Introduction
Over the past three decades, Poland has made substantial progress in reducing tobacco use [1–3]. Between 1982 and 2019 the prevalence of daily tobacco smoking decreased from 62% to 24.4% among men and from 32% to 18% among women [1]. According to the Chief Sanitary Inspectorate, in 2019, 21.0% of Poles aged 15 and over were current daily smokers and 1.3% were occasional tobacco smokers [1]. Despite the substantial decrease in tobacco use in Poland, still, more than 70,000 people die each year from smoking-related diseases [2, 3] and lung cancer remains the leading cause of cancer death among both men and women [4].
In 1995, the Polish Parliament introduced a comprehensive tobacco control law to reduce the burden of tobacco-related illness and protect non-smokers and children from secondhand smoke. Smoke-free policy in Poland imposed restrictions on the sale, advertising, and promotion of tobacco products (including prohibiting the sale of tobacco products in healthcare facilities), mandated health warnings on tobacco product packages, and restricted smoking in certain types of public spaces, including healthcare facilities, schools and indoor workplaces [5]. However, the Act still allowed for designated smoking spaces and also specifically provided for a physician to give a patient under his or her care an exemption from the restriction on smoking in healthcare settings [5]. The Act was amended multiple times over subsequent years [6–8]. A substantial revision in November 2010 extended and clarified the requirements for smokefree spaces [7]. The amendment stated that the prohibition on smoking in healthcare facilities extended to all premises where healthcare services are provided, excluded healthcare facilities from the list of establishments where designated smoking rooms were allowed, and removed the provision allowing a doctor to give a patient an exemption from the smoking prohibition. Thus, the 2010 revision mandated a complete ban on smoking in all healthcare facilities [7]. A further July 2016 amendment to the Act extends the smoking ban to electronic cigarettes and novel tobacco products [6, 8]. At the same time, the 2016 amendment allows that the owner or manager of healthcare facility may designate a smoking room “in 24-hour psychiatric wards, excluding wards with enhanced and maximum security conditions” [8].
Smoking behavior and norms among health professionals and in the healthcare setting have played an important role historically in leading population level changes in tobacco use [9, 10]. For example, in the U.S., early findings about the health effects of smoking in the 1950s led to a rapid drop in smoking prevalence among physicians and increase in physician advice to patients to quit smoking, which, in turn, was followed by a shift in Americans’ attitudes towards smoking [9]. Additionally, a systematic review of available evidence supports the conclusion that institutional smoke-free policies in hospitals and universities do reduce smoking rates [11]. Thus, healthcare entities, especially hospitals, have an important role in setting an example through implementation of smoke-free policies [12, 13]. Key elements of a comprehensive hospital smoke-free policy include: (1) providing a smoke-free environment for patients, visitors and staff, (2) reducing tobacco consumption among the staff and (3) providing tobacco cessation services for patients [12–15]. Since 2000, the Global Network for Tobacco Free Healthcare Services (ENSH-Global) (primarily as the European Network of Smoke-free Hospitals) has developed guidelines and supportive instruments to promote a smoke-free environment in hospitals across the globe [16]. Data from Spain [17] and Ireland [18] indicate that the tools developed by ENSH-Global can be an effective method of evaluating tobacco control policies in hospitals. Currently, there is a lack of data on the smoke-free policies implemented in hospitals operating in Poland. The aims of this study were: (1) to determine the state of smoke-free practices in hospitals operating in Poland, as well as (2) to identify challenges facing hospitals implementing smoke-free practices.
Material and methods
A cross-sectional survey was conducted between September and November 2018 in a representative sample of 100 hospitals operating in Poland. The study group was randomly selected from 210 hospitals that are members of the Polish Hospital Federation, which is the most representative hospital organization in Poland. The Federation is a nationwide organization of hospitals regardless of their ownership structure, size or operating model, and represents 75,000 hospital beds and over 140,000 hospital employees across Poland [19]. Additionally, ten hospitals were selected for qualitative interviews with a member of the hospital management staff in order to enhance interpretation of the survey results and to gather more detailed information about challenges in implementing smoke-free policies.
The survey instrument was adapted from the ENSH-Global Self-Audit Questionnaire (version 10/01/2016), developed by the Global Network for Tobacco Free Healthcare Services. The questionnaire has been previously piloted in smoke-free hospital surveys in France, Finland, Ireland and Italy [20]. ENSH-Global Self-Audit Questionnaire enables hospitals to monitor and review their progress towards achievement of a smoke-free environment [21]. The questionnaire was adapted and translated into Polish using standard procedures including back-translation.
The questionnaire included 48 items covering various aspects of smoke-free policy implementation in hospitals (Supplementary material – Appendix 1). The questions were sorted into 8 standards: governance and commitment (10 items), communication (3 items), education and training (4 items), identification, diagnosis and tobacco cessation support (10 items), tobacco-free environment (7 items), healthy workplace (5 items), community engagement (4 items) and monitoring and evaluation (5 items). Each of 48 items was scored with a 4-point response scale: 0 = no/not implemented, 1 = less than half implemented, 2 = more than half implemented and 3 = yes/fully implemented. The maximum score of the questionnaire was 144 points, as the sum of its 8 standards. The questionnaire was addressed to the managing director or a designated board member and completed through a phone interview conducted by a member of the study team. The response rate was 100%.
Statistical analysis
The data were analyzed with Statistica 12 Software (StatSoft, USA). Normality of distribution of continuous variables was assessed by the Shapiro-Wilk test. The distribution of categorical variables was shown by proportions. The degree of implementation of the smoke-free practices in the hospitals was analyzed by means of the score obtained in each standard of the ENSH-Global Self-Audit Questionnaire. Based on the ownership structure, the hospitals were classified into private or public healthcare entities. Differences in the distribution of quantitative variables were evaluated based on the results of the Student’s t-test or non-parametric test (Mann-Whitney U test). Statistical inference was based on the criterion p < 0.05.
Results
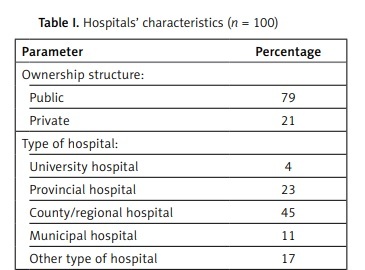
Among the surveyed hospitals, 65% were public non-profit entities, 14% were incorporated with a majority public sector share, and 21% were private corporations (Table I). Categorized by type: 4% were university hospitals, 23% provincial/regional hospitals, 45% county hospitals, 11% municipal hospitals, and 17% other facilities. The staff size in the surveyed hospitals ranged from 25 to 5,000 employees. The respondent group was composed of general directors (18%), mid-level managers (5%), specialists (quality, occupational health and safety or epidemiology) (51%), quality representatives (12%), and other employees responsible for implementation of legal regulations (14%). The mean score for all analyzed standards was 78.55 points (out of 144 maximum available), with no statistically significant (p = 0.4) difference between public and private entities (Table II).
Table I
Hospitals’ characteristics (n = 100)
Table II
Scoring for individual ENSH Standards depending on the ownership structure of the hospital
More than half of the surveyed hospitals (61%) have fully implemented a tobacco-free policy in line with the ENSH-Global Standards. Among the 8 analyzed standards, the best implemented standards were standard 1 (governance and commitment), standard 2 (communication) and standard 5 (tobacco-free environment). In the majority of surveyed hospitals (87%), a senior manager is responsible for the implementation of the tobacco-free policy, and more than half of the hospitals (60%) set up a dedicated implementation team responsible for the development and implementation of the hospital’s tobacco-free policy. In almost all of the surveyed entities, hospital staff (95%), service users (98%) and the community, including specific target groups (95%), were informed, at least at a basic level, about the hospital’s tobacco-free policy and the available tobacco cessation services.
Signage identifying prohibited products and the tobacco-free campus boundaries were present in all of the surveyed hospitals. The vast majority of hospitals make informational materials available on the health effects of smoking (87%), provide brief advice on how to quit smoking (70%), and provide access to tobacco cessation services (81%) and pharmacological support (64%). In 85% of surveyed hospitals medical staff were trained in providing brief advice to motivate tobacco users to quit, and in 77% of hospitals the key medical staff were trained in motivational tobacco cessation techniques. Almost all hospitals reported a total ban on the sale of tobacco products and associated devices (including e-cigarettes) (96%) and a ban on the acceptance of tobacco industry sponsorship and funding (92%). A total ban on tobacco use (including buildings, grounds and transport systems) was achieved in 97 out of 100 surveyed hospitals.
The lowest degree of implementation of smoke-free hospital practices was observed for standard 4 (identification, diagnosis and tobacco cessation support), standard 7 (community engagement) and standard 8 (monitoring and evaluation). More than half of hospitals (64%) did not routinely identify tobacco use or refer tobacco users for treatment, and 54% of surveyed hospitals did not document active or passive smoking status in the patient’s medical records. About half (53%) of hospitals have disciplinary procedures in place for non-compliance with the tobacco-free policies by staff. Only 25% of hospitals had a system in place to record policy breaches and other incidents, and 22% of hospitals had a procedure to monitor secondhand smoke exposure in the facility. Only 21% of the surveyed hospitals actively promoted and disseminated their tobacco-free activities. Detailed results for each of the analyzed standards are presented as Supplementary Tables SI–SVIII.
In the qualitative interviews, hospital staff provided additional information about the challenges in implementing smoke-free policies in Polish hospitals. Hospital staff interviewed noted that, despite having a written institutional policy, hospitals lacked any specific documentation about how the policy should be implemented or who is responsible for enforcing it. Additionally, they identified specific barriers, including a lack of sanctions or consequences for violating the policy, disregard of the policy by some staff and visitors, and the lack of support for treating nicotine dependence.
Discussion
To the authors’ best knowledge, this is the first available study addressing smoke-free practices in hospitals operating in Poland. Overall, we observed a high level of commitment by hospitals for maintaining a tobacco-free environment. In most of the surveyed entities, staff, service users and visitors were generally informed about the institution’s tobacco control policy. Nevertheless, the majority of hospitals surveyed do not conduct periodic monitoring and evaluation of the smoke-free policy. The identification and treatment of patients who use tobacco products remain a significant challenge for many hospitals.
According to the National Tobacco Control Act in Poland [8], smoking in the buildings and on premises of healthcare facilities is completely prohibited (except in designated places in 24-hour psychiatric wards) and the owner or manager of the hospital should place in a visible location appropriate text and graphic signs informing staff and visitors about the smoking ban. In our study, all surveyed hospitals reported the presence of signage identifying prohibited products and the tobacco-free campus boundaries. Similar results were observed in a report of the Chief Sanitary Inspectorate, which is responsible for the enforcement and audit of the implementation of the smoke-free policy in Poland. In 2016, among 49,040 audited healthcare entities in Poland (most of which were not hospitals), only three failed to meet smoke-free hospital requirements resulting from the National Tobacco Control Act [22]. The lack of significant differences in the implementation of smoke-free policy between public and private entities may be due to the fact that the National Tobacco Control Act applies to all medical facilities, regardless of the ownership structure.
Our findings show some similarities with findings in other European countries using the same ENSH-Global Self-Audit Questionnaire. Martinez et al. [17] performed two cross-sectional surveys in 32 hospitals of Catalonia, Spain, to evaluate tobacco control policies before (2005) and after (2007) the implementation of a national smoke-free workplace policy. After implementation of the policy, a significant increase (36.5%) in the implementation score of tobacco control polices was observed in hospitals. The highest score was seen for “environment” and “tobacco control” standards, while the “health promotion” and “identification and cessation support” standards saw only limited implementation [17]. Additionally, another study from Spain surveying hospital middle managers found that although they were aware of and supported hospital smokefree policies, they had a limited role in enforcing the policy and did not make use of enforcement mechanisms such as fines [23]. These findings are similar to what was observed in our study, which showed broad awareness of hospital smoking restrictions and success in their implementation but a lack of support for tobacco cessation and health promotion activities and lack of formal compliance mechanisms. In a study by McArdle and Kabir [18] performed in healthcare facilities in Ireland, the surveyed entities had a systematic procedure in place to identify and document the tobacco use status of patients, though the study sample was small (only 3 healthcare facilities). In our study, systematic procedures to document the tobacco use status of patients are still lacking in Poland. Nevertheless, we observed high compliance with education and training standards among the clinical staff of the surveyed hospitals. Similarly, in a study from Ireland, 81% of nursing staff and 92% of medical staff received training in smoking cessation techniques [18]. In a study from Catalonia, Spain, cessation programs were mostly observed in central referral hospitals and high technology hospitals [17].
There is no safe level of exposure to secondhand smoke [24]. According to the World Health Organization policy recommendations, all indoor public places and workplaces should be 100% smoke-free [6, 24]. Exposure to secondhand smoke harms children and adults. Hospitalized patients, due to their health status, should be particularly protected from secondhand smoke. National smoke-free policies should address healthcare facilities as a priority in providing a smoke-free environment. In the U.S., hospitals were undergoing the first industry-wide ban on smoking in the workplace and set an example for other industries on how to eliminate exposure to secondhand smoke [25]. Moreover, several studies showed that hospital-initiated smoking cessation intervention effectively improves quit outcomes and may lead to a subsequent decrease in healthcare usage [26–28].
In 2017, over 7.1 million deaths and loss of 182 million disability-adjusted life-years (DALYs) were attributable to tobacco use [29]. Smoking is the most preventable cause of cardiovascular disease – the leading cause of death worldwide [29–31]. Therefore, smoking cessation should be a priority for cardiovascular high-risk patients [30, 31]. During hospitalization for illness, smokers are more likely to be receptive to health messages to quit and motivated to change their behavior [28]. Thus, providing a smoke-free environment and access to smoking cessation services in the healthcare facility can be a crucial factor in contributing to smoking cessation among patients [32]. However, smoking cessation services are often unavailable during hospitalization. Although various forms of pharmacotherapies for smoking cessation (including nicotine replacement therapy, cytisine, varenicline, and bupropion) are available over the counter, they are not covered by health insurance in Poland. Moreover, a study conducted in 2018 among 423 physicians in Poland showed that only two-thirds of physicians assessed the smoking status of their patients and 37.6% of physicians regularly offered minimal intervention on smoking cessation to smoking patients [10]. Providing smoking cessation counseling and medication for hospitalized smokers may increase smoking cessation rates [26–28]. Moreover, identification of the patients’ smoking status should be a standard procedure when admitted to the hospital. Organizational activities are needed to improve access to smoking cessation services for hospitalized smokers, especially those with cardiovascular or respiratory diseases [33, 34].
Tobacco smoking in the hospital setting is not only an issue for smokers, but also creates administrative challenges for healthcare facility managers. Smoking in hospital buildings, especially in social rooms or bathrooms, causes damage to hospital infrastructure, increases cleaning costs and presents a fire hazard, especially among patients who smoke in hospital beds [35]. An effective smoke-free policy should also address occupational health and safety issues.
Our study has some limitations which should be acknowledged. First, the results on the presence of smoke in hospitals and compliance with the policy were based on staff reporting and were not verified by measurements of environmental tobacco smoke, such as through the use of passive nicotine monitors or measurements of concentration of particulate matter (PM2.5). Secondly, compliance with smoke-free policy was defined based on self-reported data provided by managing directors or designated board members, so we cannot exclude the possibility of recall bias. Additionally, we did not measure the prevalence of tobacco use among patients and the hospital staff. Nevertheless, this is the first and largest study assessing the state of smoke-free practices in hospitals operating in Poland. The results of our study have significant public health implications and point to the areas of hospital tobacco control policies that warrant increased attention.
In conclusion, smoke-free policies in hospitals operating in Poland are compliant with the National Tobacco Control Act and provide a smoke-free environment for service users and staff. However, ongoing monitoring, evaluation and proactive implementation of tobacco control are necessary to support effective and ongoing implementation of these policies and to increase access to cessation services. To achieve a smoke-free country, tobacco-free hospitals should become leaders in national tobacco control strategies and policies.