Introduction
Tens of millions of patients in China suffer from chronic hepatitis, out of which nearly one-third of the hepatitis patients gradually develop liver cirrhosis and portal hypertension (PH) [1]. The most significant complication that leads to death due to cirrhosis is esophageal and gastric varices bleeding (EGVB). A constant increase in the number of elderly patients has been reported, with the increasing life expectancy of the population. The elderly often suffer from a variety of medical comorbidities that have an adverse effect on the surgical outcomes, which is one of the reasons why palliative care modalities are preferred, including endoscopic treatment. With the development of technology, endoscopy has emerged as a significant technique for non-surgical treatment of EGVB. Endoscopy provides a positive and temporary hemostatic effect through the ligation of the varicose vessel and injection with a sclerosing agent. Despite the provision of short-term hemostasis, the rebleeding rate can be as high as 60% [2].
For a long time, open splenectomy plus pericardial devascularization (OSPD) has been widely accepted by surgeons as an effective treatment option for hypersplenism caused by EGVB and PH [3]. In 1991, Delaitre and Maignien proposed the first laparoscopic splenectomy (LS) [4]. A growing body evidence indicates that with the improvement in types of operating devices, laparoscopy is a preferred choice over open surgery for splenectomy [5–8]. Unfortunately, only limited studies dealing with LS plus pericardial devascularization (LSPD) for elderly patients are available.
Aim
This study was aimed at evaluating the safety and effectiveness of spleen bed LSPD in elderly patients with PH.
Material and methods
Patients
A total of 132 elderly patients (age > 60 years), who had undergone LSPD or OSPD for EGVB of PH between June 2014 and December 2019, were selected, while patients who underwent laparotomy or had a history of abdominal surgery were not included. Patients and their families were informed of the advantages, disadvantages, and the risks associated with the two approaches, and they were asked to make a voluntary choice between laparoscopic surgery and conventional open surgery. Thus, informed consent was obtained from all participants. All surgical procedures were performed by the surgical team of the department. The approval of the Ethics Committee of the hospital was sought before the study. The clinical data of the selected patients are presented in Table I.
Table I
Clinical characteristics of laparoscopic and open surgery groups
Operative method
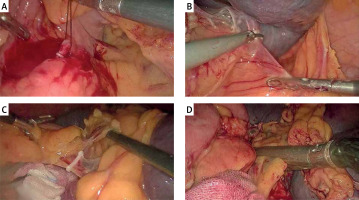
The patient was placed in a right lateral semidecubitus position with tilting of the operating table slightly to the reverse Trendelenburg position. The surgeon operated from the right side of the operating table. Depending on the size of the spleen, a pneumoperitoneum was created by puncturing under or near the umbilicus, and the intra-abdominal pressure was maintained at 12–14 mm Hg. The abdominal cavity was examined by puncturing a 10-mm trocar (trocar A) and by placing a 30° scope. Two trocars (trocar B and C; length = 5 mm) were inserted under the xiphisternum and the left mid-abdomen; a 12-mm trocar (trocar D) was inserted at the mid-point between the xiphisternum and the navel; and a 10-mm trocar (trocar E) was inserted at the midpoint between the left mid-abdomen and the navel. The positions of the trocars were often corrected according to the length of the spleen. The operator and the camera were positioned on the right side of the patient, while the assistant was on the left side. The splenogastric ligament was divided with a harmonic scalpel against the greater curvature of the stomach, such that the splenic artery could be separated and ligated (Photo 1 A) if it was noted to be located at the superior margin of the pancreas. If it was located behind the pancreas and was difficult to detect, the spleen was prepared for dissection without ligating or separating the splenic artery. The inferior margin of the spleen was held up by the grasping forceps, and the connective tissue, including the splenorenal ligaments, was divided using a harmonic scalpel (Photo 1 B). Then, the upper pole of the spleen was held up with the grasping forceps, and the connective tissues of the splenic–diaphragmatic ligament was divided. The short gastric vessels were well ligated with Hem-o-lok clamps and the spleen was freed from all attachments and ligaments (Photo 1 C), except for the splenic hilum. Finally, the splenectomy was completed using an endoscopic linear stapler (Echelon Flex 60 Endopath) to transect the spleen at the splenic hilum through the tunnel between the superior edge of the splenic hilum and the superior pole of the splenogastric ligament (Photo 1 D). The spleen was then placed in a large specimen bag and was cut into pieces and extracted using trocar E. After dissection of the left subphrenic vein, the posterior gastric vein and the branches of the distal gastric coronary vein, including the gastric and esophageal branches and superior esophageal branches, the perforating branches of the paraesophageal vein, the distal esophagus was made completely free for 8 to 10 cm by using a harmonic scalpel and hem-o-lock clamps. Thus, devascularization was accomplished. OSPD was performed as previously described [6].
Statistical analysis
Continuous variables were expressed as mean ± standard deviation and were compared using Student’s t-test. Quantitative variables were compared using χ2 analysis and Fisher’s exact test. P < 0.05 was considered to be statistically significant. Statistical analyses were conducted using the SPSS 21.0 software.
Results
A comparative analysis of the clinical characteristics of the two groups is presented in Table I. No differences in clinical characteristics were found between the two groups (p > 0.05 for all). No deaths were reported during surgery in either of the groups. The difference between the operation time of LSPD and OSPD groups (151.6 ±19.9, 157.9 ±16.7 min, respectively; p = 0.052) was not statistically significant. The estimated blood loss in the LSPD group was significantly less than that in the OSPD group (268.5 ±159.4, 341.6 ±160.9 ml, respectively; p < 0.05). No other major intra-operative complications were reported in the two groups.
The patients of the LSPD group took less time to start oral intake as compared to those in the OSPD group (1.9 ±0.9, 3.1 ±0.9 days, respectively; p < 0.05). The mean duration of post-operative hospital stay of the LSPD group was shorter than that of the OSPD group (7.6 ±1.7, 9.5 ±1.8 days, respectively; p < 0.05). The most common complication observed in both the groups was portal vein thrombosis (PVT), although the incidence rate was lower in the LSPD group than the OSPD group (11.8%, 31.3%, respectively; p < 0.05). Other complications included pancreatic leakage, pleural effusion, pulmonary infection, and delayed wound healing; the complication rate was lower in the LSPD group (p < 0.05). No deaths from postoperative complications were reported. The perioperative data are shown in Tables II and III.
Table II
Perioperative clinical data of patients in laparoscopic and open surgery groups
Table III
Postoperative complications during hospitalization and follow-up data of patients in laparoscopic and open surgery groups
During the post-operative follow-up period (6–70 months) (Table III), esophagogastric variceal rebleeding occurred in 5 (7.4%) patients who underwent laparoscopic surgery and 6 (9.4%) patients who underwent open surgery (p = 0.673). Hepatic encephalopathy occurred in 3 (4.4%) patients who underwent laparoscopic surgery and 2 (3.1%) patients who underwent open surgery (p = 0.699). Secondary liver cancer was reported in 3 (4.4%) patients who underwent laparoscopic surgery and in 4 (6.3%) patients who underwent open surgery (p = 0.638). Three patients from the laparoscopy group died because of acute upper gastrointestinal rebleeding, 3 died because of hepatic encephalopathy, and 2 died because of secondary liver cancer. The 3 patients who underwent open surgery died because of acute upper gastrointestinal rebleeding, 3 died because of hepatic encephalopathy, and 4 because of secondary liver cancer. The mortality rate of the two groups did not differ significantly (p = 0.518).
Discussion
In 1966, Hassab proposed splenectomy plus pericardial devascularization for PH [6]. OSPD has been widely applied for treating EGVB and hypersplenism caused by PH in China [9]. In recent years, due to the latest advances in techniques and instruments, laparoscopic techniques, including LSPD, have been widely used for surgical purposes in clinics [8]. The spleen of patients with liver cirrhosis is often enlarged, which permits little space, leading to difficulty in performing surgery and in separating the splenic hilum. When the splenic hilum is separated in situ, the gap between the splenic hilum and the pancreatic tail is often extremely small, and there is a possibility that the ligation of the splenic hilum may damage the pancreatic tail during surgery and thereby increase the risk of pancreatic leakage. In general, elderly patients with PH have more complications than younger patients, and they tend to receive less curative treatment, which leads to a poorer prognosis than younger patients. Under these circumstances, the conventional surgical procedure for LS was modified [10], which was proved to be safer.
The conventional method for the improved surgical approach not only made splenectomy a precise procedure but ligating the splenic hilum usually requires deep dissection of the surrounding ligaments to fully expose it, which increases the risk of injury and bleeding due to extensive separation. During dissection along the splenic bed to the upper spleen, this area was found to contain loose connective tissue lacking blood vessels, from which the spleen could be separated relatively safely. After sufficient separation of the perisplenic ligaments, a tunnel was created through the spleen bed of the splenic hilum and posterolateral to the spleen. The splenic hilum was disconnected through the tunnel using an endoscopic linear stapler to avoid damage to the blood vessels; thus, the risk of bleeding and injury of the pancreatic tail was decreased, which was reported in our previous research [11].
This study found LSPD to be more advantageous than OSPD for the following reasons: less intraoperative blood loss; oral intake can be started early; and shorter duration of postoperative hospital stay. These advantages have also been reported in previous studies [12, 13]. The amount of intraoperative blood loss can be lessened by controlling the splenic hilum through the tunnel; hence, to a large extent, it reduces the risk of hemorrhage due to a large number of branches of the splenic portal vessels or due to incomplete dissection. Oral intake could be started early and resulted in a shorter duration of postoperative hospital stay, as the invasion was minimal. However, the time taken for surgery was longer than that mentioned in other reports [14]. The reason could be that much time was spent removing the residual spleen from the abdominal cavity. The time taken to perform laparoscopy decreases gradually with experience. The data revealed that the incidence of complications was lower in the LSPD group, especially pertaining to PVT, pancreatic leakage, pleural effusion, pulmonary infection, and wound infection. PVT was reported as a potentially fatal postoperative complication after splenectomy, which is mainly associated with injury to vascular endothelial cells and alterations in portal vein hemodynamics and blood coagulation [15]. The results also showed that the rate of PVT was significantly lower in the LSPD group than in the OSPD group, which may be due to the following reasons: first, early ambulation increased the blood flow of the portal vein system, which was helpful in reducing the hypercoagulable state of this system; second, aspirin and low molecular weight heparin were started on the first day after surgery if the patient had minimal risk associated with bleeding [16]. The rate of pancreatic leakage was significantly lower in the LSPD group than in the OSPD group. Pancreatic leakage occurred, as the tail of the pancreas was injured due to inadequacy in the dissection of the splenic hilum, as well as postoperative thrombosis of the splenic veins, which possibly led to congestion, hemorrhage, and necrosis of the tail of the pancreas. If the conventional surgical approach is changed to avoid damage to the important anatomical structures at the splenic hilum, injury to the pancreas during dissection of the splenic hilum can be avoided.
Elderly patients also have some coexisting medical morbidities, such as diabetes mellitus, hypertension, and CVDs, which can have adverse effects on surgical outcomes. As elderly patients are not in a position to bear much trauma during the surgical process and need to recover quickly, improved surgical methods are required. This study revealed several advantages of the modified approach over open surgery, including earlier postoperative recovery and fewer postoperative complications. However, the present study also had some limitations. This was a retrospective study, and all the patients underwent treatment at a single center. Therefore, the need for validation and judging the feasibility of the surgical approach by employing a more heterogeneous sample through the selection of patients from different centers is recommended. Thus, spleen bed LSPD is a safe and feasible procedure that can be adopted by experienced surgeons to treat elderly PH patients.