Introduction
Atrial fibrillation (AF) is one of the most common arrhythmias. The prevalence in patients ≥ 65 years old is 4.8% in women and 6.2% in men [1]. The most important risk factors are as follows: age > 60 years, arterial hypertension, and heart diseases (coronary artery disease, cardiomyopathy, pericardial inflammation, prior heart attacks, congestive heart failure, etc.). According to the RecordAF study, 15.6% of patients with recently diagnosed AF in Poland have AF without any underlying heart disease [2]. In this considerable group of patients, we tried to look for other possible causes. There is an increasing amount of literature on the influence of hiatal hernia (HH) with occurrence of AF. HH is defined as the protrusion of intra-abdominal structures through a dilated oesophageal hiatus. In the USA 60% of patients over 50 years old have HH [3]. Cases of AF in which a surgical repair of HH treated the arrhythmia seem to confirm a cause and effect relation of this two diseases [4]. Most studies concentrate on how many patients with HH also have AF. Roy et al. reported that 5.3% of patients with HH had also AF.
The aim of this paper is to investigate how many patients with AF waiting for an ablation have HH. We think such results are interesting for clinicians, because this lesion, as an increasing number of studies suggest, may be another risk factor for AF. Moreover, the mentioned case reports show that it may be a treatable cause. Radiologists should be aware of the role that HH may play in the pathomechanism of AF, so it should be reported in every patient with AF.
The multi-detector row computed tomography (MDCT) can visualise anatomical structures with high resolution. In cardiology, MDCT can be used to determine the coronary calcium score, the coronary arteries (coronary CT angiography – CCTA). Furthermore, CCTA is used to visualise coronary atherosclerosis, coronary stents, bypass grafts, coronary and pulmonary veins, and general morphology of the heart and vessels [5]. The clinical applications of cardiac CT involve AF wherein it is used for visualisation of the anatomy of pulmonary veins necessary for atrial ablation – treatment of AF.
Material and methods
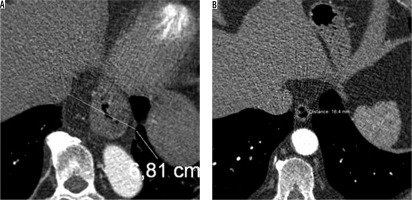
The study included 207 patients with planned ablation of pulmonary veins and 234 in the control group, which consisted of patients who had CT examination (CCTA) to exclude coronary disease. No scans were performed only for the purpose of this study, all the patients were sent for CT due to medical reasons, and the study was retrospective. The control group consisted of 71 women and 163 men (mean age 59.01 ± 10.57 years, range 24-83 years), and the study group included 78 women and 129 men (mean age 58.07 ± 11.55 years, range 21-87 years). The inclusion criterion was diagnosed AF; whereas, there was no AF in the control group. The study included 442 CT chest examinations on a dual-source CT scanner (SOMATOM Definition Flash, Siemens Heathineers, Forchheim, Germany) in the Silesian Centre for Heart Disease in Zabrze, Poland. Hiatal hernias were observed and measured in each CT examination (Figure 1). The radiologists detected all hiatal hernias in CT scans without dividing into slide or paraesophageal HH. In the AF group no patients had symptoms of gastro-oesophageal reflux disease (GERD).
Figure 1
Computed tomography images of one of the biggest (A) and one of the smallest (B) hiatal hernias in our study population
The statistical analysis was carried out with the Statistica 10 package (StatSoft, United States), with the threshold of statistical significance set at p ≤ 0.05. The c2 test and some variations of this (c2 with Yates corrected and Fisher exact) were performed.
Results
We analysed the data of 207 patients in the study group and 234 in the control group. Baseline characteristics are summarised in Table 1. In the study group 10 patients (4.83%) had an HH of 2 cm or less and 19 (9.18%) had HH greater than 2 cm; whereas, in the control group these were 2 (0.85%) and 26 (11.11%), respectively. The statistical analysis shows that the prevalence of small HH (≤ 2 cm) is almost 6 times higher in the study group compared to the control group, which is not observed for large HH. This parameter is statistically significant in the analysis with the Yates c2 test (p = 0.026), but it has weak association, with a contingency coefficient of 0.13. No more correlations were found in statistical analysis.
Table 1
The analysis of our data in relation to age, sex, and diameter of HH
Discussion
The largest study up till now that focused on this issue showed that 7.1% of patients with HH also had AF, compared to 1% of the general population [6]. There was no breakdown of patients with HH into type or size groups [6]. Our research demonstrated that HH with a size smaller than 2 cm is correlated with a higher risk of atrial fibrillation. We could not prove correlation between large HH and AF. The explanation may be that our control group consisted of patients enrolled for CCTA because of clinical symptoms such as heartburn. This could have resulted in a larger number of HH in our control group than in the general population. The most common theory of how HH can trigger AF is mechanical irritation of the left atrium. There are cases of AF treatment due to HH repair, but the sizes of these lesions are substantially larger, for example two-thirds of the stomach above the diaphragm in a case reported by Cristian et al. [4]. Naoum et al. showed in a study with 52 patients with large HHs, defined as a hernia consisting of ≥ 30% intrathoracic stomach, that they can cause haemodynamic changes and dyspnoea [7]. While radiologists are describing CT scans of the heart, they should measure diameters of HH, to rule out one possible and treatable mechanism causing AF. Our study may suggest that there are different possible ways to correlate atrial fibrillation and hiatus hernias. Perhaps, mechanical irritation is only one of many causes.


