this process include inhibition of the cough reflex and ciliary movement in the airways and the use of sedating drugs. The standard clinical practice is the suctioning of the residual secretions in the bronchial tree performed blindly with a suction catheter. Repeated introduction of the catheter may lead to mechanical injury of the respiratory tract mucosa [1].
A forty-year-old man had been brought to the emergency room department after sustaining a traumatic head injury causing intracranial hematoma located in the posterior cranial cavity and traumatic brain oedema. He was subsequently transferred to the Intensive Care Unit (ICU) where a tracheostomy was performed due to the lack of neurological improvement, Glasgow Coma Scale (GCS) of 4 points.
During the course of hospitalization, the patient developed Acinetobacter baumannii pneumonia. On the 11th day of treatment, progressing ventilation problems were observed and the following parameters were noted: decreased tidal volumes, increase in ventilation pressure, and a sudden increase in carbon dioxide levels as seen in the arterial blood gas test.
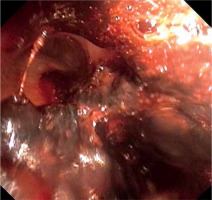
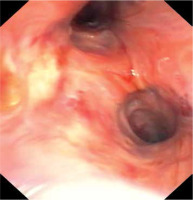
Urgent bronchofibroscopy was performed through a tracheostomy tube and a large clot around the bifurcation of the trachea impairing the patency of both main bronchi was found (Figure 1). Several attempts were made to aspirate the clot with the suction channel of the bronchofibroscope, followed by the use of endoscopic forceps, and by using external suction on the tracheostomy tube (Figure 2). Re-inspection of the airways revealed a severely hyperaemic and oozing area of the mucosa around the bifurcation of the trachea (Figure 3). Due to the extensive mucosal damage, repeated rinsing of the airways several times with norepinephrine solution (4 mg in 250 mL of cold saline) was done and resulted in the resolution of bleeding. Laboratory tests showed no abnormalities in the number of platelets and coagulogram (aPTT, PT, fibrinogen). Subsequently, the patient received a prophylactic dose of enoxaparin.
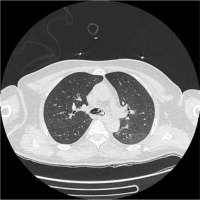
On the 13th day, the patient was noted to have decreasing levels of oxygen saturation in the blood and the recurrence of ventilation problems was observed. Bronchofibroscopy confirmed the presence of another clot in the area of the bifurcation of the trachea. Several unsuccessful attempts were made to remove the clot using suction and biopsy forceps. Computed tomography angiography of the chest revealed only the presence of a clot (Figure 4). Another round of unsuccessful attempts to remove the clot was done by using lavage, suctioning through the bronchofibroscope working channel, and biopsy forceps. Due to worsening respiratory acidosis and the need for ventilation with 100% oxygen to maintain adequate oxygenation, an attempt was made to remove the clot with the use of increased suction through the endotracheal tube. The tracheostomy tube was then replaced with an endotracheal tube, where bronchofibroscopy was used to position the tube in direct contact with the clot. After the bronchofibroscope was removed, suction was connected to the endotracheal tube and the clot was slowly pulled out along with the tracheal tube [2].
Upon repeated visual inspection, the airways were once again oozing at the mucosal surface of the trachea (Figure 3).
Due to rebleeding, nebulization with tranexamic acid was opted for (off-label use) instead of rinsing the airway mucosa with noradrenaline solution. Nebulisations with 250 mg of tranexamic acid were performed 3 times every 8 hours using a standard nebulization kit attached to the ventilator tubing system. Twenty-four hours after initiation of tranexamic acid nebulization, follow-up bronchofibroscopy was performed; it showed a largely healed mucosal surface in the area of the bifurcation of the trachea (Figure 5). No rebleeding or clot formation was observed in the following days and the mucosa of the airway was healed upon visual inspection.
Bronchofibroscopy is both a diagnostic and therapeutic method with the capability of aspiration of secretions or the use of specialised tools such as biopsy forceps. One drawback is the progressive miniaturisation of equipment that limits the suction power used during operations and removal of the formed clot in narrow airways.
Some cases may require the use of a suction pressure that is higher than that available in bronchoscopic devices. The procedure was performed using the Olympus BF-1TQ170 bronchofibroscope (Olympus European, Hamburg, Germany) with a 2.8 mm working port and a nominal suction force of 100 mmHg. Due to the presence of a large clot around the bifurcation of the trachea, a set consisting of an ID 7.5 mm endotracheal tube was used on the bronchofibroscope (Figures 6 and 7), thus making it possible to remove the clot that might potentially cause complete airway obstruction.
Tranexamic acid, a synthetic amino acid with anti-haemorrhagic pro-perties, works by blocking the conversion of plasminogen to plasmin. Its primary indication is the prevention of bleeding caused by generalised fibrinolysis and bleeding associated with fibrinolytic drugs [3–5]. It is registered in Poland and can be given through intravenous and oral routes. Some lite-rature reports that other modalities of tranexamic acid can be used, such as inhalation in the form of nebulization [6–10] and endobronchial administration [11–13]. The inhalation form allows the deposition of a substance that acts directly at the mucosal site, therefore inhibiting superficial bleeding and accelerating the reconstruction of the respiratory mucosa.
Oral or intravenous tranexamic acid is used at a dose of 20–25 mg kg–1 body weight. When nebulised in patients, a dose of 250 mg of tranexamic acid in 5 mL of saline is sufficient to act directly on the injury site [14]. The nebuliser connected to the respirator enables the production of aerosol particles having the size of 0.5–5 mm that allows movement and transport with gases to the mucosa of the respiratory system.
Due to anatomical conditions, the catheter used to clear the bronchial tree secretions damages the area of the bifurcation of the trachea and typically goes to the right bronchus. Deterioration of ventilation as manifested by an increase in ventilation pressures or limitation of tidal volumes would prompt healthcare workers to suction and evacuate secretions, which may cause repetitive damage to the airway surface, leading to bleeding and clot formation.
The gold standard in removal of the endobronchial clot is rigid bronchoscopy. This method is rarely used by anaesthetists and is predominantly used in highly specialised centres [15]. There are reports in the literature of attempts to locally dissolve the clot in the airways using the administration of tissue plasminogen activator [16], streptokinase [17] or cryoablation [15]. There are also case reports of the use of a Fogarty catheter to extract the clot from the airway [18]. Dissolving the clot only results in the removal of a mechanical blockage and still fails to address the cause of its formation.
The usage of bronchofibroscopy along with additional tools such as forceps or endoscopic baskets does not guarantee success. In the event of unsuccessful endoscopic removal, further attempts may be made by applying a larger and localised suction source. An alternative is to place the end of the endotracheal tube under direct vision to see the clot. After removal of the fiberscope, an increase in suction pressure may be used to remove the blockage along with the endotracheal tube (2) while keeping in mind the potential complication of airway barotrauma associated with the procedure.
In many centres standard practice in airway bleeding is rinsing the damaged mucosa with a cold saline solution or with solutions containing a vasoconstrictive agent. Yet there are also reports of the usage of substances that directly affect the coagulation cascade such as intravenous tranexamic acid, which may be associated with some thrombotic complications [19]. Some literature also states the beneficial use of inhaled tranexamic acid [6–10, 20, 21].
In this case of our patient, who manifested with recurrent bleeding and airway obstruction secondary to blood clots, the use of tranexamic acid for nebulisation was utilised at the lower dose compared to the dose used in infusion.
Prompt termination of superficial bleeding arising from the mucosa led to rapid healing of the damaged tissue, preventing formation of another potentially fatal airway obstruction.