Introduction
Stroke is characterized by a high incidence rate, high disability rate, and high mortality rate [1]. Acute ischaemic stroke (AIS) accounts for approximately 80% of all strokes [2]. Due to the narrow time window for intravenous thrombolysis, the use of endovascular treatment is increasing. At present, the most commonly used methods of endovascular treatment are stent retriever thrombectomy and aspiration thrombectomy. Stent retriever thrombectomy has been confirmed as the standard treatment for AIS by 5 large randomized controlled trials [3–7] published in 2015. Moreover, the 2018 guidelines for the early management of patients with AIS clearly state that stent retriever thrombectomy is still the first choice for AIS endovascular treatment [8]. However, in recent years, some studies have shown that the safety and efficacy of aspiration thrombectomy are not inferior to those of stent retriever thrombectomy [9, 10], although the results remain controversial.
Aim
This meta-analysis aims to systematically evaluate the safety and efficacy of aspiration thrombectomy versus stent retriever thrombectomy in the treatment of AIS and provide evidence-based references for clinical diagnosis and treatment.
Material and methods
Search strategy
We clearly declared the subject of our systematic review in accordance with the populations, interventions, comparators, outcomes, and study (PICOS) design principle. The subjects, AIS patients, were divided into 2 groups: a group who received aspiration thrombectomy and a control group who received stent retriever thrombectomy instead. Outcomes included 90-day all-cause mortality, 90-day modified Rankin Scale (mRS) scores of 0–2, and intracranial haemorrhage and successful recanalization rates. We searched the PubMed, Embase, Cochrane Library, and SinoMed databases to collect randomized controlled trials (RCTs) and retrospective studies of aspiration thrombectomy versus stent retriever thrombectomy in the treatment of AIS. The Chinese database was searched with the terms “aspiration thrombectomy”, “stent retriever thrombectomy”, “acute ischemic stroke”, “randomized controlled trial”, and “retrospective studies”. The English-language databases were searched with the terms “ischemic stroke”, “thrombectomy”, “stents”, “randomized controlled trial”, and “retrospective studies”, and some references from the identified articles were searched simultaneously. The time range for retrieval was from database inception to 15 March 2021.
Inclusion criteria
(1) The studies were randomized controlled trials or retrospective studies on aspiration thrombectomy versus stent retriever thrombectomy as treatment for AIS; both foreign and domestic publications were included. (2) The experimental group underwent aspiration thrombectomy (there were no limitations on the type of aspiration catheter or the aspiration mode), the control group underwent stent retriever thrombectomy (any stent type was permitted), and any embolic vessel location was permitted. (3) Complete information was available regarding diagnosis, treatment, prognosis, follow-up, and clinical data. (4) Outcome indicators: Safety outcomes were measured by 90-day all-cause mortality and intracranial haemorrhage. Efficacy outcomes were measured by a 90-day mRS scores 0–2 and the successful recanalization rate (TICI score 2b-3/mTICI score 2b-3/eTICI score 2b-3).
Exclusion criteria
(1) Descriptive literature such as reviews, comments, or case reports; conference proceedings; correspondence; preclinical studies, etc. (2) Studies lacking critical key information, such as loss of therapeutic details and basic characteristics of patients. (3) Repeated analyses of previously included studies.
Data extraction
The extracted data included the first author, year of publication, type of study, embolic vessel locations, intervention measures, sample size of patients, mean age, sex ratio, and outcome indicators. Hong and Luo read the literature and extracted the data at the same time. In the event of a disagreement between those two authors, all the authors discussed the matter and arrived at a final decision together.
Quality assessment
We applied the Jadad scale to evaluate the quality of RCTs included in this study, using a 0–5 score to indicate the quality of each RCT. Studies scoring 2 points or less were considered low-quality research, and studies scoring ≥ 3 points were considered high-quality research. The quality of the retrospective studies was evaluated with the MINORS evaluation items. This instrument has 12 evaluation items. Each item is scored on a scale of 0–2 points, where 0 points means the item was not reported, 1 point means the item was reported with insufficient information, and 2 points means the item was reported with sufficient information.
Statistical analysis
Combined effect: odds ratios (ORs) and 95% confidence intervals (CIs) were used to compare dichotomous variables. Continuous variables are expressed as the mean ± standard deviation (x ± s), mean deviation (MD), and 95% CI. The confidence intervals were used to compare the 2 groups. P-values < 0.05 were considered statistically significant.
Heterogeneity analysis: Heterogeneity was generally measured and estimated by the I2. When I2 < 30%, heterogeneity was considered low. If I2 > 50%, heterogeneity was deemed significant. Sensitivity analysis was implemented by eliminating individual studies one by one to identify the source of heterogeneity.
Forest plots were used to determine whether the difference between aspiration thrombectomy and stent retriever thrombectomy for AIS treatment was statistically significant. Funnel plots were used to assess publication bias in the included studies. The analysis was performed with a random effects model because all the included studies have heterogenous datasets from different centres.
RevMan 5.2 was used for this study.
Results
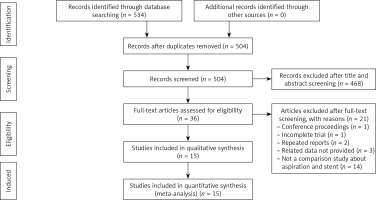
The screening process for this study is presented in Figure 1. A total of 534 related citations were obtained; 30 duplicate citations were excluded, leaving 504. After the titles and abstracts were read, 468 articles were excluded, leaving 36. After the full-text articles were read, 21 studies that did not meet the inclusion criteria were excluded, and the remaining 15 studies were included [9–23], comprising 2 RCTs and 13 retrospective studies. The basic information and quality evaluations of the included studies are shown in Table I. Among a total of 3067 cases, 1063 were in the aspiration thrombectomy group, and 2004 were in the stent retriever thrombectomy group.
Table I
Baseline characteristics of the included studies
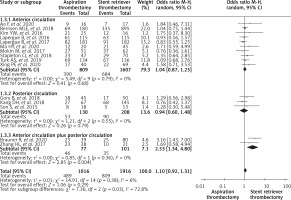
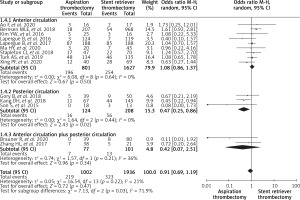
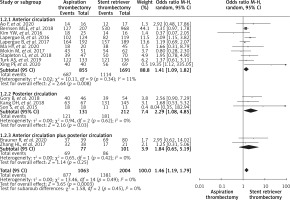
There was no significant difference in 90-day all-cause mortality between the aspiration thrombectomy group and the stent retriever thrombectomy group (OR = 0.98, 95% CI: (0.81, 1.20), p = 0.88), as shown in Figure 2. The proportion of patients with 90-day mRS scores of 0–2 was also not significantly different between the 2 groups, as shown in Figure 3 (OR = 1.10, 95% CI: (0.92, 1.31), p = 0.29). Regarding intracranial haemorrhage, the 2 groups once again had no significant difference, as shown in Figure 4 (OR = 0.91, 95% CI (0.69, 1.19), p = 0.47). In terms of successful recanalization rate, the aspiration thrombectomy group had better outcomes than the stent retriever thrombectomy group, and the difference was statistically significant (OR = 1.46, 95% CI (1.19, 1.79), p = 0.0003), as shown in Figure 5. As can be seen from the forest plots, the heterogeneity of 90-day all-cause mortality (I2 = 0%), 90-day mRS scores of 0–2 (I2 = 6%), intracranial haemorrhage (I2 = 21%), and successful recanalization rate (I2 = 0%) are less than 30%, so it was considered low heterogeneity.
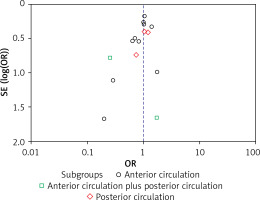
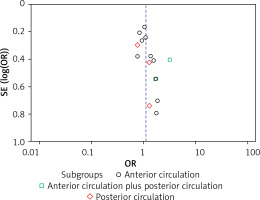
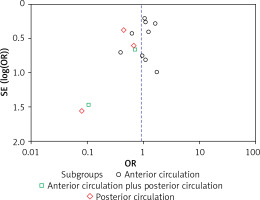
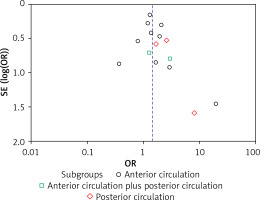
In order to explore the reasons for the different successful recanalization rates, the AIS patients were divided into 3 subgroups, namely, the anterior circulation subgroup, the posterior circulation subgroup, and the anterior circulation plus posterior circulation subgroup, according to the anterior circulation and posterior circulation. The results showed that there was no significant difference in 90-day all-cause mortality by procedure type within the anterior circulation (OR = 1.00, 95% CI (0.80, 1.24), p = 0.97), posterior circulation (OR = 1.06, 95% CI (0.63, 1.79), p = 0.83), or anterior circulation plus posterior circulation (OR = 0.38, 95% CI (0.08, 1.74), p = 0.21) subgroup. There was also no significant difference by procedure type in the proportion of 90-day mRS scores 0–2 within the anterior circulation (OR = 1.04, 95% CI (0.87, 1.25), p = 0.68) and posterior circulation (OR = 0.94, 95% CI (0.60, 1.48), p = 0.79) except for anterior circulation plus posterior circulation (OR = 2.53, 95% CI (1.34, 4.80), p = 0.004) subgroup. Regarding intracranial haemorrhage, the aspiration and stent retriever thrombectomy groups showed no significant difference in the anterior circulation (OR = 1.08, 95% CI (0.86, 1.37), p = 0.50) and anterior circulation plus posterior circulation (OR = 0.42, 95% CI (0.07, 2.51), p = 0.34) subgroup except the posterior circulation (OR = 0.47, 95% CI (0.25, 0.86), p = 0.02) subgroup. Regarding the successful recanalization rate, the anterior circulation (OR = 1.41, 95% CI (1.09, 1.82), p = 0.008) and posterior circulation (OR = 2.29, 95% CI (1.08, 4.85), p = 0.03) subgroups showed higher values in the aspiration thrombectomy group than in the stent retriever thrombectomy group. However, there was no significant difference between procedure types in the anterior circulation plus posterior circulation subgroup (OR = 1.84, 95% CI (0.65, 5.19), p = 0.25). The subgroup analysis showed that there was no significant difference in anterior circulation and posterior circulation in 90-day all-cause mortality (anterior circulation, p = 0.97, posterior circulation, p = 0.83) and 90-day mRS scores 0–2 (anterior circulation, p = 0.68, posterior circulation, p = 0.79) between aspiration thrombectomy and stent retriever thrombectomy. Aspiration thrombectomy was better in successful recanalization rate in anterior circulation and posterior circulation (anterior circulation, p = 0.008, posterior circulation, p = 0.03), with lower incidence of intracranial haemorrhage than stent retriever thrombectomy in posterior circulation (p = 0.02). The results of subgroup analysis showed that aspiration thrombectomy was not inferior to stent retriever thrombectomy in anterior circulation or posterior circulation.
The 90-day all-cause mortality, 90-day mRS scores 0–2, intracranial haemorrhage rate, and successful recanalization rate are shown in funnel plots, and the details are shown in Figures 6–9. The distribution of points was basically symmetrical, which indicated that there was no obvious publication bias.
Sensitivity analysis was performed on the outcome indicators of 90-day all-cause mortality, 90-day mRS scores 0–2, intracranial haemorrhage rate, and successful recanalization rate, respectively. The sensitivity analysis results showed that excluding any one of the studies did not affect the total results of our meta-analysis for all outcome indicators.
Discussion
Our meta-analysis included 15 studies, containing 2 RCTs (the ASTER [9] and COMPASS [10] trials), and a total of 3067 AIS patients were eligible for analysis. The results of our study show that there was no significant difference in 90-day all-cause mortality, 90-day mRS scores 0–2, or intracranial haemorrhage between aspiration thrombectomy and stent retriever thrombectomy. Although some similar meta-analyses have been reported before our study, they are different in some aspects [24–30]. Primiani et al. [24] reported that aspiration thrombectomy was a safe and effective alternative to primary stent retriever thrombectomy for AIS in a total sample size of 9127 patients, but their included studies did not include all control groups. Qin et al. [25] stated that aspiration thrombectomy had better functional outcomes than stent retriever thrombectomy and a similar successful recanalization rate, but less than 9 studies (included studies = 9) were included in the final analysis. Zhang et al. [26] included 20 studies (17 studies were retrospective, and 3 studies were prospective) and showed similar clinical outcomes of aspiration thrombectomy and stent retriever. However, significant heterogeneity was detected in outcome indicators, which reduced the reliability of these pooled results. Tsang et al. [27], in an analysis of 18 studies, found that stent retriever thrombectomy was superior to aspiration thrombectomy in successful recanalization. The high heterogeneity among studies may explain why that meta-analysis produced different results from the others. Ye et al. found [28] that aspiration thrombectomy had a higher success rate and shorter recanalization times than stent retriever thrombectomy based on 5 basilar artery occlusion studies. However, Sheng et al. [29] only included posterior circulation stroke and found there was no statistically significant difference for the primary clinical outcomes of mortality and favourable outcome (mRS score 0–2) at 3 months. Because anterior circulation occlusion is more common, the outcomes of Ye and Sheng cannot be representative of the overall reality. Boulanger et al. [30], in an analysis of 15 anterior circulation large-artery occlusion studies, stated that there was no difference in efficacy and safety between first-line contact aspiration and stent retriever thrombectomy, as in our meta-analysis. Recently, a BASICS RCT [31] on endovascular therapy versus medical treatment for basilar-artery occlusion showed no significantly different in functional outcome, despite many prospective studies suggesting otherwise. The BASICS RCT study was a randomized controlled trial. Hence, we should prudently choose endovascular therapy for basilar-artery occlusion stroke.
In subgroup analysis, 90-day mRS scores 0–2 (anterior circulation plus posterior circulation), intracranial haemorrhage (posterior circulation), and successful recanalization rate (anterior circulation plus posterior circulation) were opposite to pooled analysis. The small number of patients included in these subgroups may be the cause of this discrepancy. Moreover, we found that higher recanalization was not necessarily associated with better functional outcomes. Hussein et al. [32] also presented that recanalization sometimes failed to produce good outcomes in the endovascular treatment of the basilar artery. Ischaemia-reperfusion injury [33], the number of thrombectomy attempts [34], and the procedure time [35] might limit its benefit. Loh et al. [34] found that more than 3 thrombectomy attempts may not improve the chance of recanalization and may increase the risk of symptomatic intracranial haemorrhage after surgery. Two randomized controlled trials (the ASTER [9] and COMPASS [10] trials) clearly stated that operators should switch to another endovascular treatment when the large vessels continued to be occluded after 3 failed thrombectomy attempts. Therefore, it is reasonable to believe that switching to another device is a better option after 3 failed thrombectomy attempts. Mehdi et al. [35] found that a shorter procedure time was one of the important predictors of good functional outcomes. Although we did not conduct the procedure time analysis of aspiration thrombectomy and stent retriever thrombectomy, this could be considered an advantage of aspiration thrombectomy.
In recent years, in order to achieve better clinical outcomes, and reduce the times of thrombectomy attempts and complications, researchers have proposed 2 new treatment schemes, namely “switching strategy” and “Solumbra” [36]. “Switching strategy” refers to the situation when vascular recanalization is not achieved or there are several thrombectomy attempts by one device, and then a second device should be used as a remedy. “Solumbra” is a combination of aspiration thrombectomy and stent retriever thrombectomy. The most common combination is a Solitaire FR stent and penumbral reperfusion catheter. The technical principle is that, with the assistance of the intermediate catheter, after conventional stent release, the syringe is connected to the end of the guide catheter for continuous negative pressure inhalation, while the stent system is retracted. Texakalidis et al. [37] reported 3 endovascular treatments (Stent Retrievers, Direct Aspiration, and Combined Approach), and showed that stent retrieval thrombectomy and direct aspiration did not have significant differences. The combined approach achieved higher mTICI 2b/3 and mTICI 3 recanalization rates compared to aspiration alone, although with a higher risk of SAH. Furthermore, “Solumbra” costs more than “switching strategy” [36], and Turk et al. [10] proved that aspiration thrombectomy costs less than stent retriever thrombectomy. Therefore, aspiration thrombectomy or switching strategy with aspiration thrombectomy as the first-line treatment is a better choice for AIS because it greatly reduces the patients burden while obtaining favourable clinical outcomes, which are a significant advantage.
This paper has some limitations: (1) There were only 2 randomized controlled trials, and the rest were retrospective studies, which may have had bias in the selection or exclusion of cases on a subjective basis. Nonetheless, the larger sample size can reduce the bias. (2) There was a large gap between the sizes of the aspiration and stent retriever thrombectomy groups. (3) In the subgroup analysis, the posterior circulation subgroup and the anterior circulation plus posterior circulation subgroup included few studies; more clinical trials are needed to improve the quality of evidence. (4) Two studies of M2 occlusions were included in our study, and there may be a bias between our results and the real world because some interventionists consider M2 strokes as distal occlusions, and the results were different from large vessel occlusions. Therefore, our meta-analysis results should be analysed prudently; subgroup analysis can be performed if there are enough studies. (5) Because there were few studies of balloon guide catheter in our meta-analysis, we did not take into account it.
Conclusions
Our meta-analysis showed that the outcomes of aspiration thrombectomy were similar to those of stent thrombectomy in terms of 90-day all-cause mortality, 90-day mRS score 0–2, and intracranial haemorrhage, but superior to stent thrombectomy in terms of successful recurrence rates. Both aspiration thrombectomy and stent thrombectomy can be used as the first line of intravascular treatment for AIS.