Prone positioning recently gained more popularity from its use in COVID-19 management. It is gene--rally considered to improve respiratory mechanics via increased lung compliance. In surgery, prone positioning is typically encountered when it is a necessity to access certain posterior anatomic structures. Though certain post-operative complications from prone positioning are well known (e.g., postoperative vision loss), the potential intraoperative complications that it can have for respiratory com-pliance and O2 saturation, in the setting of general anaesthesia, are perhaps less familiar, as only a few studies showed improved respiratory mechanics in the setting of ge-neral anaesthesia [1–3] and one study showed that prone positioning led to a 30–35% drop in respiratory compliance under general anaesthesia [4]. As the following case illustrates, proning is a critical point in the intraoperative course as it can sometimes lead to negative respiratory sequelae disrupting homeostasis.
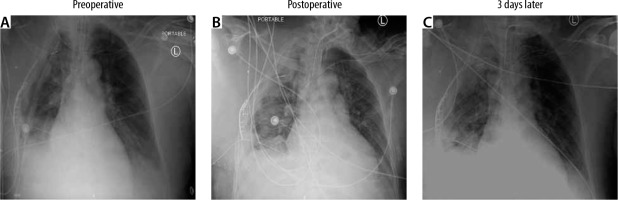
We present a case of a 48-year-old man (weight: 90.2 kg, height: 180 cm) with no significant past medical history, who sustained severe trauma as a passenger following vehicular impact at highway speed. This case report was conducted in accordance with all relevant institutional and ethical review board policies and was approved by the Rutgers New Jersey Medical School Institutional Review Board. Written informed consent was obtained from the patient for the publication of this case report. Upon presentation to the trauma bay, the patient presented with several rib fractures, a tension pneumothorax, and right-sided pulmonary contusions. The right-sided pneumothorax was temporised by a needle decompression, after which an ipsilateral haemothorax became apparent. A right-sided thoracotomy was then performed and revealed areas of posterior right lung lacerations from concurrent rib fractures. Another, more prominent laceration was observed in the right middle lobe which sustained a parenchymal injury and subsequently had an air leak. The air leak was sealed, and two chest tubes were inserted to stabilise the patient with a total drainage output of 1600 mL. Additionally, the patient sustained atlanto-occipital and atlanto-axial dislocation requiring surgical fusion of C2, which is the setting of this report. A preoperative chest X-ray further illustrates the patient’s respiratory status, showing a resolution of the initial haemothorax but presence of a pleural effusion and atelectasis (Figure 1A). In order to optimise the patient before the C2 fusion surgery, the decision was made to maintain the patient’s chest tubes on suction, which would remove any fluid from the right lung. The patient presented for the C2 fusion surgery intubated and mechanically ventilated on 40% FiO2, tidal volumes of 500 mL, positive end-expiratory pressure (PEEP) of 10 cm H2O, and a respiratory rate of 16. The patient was transported to the operating room from the ICU with PEEP ventilation. Once in the operating room arterial blood gas (ABG) analysis revealed a PaO2 of 100 mmHg on 60% FiO2 and subsequent repeat baseline ABG before commencing surgery showed worsening hypoxaemia with a PaO2 of 91 mmHg on 100% FiO2, PEEP of 10 cm H2O, tidal volume of 500 mL, and a respiratory rate of 20. Given the surgical urgency, a decision was made by the anaesthesia and orthopaedic teams to proceed despite the suboptimal respiratory status. A slow inhaled anaesthetic induction via the already inserted endotracheal tube was chosen with expired sevoflurane of about 1 MAC (~2 vol%) and paralysis with rocuronium (0.2 mg kg–1). The patient was positioned from the supine to prone position on a Jackson table (Mizuho, Tokyo, Japan). Initially the patient tolerated the prone position with SpO2 of 100%. However, roughly 10 minutes after the repositioning, the SpO2 began to fall gradually to a nadir of 78%. Manual PEEP via bag ventilation was utilised while adequate ventilation was confirmed with bronchoscopy which confirmed airway patency and removed minimal secretions. An additional ABG analysis was performed and recorded at this time. The hypoxaemia did not resolve with hand ventilation and SpO2 over 80% was not achievable. A decision to abort the procedure was made and the patient was re-positioned in the supine position. ABG results indicated a PaO2 of 53 mmHg on 100% FiO2 accompanied by hypercapnia with a PaCO2 of 79 mmHg. Interestingly, shortly after the repositioning the patient’s SpO2 quickly returned to 100%. Postoperative chest X-ray revealed worsening pleural effusion and associated atelectasis (Figure 1B). In order to facilitate mechanical ventilation and reduce dead space, a tracheostomy was performed. Over the next three days, the patient’s status gradually improved. One of the patient’s two chest tubes was removed and a subsequent chest X-ray showed improvement of the pleural effusion and atelectasis (Figure 1C). It was at this time that spinal fusion surgery was attempted again and was completed successfully with less desaturation with proning and a SpO2 nadir of 92% and with no further complications.
FIGURE 1
Chest X-rays during the preoperative assessment (A), postoperatively (B), and three days later before the repeat surgery (C) are presented. Patient exhibits worsening pleural effusion and subsequent gradual improvement
Prone positioning is shown to improve gas exchange in normal, healthy patients by affecting ventilation and perfusion in a way that optimises the V/Q ratio. The prone placement of the lung makes both ventilation and perfusion more uniform, which limits mismatch and ulti-mately results in improved gas exchange [5, 6]. This is mainly due to the anatomical geometry of lung tissue such that the dorso-caudal regions of the lung become compressed in the supine position and are subsequently relieved when positioned in the prone position [7].
Prone positioning is beneficial in patients with ARDS and hence used in ICU settings [8]. ARDS patients exhibit increased oedema leading to increased lung weight and an increased pressure along the vertical-dorsal axis due to gravity. This leads to reduced ventilation and perfusion, especially in West’s zone 3, which experiences the highest blood flow. In the prone position, the underlying increased pressure in ARDS shifts and homogenises, ultimately improving ventilation and perfusion by eliminating the negative sequela of gravity. Because of this aetiology prone positioning is useful in ARDS patients.
However, this patient experienced several thoracic injuries, including bilateral rib fractures, a tension pneumothorax, and pulmonary contusions – all of which cause significant deformity of the pulmonary structure and vasculature. The tension pneumothorax and subsequent haemothorax were treated with two chest tubes but the sustained lung tissue injury led to significant pleural effusion and atelectasis, which worsened the patient’s respiratory status. Such injuries to the lung parenchyma are expected to alter V/Q matching because of areas of dead space or shunting. In this case, the patient’s underlying pleural effusion led to significant hypoxaemia via an intrapulmonary shunt [9]. Theoretically, prone positioning should improve this patient’s hypoxaemia by improving V/Q matching, decreasing the shunt fraction, and relieving compression on any atelectatic lung zones [10]. However, the effects of prone positioning on the equilibrium between the opposing forces of the chest wall recoil and the elasticity of the lung may not have been beneficial in this situation. The patient’s bilateral rib fractures and chest injuries most likely led to thoracic collapse when in the prone position. The additional pressure on the thorax in conjunction with the underlying trauma made this patient susceptible to reduced preload, cardiac inflow or outflow obstruction, as well as significant deformation of lung morphology – all of which could have contributed to transient hypoxaemia when prone [11]. Interestingly, this does not occur in all patients who sustain thoracic trauma. A previous report in a man who sustained significant thoracic trauma leading to pulmonary contusions and ARDS showed that prone positioning improved respiratory recovery [12]. However, that patient did not undergo surgery and, more importantly, did not receive general anaesthesia, which is likely to worsen an underlying V/Q mismatch by increasing the intrapulmonary shunt [13].
It is also possible that in the prone position the patient had more weight on his right side and more compression in the area predominantly affected by the pleural effusion; such positional changes have been shown to decrease oxygen saturation [14]. By having more weight shifted ipsilaterally to the pleural effusions, the A-a gradient can increase, leading to hypoxaemia [15]. Furthermore, blood flow can also be affected due to compression of the pulmonary vessels with an increase in hydrostatic pressure, and subsequent diversion of blood flow to the other lung, which would further exacerbate the V/Q mismatch.
In summary, we present a case of a middle-aged patient with major thoracic trauma who experienced significant respiratory decompensation with prone positioning. In most situations, prone positioning has been shown to improve respiratory function and attenuate V/Q mismatch in both healthy and ARDS patients. However, in patients who exhibit severe thoracic trauma and injury to the lungs, prone positioning can be harmful by distorting the normal structure of the lungs and rib cage and thereby leading to significant V/Q mismatch and hypoxaemia. Extra vigilance and careful communication are warranted in order to ensure safe prone positioning before surgery.




