Introduction
The number of bariatric operations performed worldwide increases steadily every year [1–3]. Currently, the most frequently performed types of bariatric surgery are laparoscopic sleeve gastrectomy (SG) and laparoscopic Roux-en-Y gastric bypass (RYGB) [4]. Surgical treatment of obesity has become a recognized method of treating patients diagnosed with morbid obesity and its comorbidities [5, 6]. Unfortunately, a portion of individuals who underwent a bariatric procedure does not achieve an adequate weight loss or remission of obesity-related comorbidities [7]. Revisional bariatric surgery (RBS) has been reported to be necessary in 5–25% of cases [8, 9]. Considering that the number of bariatric procedures is increasing, it can be assumed that the frequency of RBS will also increase. Therefore, investigating this group of patients appears to be currently valid.
RBS may be required due to unsatisfactory outcomes or complications after the primary procedure [10, 11]. It is often assumed that revisional surgery is more technically challenging and associated with increased morbidity and mortality [12, 13]. These procedures may potentially require longer operative time as well as prolonged length of stay (LOS) [14].
Aim
The objective of this multicenter study was to collect, systematize and present the available data on RBS after surgical treatment of morbid obesity among Polish patients. Currently, there are no data in Poland on the frequency of RBS, types of RBS, the most common indications for these procedures and their outcomes. Thus, we conducted this multicenter study.
Material and methods
Study design
This multicenter study included Polish surgical departments that perform laparoscopic bariatric procedures. It is a retrospective analysis of a prospectively maintained database conducted between 2019 and 2020 under the patronage of the Metabolic and Bariatric Surgery Chapter and the Videosurgery Chapter of the Association of Polish Surgeons. At each center, authors involved in the surgical treatment of obesity introduced data concerning bariatric patients undergoing laparoscopic RBS to build a comprehensive database. The inclusion criteria for this study were informed consent to participate in the study and meeting the eligibility criteria for RBS [15, 16]. Patients with missing or inconsistent data were excluded from the study. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement was used to design the study and to prepare the manuscript [17].
The database contained demographic characteristics of patients: sex, age, maximal weight, weight before primary surgery, weight before RBS, height, and body mass index (BMI). It also included information concerning patients’ comorbidities: type 2 diabetes (T2D) and hypertension, duration of obesity, treatment with non-steroidal anti-inflammatory drugs (NSAIDs), smoking status, alcohol consumption and others. Additionally, it included data on the primary surgery (prior intragastric balloon placement), type of surgery, LOS, complications, outcomes of primary bariatric treatment (lowest body weight, lowest BMI, T2D remission, hypertension remission), data concerning RBS (indication for RBS, center conducting RBS, LOS, type of surgery, complications), outcomes of RBS (current weight, T2D remission, hypertension remission), data concerning secondary RBS (indication for secondary RBS, center conducting RBS, LOS, type of surgery, complications) and outcomes of RBS (current weight, T2D remission, hypertension remission).
Insufficient weight loss was defined as excess weight loss (EWL) of < 50% at 18 months after bariatric surgery, while recurrence of obesity was defined as a regain of weight after initial successful weight loss (defined as EWL% > 50%) [18].
Outcomes
The primary outcomes included an analysis of the indications for RBS, the type of surgery most frequently chosen as RBS and the course of the perioperative period of treatment among patients undergoing RBS. The secondary outcome was the analysis of characteristics of the patient population undergoing RBS in Poland.
Surgical technique and perioperative care
The surgical technique and the perioperative care protocol including the preoperative, intra-operative, and postoperative interventions were standard at every participating center. Patients were treated by a multidisciplinary team consisting of surgeons, physicians, nurses, dieticians and psychologists in each bariatric center.
Ethical considerations
The data were completely anonymized, and no information about patients or hospitals was collected in the database. The study was performed in accordance with the ethical standards of the 1964 Declaration of Helsinki and its subsequent amendments (Fortaleza). The protocol was registered at clinical trials.gov (NCT05108532). There were no changes in the treatment of patients included in the study. The study was closely monitored by the primary investigator, who processed and verified any missing or unclear data submitted to the central database. The study was approved by the Bioethics Committee of the Regional Chamber of Physicians, District of Warmia and Mazury, Poland (23/2021/VIII).
Statistical analysis
We conducted a descriptive statistical analysis. All data were analyzed using Statistica software 13.1PL (StatSoft Inc., Tulsa, OK, USA). The normal distribution was checked using the Shapiro-Wilk test. A number and a percentage were used for categorical variables. For continuous variables with normal distribution, the mean and standard deviation were used. Median and range were used for non-normally distributed data. There was no shortage of data.
Results
Study group characteristics
The group consisted of 799 patients (624 (78.1%) women, 175 (21.9%) men). The mean age was 38.96 ±9.72 years. A group of 105 (13.14%) patients smoked tobacco during the bariatric treatment. Alcohol consumption above 14 units a week was recorded in 7 (0.88%) patients and 80 (10.01%) patients used NSAIDs more than once a week.
Primary bariatric surgery
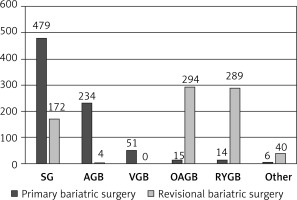
In 479 (59.95%) patients the primary procedure was SG, 234 (29.29%) patients underwent an adjustable gastric band (AGB), and 51 (6.38%) patients underwent vertical band gastroplasty (VBG). All primary surgery procedures are presented in Figure 1. Mean preoperative weight for each bariatric procedure was: 133.32 ±29.48 kg for SG, 123.99 ±23.39 kg for AGB, 130.9 ±31.08 kg for VBG, 114.67 ±31.61 kg for OAGB and 125.38 ±22.91 kg for RYGB.
Indications for RBS
In the group study, after primary surgery 374 (46.81%) patients experienced a recurrence of obesity, meeting the criteria for bariatric treatment, 288 (36.05%) patients experienced insufficient weight loss after primary surgery, 182 (22.78%) patients experienced long-term complications. A total of 42 (5.26%) patients required secondary RBS. After RBS 13 (1.63%) patients experienced recurrence of obesity that met the criteria for bariatric treatment, 10 (1.25%) patients had insufficient weight loss after RBS and 23 (2.88%) patients developed long-term complications.
Types of RBS
The types of RBS included 294 one anastomosis gastric bypass (OAGB) (36.8%), 289 RYGB (36.17%), 172 SG (21.52%) and other procedures, presented in Figure 1. Types of RBS performed after individual bariatric surgery are presented in Table I. Secondary RBS types were RYGB – 14 (33.33%%), repair of previously created anastomosis – 9 (21.43%), SG – 7 (16.67%) and other types.
Table I
Revisional procedures after each primary bariatric surgery
[i] SG – sleeve gastrectomy, AGB – adjustable gastric band, VBG – vertical band gastroplasty, OAGB – one anastomosis gastric bypass, RYGB – Roux-en-Y gastric bypass, SADI-S – single anastomosis duodeno–ileal bypass with sleeve gastrectomy, SASI – single anastomosis stomach–ileal bypass, SAGI – single anastomosis gastro-ileal bypass, BPD-DS – biliopancreatic diversion with duodenal switch.
Weight loss
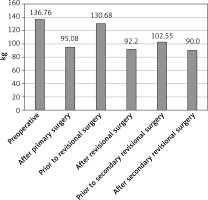
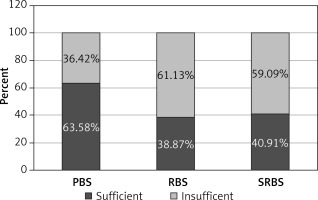
Mean preoperative weight was 136.76 ±29.27 kg. Mean preoperative BMI was 48.04 ±9.26 kg/m2. Mean lowest weight and BMI after primary surgery were 95.08 ±25.47 kg and 34.4 ±10.51 kg/m2, respectively. Before RBS mean weight and BMI were 130.68 ±26.43 kg and 39.95 ±8.38 kg/m2. After RBS mean weight and BMI were 92.2 ±22.46 kg and 32.27 ±8.05 kg/m2. Prior to secondary RBS mean weight and BMI were 102.55 ±21.795 kg and 36.71 ±7.14 kg/m2. Mean weight and BMI after secondary RBS were 90 ±29.88 kg and 33.54 ±7.84 kg/m2 (Figure 2). The mean follow-up was 22.7 ±28.3 months. After primary surgery 63.58% of patients achieved sufficient weight loss. After RBS 38.87% of patients achieved sufficient weight loss and after SRBS 40.91% of patients achieved sufficient weight loss (Figure 3).
Remission of obesity related comorbidities
T2D was diagnosed in 186 patients (23.28%) prior to bariatric treatment. A total of 335 (41.93%) patients were diagnosed with preoperative hypertension. After primary bariatric surgery 41 (22.04%) patients achieved remission of T2D. In the group of 62 (33.33%) patients we observed improvement in T2D control. A group of 62 (18.51%) patients achieved complete remission of hypertension and 88 (26.27%) patients had improvement in hypertension control. Prior to RBS T2D was diagnosed in 145 (18.15%) patients and hypertension was diagnosed among 273 (34.17%) patients. After RBS 63 (43.45%) patients achieved remission of T2D, in 54 (37.24%) patients we observed improvement of T2D control, 87 (31.87%) patients had complete remission of hypertension and 94 (34.43%) patients presented improvement in hypertension control. Prior to secondary RBS T2D was diagnosed in 18 (42.86%) patients and hypertension was diagnosed among 28 (66.67%) patients. After secondary RBS 1 (5.56%) patient achieved remission of T2D, 6 (33.33%) patients observed improvement in T2D control, 5 (17.86%) patients had complete remission of hypertension and 7 (25%) patients presented improvement in hypertension control.
Complications and LOS after RBS
Complications were noted in 222 (27.78%) cases after RBS. The most common complications included GERD – 117 (14.64%) patients, followed by vomiting in 42 (5.26%) cases, band malfunction in 20 (2.5%) patients, gastrointestinal obstruction in 20 (2.5%) patients, malnutrition in 9 (1.12%) patients, gastrointestinal leakage in 5 (0.63%) patients and anemia in 4 (0.5%) patients. A total of 8 (19.04%) patients experienced complications after second RBS. The most common included malnutrition – 2 (4.76%) patients and gastrointestinal leakage 2 (4.76%) patients. The median LOS was 3 days (2–25) after the first revisional surgery and 3.5 days (1–36) after the second RBS.
Discussion
This study includes data on, thus far, the largest group of patients undergoing RBS in Poland. The size of the study group highlights the fact that bariatric surgery is becoming increasingly common. Thus, RBS is also more frequent. Therefore, research on this group of patients seems to be up to date. In our opinion it is one of the largest databases concerning RBS ever created. Hopefully it will provide new insight and become useful to surgeons.
The most common primary bariatric surgery requiring revision in our study group was SG, followed by AGB. A meta-analysis by Koh et al. reported similar outcomes with VBG (29.0%), AGB (27.2%) and SG (27.1%), being the most common bariatric operations which required RBS [19]. Notably, the frequency of AGB drastically decreased in recent years, which may be related to its unsatisfactory long-term results [20]. The two main RBS procedures for patients after AGB are SG or RYGB and duodenal switch for extra weight loss. OAGB was used as a third alternative in our study. The need for RBS after AGB and SG has multiple causes. A meta-analysis of the effect of long-term loss of excess body weight showed that AGB compared to RYGB, OAGB and SG has significantly worse long-term results. EWL was 45.9% for AGB, 57% for SG, 55.4% for RYGB and 80.9% for OAGB [21]. The analysis of the short-term weight loss in patients after AGB treated with SG (n = 205) and RYGB (n = 232) showed no significant differences between the groups [22] Another study describing revisions after unsuccessful AGB using laparoscopic RYGB and SG showed that LOS and complication rates after 12 months are similar for both methods, but better weight loss after 24 months was noted for RYGB [23]. The analysis of studies comparing RBS after AGB and SG (n = 106) and RYGB (n = 514) revealed RYGB to be a method where EWL was twice as high as after SG [24]. OAGB is also a therapeutic option ensuring safety and a good effect after insufficient AGB surgery [25]. OAGB is recognized as a revision after primary restrictive surgery – the Kermansaravi meta-analysis included a total of 1771 revised patients, indicating high efficacy in both weight loss after secondary surgery and satisfactory remission of T2D with follow-up up to 5 years [26]. It should be remembered that OAGB may be a factor conducive to GERD remission and the development of GERD de novo symptoms.
According to our data, the most common indications for RBS were insufficient weight loss and recurrence of obesity. This is in line with a previous meta-analysis by Koh et al., who reported insufficient weight loss, followed by complications of primary surgery, to be the most common indications [19]. Amiki et al. conducted a study on patients undergoing RBS due to insufficient weight loss or GERD [27]. According to O’Brien et al. the most common causes of gastric band failure are band slippage, ingrowth, port dislocation and patient intolerance by the patient [21].
The relative lack of long-term data for more than 10 years on sleeve gastrectomy is worrying as it has already become the most common bariatric procedure. Data are often difficult to interpret due to different definitions of RBS. The systematic review of Cheung et al. highlights the research difficulties in determining the actual benefits of using a specific procedure after SG. At the same time, it identifies RYGB as one of the potential methods useful for achieving short-term weight reduction [28]. The meta-analysis by Matar et al. explored the problem of insufficient weight loss or recurrence of obesity as well as SG complications such as GERD. RYGB is presented here as a revision method in patients with GERD or due to insufficient weight loss/obesity recurrence. It achieves satisfactory relief of GERD symptoms and weight loss [29]. Unfortunately, these data refer to a short-term analysis – up to one year.
An extensive meta-analysis by Guan et al. revealed differences in the short- and long-term SG scores [30]. The overall revision rate was 10.4%, but for patients ≥ 10 years of follow-up it was 22.6%. The most common cause of revision was, as in our study, failure to lose weight, but the most common RBS was RYGB. The higher incidence of GERD after SG is well known. While in the case of primary GERD there is a high effectiveness of SG with simultaneous anti-reflux treatment, in the case of revision surgery, the effectiveness of up to 100% is ensured by RYGB [31]. There is an increasing number of patients diagnosed after SG with Barrett’s esophagus in the absence of correlation between GERD and symptoms [32]. This may become an argument for the use of RYGB instead of OAGB, but so far there are insufficient long-term data available. It seems that the introduction of routine endoscopic diagnostics after SG could be considered as an additional criterion in selecting the type of RBS [33]. The counterargument is that the weight loss effect of revision RYGB surgery is worse than that of the primary RYGB. The results of secondary RYGB for diabetes remission are similar to the primary surgery [13]. Alternative revision procedures after RYGB are biliopancreatic diversion with duodenal switch, distal RYGB gastric banding or laparoscopic pouch resizing, banding over pouch and/or revision of gastro-jejunal anastomosis. However, the best results in terms of weight loss are achieved by biliopancreatic diversion with duodenal switch and distal RYGB, especially in a 5-year follow-up [34, 35]. In our study, we found 6 patients who underwent pouch resizing and 4 who underwent anastomotic revisions.
OAGB was the most common RBS in our study group. This procedure was feasible and effective after unsuccessful restrictive bariatric surgery. Conversion to OAGB may induce significant excess weight loss after SG, VBG, and especially AGB [25, 26]. Compared to RYGB it seems to be simpler and provides a better weight reduction, but more nutritional deficits [36]. Comparing OAGB and RYGB as RBS, Velotti et al. noted a comparable or lower complication rate and better weight loss after revisional OAGB. Similarly, Yeo et al. in another meta-analysis emphasized greater weight loss in the first 2 years after revisional OAGB and its potential for achieving diabetes and hypertension remission [37, 38]. The metabolic effect after RBS in our study concerned 63 (7.88%) patients who achieved remission of T2D, and 87 (10.89%) patients who had complete remission of arterial hypertension. Taking into account the criterion of diabetes remission in patients after primary bariatric surgery, it seems to favor RYGB over SG, but the review of the data focuses mainly on short-term analysis [39]. In RBS especially for RYGB after AGB, VBG and SG, the results of diabetes remission are better than conversion from AGB to SG [40].
According to the meta-analysis by Koh et al. RYGB is currently the most frequently performed RBS [19]. Amiki et al. observed that biliopancreatic diversion with duodenal switch as a revision surgery seems effective in further weight loss in the medium term, and RYGB appears to be effective in GERD treatment [27].
Secondary RBS is usually performed due to postoperative complications following the primary surgery or RBS. Therefore, in our study secondary RBS was more likely intended to treat postoperative complications than to achieve significant weight loss or improvement in obesity related comorbidities. A study by Kuzminow et al. reported the reoperation rate due to complications after secondary bariatric procedures and the need for further bariatric surgery. The authors estimated that 8.8% of bariatric patients required tertiary surgery, which is more than we are reporting in the present study (5.26%). Nevertheless, according to Kuzminow et al., the risk of tertiary bariatric surgery is higher than usually reported [41]. It may happen, for instance, that the third operation is conducted in a different surgical center. We cannot rule out such a possibility.
This study is associated with several limitations. The database included patients treated only in Polish bariatric centers. Therefore, the generalization of the presented outcomes to other countries should be done with caution. Due to the lack of precise guidelines concerning RBS, the protocol of care for this group of patients may be non-uniform. This could result in discrepancies in indications, operative technique, preoperative and postoperative patient care after RBS.
Data from large multicenter studies on RBS are urgently needed to guide recommendations, lacking in this domain. Choosing the proper operation for patients with insufficient weight loss, weight regain, or complications could optimize outcomes and safety of bariatric treatment.
Conclusions
RBS most often concerns patients after SG. The main indication for RBS is weight regain. OAGB and RYGB were the two most frequently chosen types of RBS. Secondary operations lead to further weight reduction and improvement in the management of T2D and other obesity related comorbidities. However, RBS is associated with a significant risk of complications.