Introduction
Pheochromocytoma (PHEO) is a catecholamine-producing tumor that originates in the adrenal medulla [1]. Surgical removal of the tumor is the only curative treatment, but rapid changes in catecholamine levels during the operation would cause dramatic fluctuations in blood pressure, which poses a great challenge to surgery [2].
Due to the preoperative medical preparation and expansion of circulating blood volume, as well as improvements in anesthesia and operative techniques, the perioperative mortality of PHEO has been greatly reduced [3]. Over the past two decades, the surgical methods of PHEO have gradually changed from open surgery to laparoscopic surgery [4]. With the development of technological instruments and surgical skills, minimally invasive surgery has been progressing [5]. Even with advances in robotic surgery, robotic adrenalectomy is becoming more common [6]. Laparoscopic surgery mainly consists of two approaches: transperitoneal laparoscopic adrenalectomy (TLA) and retroperitoneal laparoscopic adrenalectomy (RLA). Because of familiarity with abdominal anatomy and a wide working space, TLA is currently the most commonly used approach [7–9]. However, the use of RLA has increased in recent years. This is because RLA can provide direct access to expose the adrenal tumor and avoid interference with intra-abdominal organs [10, 11]. Several studies have reported that RLA was superior, or at least comparable, to TLA in terms of operative time, EBL, and length of hospital stay [12–14].
However, the advantages of RLA over TLA are still controversial for PHEO. So, we performed a systematic review and meta-analysis to evaluate the efficacy and safety of RLA versus TLA for PHEO.
Material and methods
Search strategy
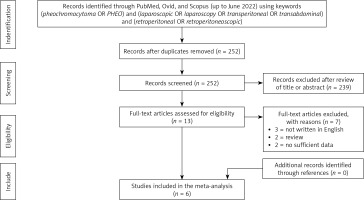
A systemic literature search of PubMed, Ovid and Scopus databases was performed prior to June 2022. The search strategy was “(pheochromocytoma OR PHEO) and (laparoscopic OR laparoscopy OR transperitoneal OR transabdominal) and (retroperitoneal OR retroperitoneoscopic)”. The following study types were included: original studies comparing RLA to TLA for PHEO. The titles and abstracts of potentially eligible studies were screened by two authors independently. All titles and abstracts written in English language were screened. Studies with insufficient data or without primary data (i.e. reviews, commentaries, conference abstracts) were excluded, but the relevant references were hand-screened to identify additional studies of interest. Any discrepancy was resolved in consultation with the third author.
Data extraction
Extraction of data was performed independently by two authors using a predefined data extraction form, including demographic characteristics (age, gender, body mass index (BMI), tumor side and tumor size), peri-operative outcomes (operative time, EBL and HI), and post-operative outcomes (complications, Clavien-Dindo score ≥ 3 complications and length of hospital stay).
Quality assessment
Two authors independently assessed the evidence level of included studies according to the Oxford Centre for Evidence-based Medicine (Table I).
Table I
Basic characteristics of included studies
Statistical analysis
Meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) criteria strictly. Cochrane Collaboration’s Review Manager (RevMan) 5.4 software (Cochrane Collaboration, Oxford, UK) was used to analyze the effects of the outcomes.
The weighted mean difference (WMD) with 95% confidence intervals (CI) was used for continuous data, while odds ratio (OR) with 95% confidence interval (CI) was calculated for dichotomous data. A validated mathematical model was used to convert median (range) to mean (standard deviation) for studies only reporting medians and ranges, because only means and standard deviations are permitted for continuous data in RevMan 5.4 [15]. Heterogeneity was defined based on the Cochrane Q p-value or I2 statistic. If p > 0.1 or I2 < 50%, a fixed-effects model was used, while if p < 0.1 or I2 > 50%, a random-effects model was used. A p-value < 0.05 was considered statistically significant. Funnel plots were examined to evaluate publication bias.
Results
Overall, six studies including 597 patients (RLA 243; TLA 354) were included in this study (Figure 1) [14, 16–20]. The basic characteristics and quality assessment of the included studies are shown in Table I.
There was no significant difference in age (WMD = –1.76 years, 95% CI: –6.34 to 2.82; p = 0.45), male component (OR = 1.09, 95% CI: 0.77 to 1.53; p = 0.63), or tumor side (OR = 1.20, 95% CI: 0.55 to 2.60; p = 0.65). RLA was associated with lower BMI compared to TLA (WMD = –0.81 kg/m2, 95% CI: –1.53 to –0.10; p = 0.03). RLA was associated with smaller tumor size (WMD = –0.90 cm, 95% CI: –1.59 to –0.20; p = 0.01) (Figure 2).
Figure 2
Forest and funnel plots of demographic characteristics of retroperitoneal laparoscopic adrenalectomy (RLA) vs. transperitoneal adrenalectomy (TLA) for pheochromocytoma (PHEO)
BMI – body mass index, SD – standard deviation, CI – confidence interval.

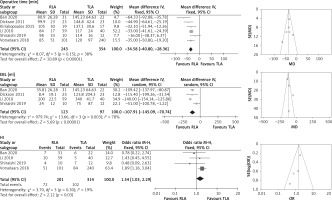
All the six studies reported operative time. The meta-analysis of these studies showed a shorter operative time for RLA (WMD = –34.58 min, 95% CI: –40.80 to –28.36; p < 0.001). EBL data were available in four studies including 220 patients (RLA 123; TLA 97) [14, 16–19]. The meta-analysis of these studies showed lower EBL for RLA (WMD = –107.91 ml, 95% CI: –145.09, –70.74; p < 0.001). Four studies including 515 patients (RLA 201; TLA 314) reported HI [14, 17–19]. The result showed that RLA was associated with a slightly higher HI rate (OR = 1.54, 95% CI: 1.03 to 2.29; p = 0.03) (Figure 3).
Figure 3
Forest and funnel plots of peri-operative outcomes of retroperitoneal laparoscopic adrenalectomy (RLA) vs. transperitoneal adrenalectomy (TLA) for pheochromocytoma (PHEO)
EBL – estimated blood loss, HI – hemodynamic instability, SD – standard deviation, CI – confidence interval.
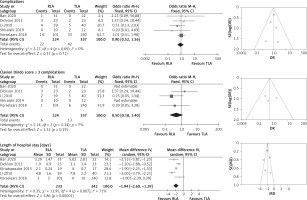
Five studies reported postoperative complications and Clavien-Dindo score ≥ 3 complications [14, 16–19]. There was no significant difference for postoperative complications (OR = 0.90, 95% CI: 0.52 to 1.56; p = 0.71) or Clavien-Dindo score ≥ 3 complications (OR = 0.50, 95% CI: 0.18 to 1.40; p = 0.19) for RLA compared to TLA. Four studies including 575 patients (RLA 233; TLA 342) reported length of hospital stay [16–19]. The results showed a shorter length of hospital stay for RLA (WMD = –1.94 days, 95% CI: –2.60 to –1.29; p < 0.001) (Figure 4).
Figure 4
Forest and funnel plots of post-operative outcomes of retroperitoneal laparoscopic adrenalectomy (RLA) vs. transperitoneal adrenalectomy (TLA) for pheochromocytoma (PHEO)
SD – standard deviation, CI – confidence interval.
There was no significant publication bias in this study.
Discussion
With the development of laparoscopic technology, laparoscopic adrenalectomy for PHEO has been proven to be a safe and viable treatment option in recent years [4]. The procedure can be performed via a transperitoneal or retroperitoneal approach [20–22]. Constantinides et al. performed a systematic review and meta-analysis of retroperitoneoscopic versus laparoscopic adrenalectomy, and they found that RLA had equivalent outcomes to TLA but might be associated with a shorter hospital stay [23]. Arezzo et al. reported a systematic review and meta-analysis of transperitoneal versus retroperitoneal laparoscopic adrenalectomy for adrenal tumors in 2018, and they found that RLA was associated with shorter time to oral food intake and reduced late morbidity [24]. Meanwhile, Vrielink et al. reported that RLA could decrease operation time, blood loss, and complication rates compared to TLA [10]. However, whether RLA is superior to TLA is still controversial for PHEO. To better understand the ongoing debate, we performed a systematic review and meta-analysis of the current literature on this topic to help guide the way for further research.
Due to the rarity of the tumor, only six studies met the inclusion criteria. In our meta-analysis, patients undergoing RLA and TLA were similar for age, gender and tumor side. The BMI was slightly lower in the RLA group, and the tumor size was smaller in the RLA group. This might be due to the inherent selection bias of a larger working space in TLA. The bias may reduce the difficulty of RLA. Jiang et al. reported a meta-analysis in which they found that RLA could achieve better perioperative outcomes than TLA [25]. However, they only included four studies and ignored the impact of BMI and tumor size.
Surgical removal of PHEO is challenging, not only due to the fluctuation in blood pressure, but also due to the abundant blood supply and adhesion to adjacent tissues [26]. In our meta-analysis, we found that RLA was superior to TLA in operative time and EBL. This could be explained by the following factors [14, 27]. First, the RLA approach could directly expose PHEO without disturbing abdominal organs. Second, the feeding arteries could be easily identified and ligated between the posterior Gerota’s fascia and the psoas muscle, which would lead to tumor shrinkage and excellent bleeding control. Third, the right adrenal vein is usually located posterolaterally to the inferior vena cava, which could be easily identified and transected through the RLA approach. Fourth, it would be easier to handle the liver adhesion through the RLA. Our results showed a slightly higher HI in RLA. Gockel et al. reported that RLA was associated with higher HI compared to TLA [28]. Vorselaars et al. reported a multivariate analysis study, and they found that RLA carried greater risk for HI compared to TLA [18]. However, Li et al. and Shiraishi et al. reported similar HI between RLA and TLA [14, 17]. There were several possible explanations for this variation. First, the definition of HI was inconsistent among different studies. Second, preoperative preparation and capacity expansion were inconsistent across studies. Third, intraoperative anesthesiology management was not standard, which would lead to different HI outcomes. Further well-designed prospective randomized studies are needed to investigate this issue.
In our meta-analysis both the postoperative complications and Clavien-Dindo score ≥ 3 complications of RLA and TLA were found to be similar. The length of hospital stay was significantly shorter in RLA. This could be explained by the advantage of RLA, which avoided interference with abdominal organs.
There are several limitations to our study. First, the main limitation of our study was the small number of included studies and the small sample size. Second, the retrospective nature of included studies limited the quality of this study. Third, the dosage and duration of preoperative medical preparation and the intraoperative anesthesiology management were not available for further analysis. Fourth, the definition of HI was inconsistent among different studies, which reduced the reliability of the results. Fifth, there were not enough data to analyze the oncological outcomes. More multicenter randomized controlled trials with standardization of preoperative medical management, intraoperative anesthesiology management, and definition of HI are needed to further evaluate this issue.
Conclusions
RLA may be a superior surgical option to TLA in selected PHEO patients, because it provides shorter operative time, less EBL, shorter length of hospital stay, and similar complications. However, RLA was associated with a higher HI rate. In addition, lower BMI and smaller tumor size of RLA reduced the difficulty of surgery. Further prospective randomized controlled trials are needed to confirm our preliminary conclusions.