Introduction
Colorectal cancer (CRC) is one of the most frequently diagnosed neoplasms in Western countries [1] and is estimated to be the main cause of cancer-related death [2]. The average risk of developing CRC in the general population is about 6% [3]. Regrettably, the first diagnosis of CRC typically occurs when it is already in its most advanced stage (i.e., in > 30% of cases), and often with metastases (in ~18% of rectal cancer cases and in ~20–25% of colon cancer cases) [2, 4, 5].
The CRCs are a heterogeneous group of cancers with respect to their molecular backgrounds. The pathogenesis of CRC involves many different processes that violate the integrity of the cell genome (from chromosomal and microsatellite instability to abnormal methylation and DNA repair) [6–9]. Unfortunately, the diagnosis of CRC remains difficult as its symptoms depend on the localization and can be easily overlooked by patients (e.g., occult bleeding) [2]. Colonoscopy is still the gold standard of CRC diagnosis; it allows for both diagnostics (tumor localization, histopathology) and treatment of the tumor in its early stages (such as polyp removal) [10–12].
Some previous studies have shown strong correlations between particular gene mutations (such as MUTYH mutations) and CRC, with reports that about 30% of CRC cases are inherited [2]. In this study, we focused on one member of the transporter family of proteins, P-glycoprotein (~170 kDa), which is encoded by the MDR1/ABCB1 gene (multidrug resistance 1/ATP-binding cassette sub-family B member 1) [13–16]. P-glycoprotein is an active (ATP-dependent) transporter of xenobiotics (mainly large hydrophobic proteins) [16–20]. Enterocytes spanning the whole digestive tract contain P-glycoprotein, but its largest aggregation is situated at the end of the digestive tract, specifically in the colorectal region [19, 20].
The participation of P-glycoprotein in carcinogenesis and its role in drug resistance to chemotherapy are well documented [21–28]. Animal models have confirmed the participation of P-glycoprotein in the carcinogenesis of not only CRCs, but also breast and liver cancers [29–31]. In addition, a link between the MDR1/ABCB1 gene and the Wnt/β-catenin signaling cascade has been found, the latter being the most encountered dysfunction in rare cases of inherited CRC [2]. Moreover, it has been observed in vitro that MDR1/ABCB1 gene expression occurs in cells with P53 mutations (P53 mutations are detected in 50% of CRC cases) [32–35].
MDR1/ABCB1 gene analysis reveals the existence of 28 exons containing 48 polymorphic variants or single-nucleotide polymorphisms (SNPs) that might contribute to interindividual variability in the function of P-glycoprotein [36]. One of the three most common polymorphisms occurs in the 26th exon (RefSNP ID: rs1045642), while others are present in the 21st exon (RefSNP ID: rs2032582) and in the 12th exon (RefSNP ID: rs1128503) [37]. Previous studies have reported links between the ABCB1 C3435T (rs1045642) polymorphism with an increased risk of developing kidney epithelial tumor and acute lymphoblastic leukemia [38, 39]. The rs1045642 polymorphism (a synonymous sequence variant in which there is no resulting change to the encoded amino acid) affects both the expression of the MDR1 gene and the activity of P-glycoprotein.
The relationship between the genetic variants (CC, CT, or TT) of the rs1045642 polymorphism and CRC diagnosis is not clear [40–42]. However, the CC genotype may determine proper immunity in the digestive tract, as evidenced by an increased frequency of this genotype in regions with less developed medical care and increased exposure to threatening digestive tract infections (i.e., ~83% in Ghana vs. ~25% in Poland) [42, 43].
Therefore, the aim of this study was to assess the impact of the MDR1/ABCB1 polymorphism (rs1045642) on the risk of CRC and to assess any general anthropometric factors involved in its development.
Material and methods
The study included 250 patients hospitalized in the Department of Gastroenterology and Metabolic Diseases, Medical University of Warsaw (which was divided into the Department of Internal Diseases and Diabetology and the Department of Gastroenterology and Internal Medicine in 2015) and the Department of Hematology, Oncology and Internal Diseases, Medical University of Warsaw. The selection criteria for inclusion in the study were patients who underwent both a colonoscopy and polypectomy in a single endoscopy unit between 2006 and 2013 for reasons other than oncologic surveillance after CRC. All patients included in the study underwent a detailed survey to deduce the general risk factors, concomitant diseases, family history, and anthropometric measurements. A histological examination of polyp specimens was performed and genetic information was obtained from a blood sample. Histological examinations were performed in the Medical University of Warsaw; CRC was diagnosed by histological examination using the established WHO clinical TNM criteria.
The CRC was diagnosed in 50 individuals (forming the study group), and 200 patients without CRC diagnosis were included in the control group. Cases and controls were manually matched based on mean age and sex.
Patient peripheral blood samples were collected into 5 ml tubes with EDTA anticoagulant. Genetic material isolation was carried out using Syngen Blood/Cell DNA MiniKiT (Syngen Biotech Sp. z o.o.) technique. In order to detect the MDR1/ABCB1 polymorphism (rs1045642) and establish allele distribution, the light SNP assay with real-time PCR were used using the LightCycler 480 instrument in the Laboratory of Experimental Pharmacogenetics, Department of Clinical Pharmacy and Biopharmacy, Poznan University of Medical Sciences, Poland.
The study was approved by the Ethics Committee of the Medical University of Warsaw.
Statistical analysis
Statistical calculations were performed using Statistica 10 PL (StatSoft Inc. 2011) software. A χ2 test was used to assess qualitative variables. To assess quantitative predictors for normal and abnormal distribution of variables, Student’s t-test and the Mann-Whitney U test were used, respectively. Normal distribution of variables was defined based on fulfilling the hypothesis of a normal distribution for both groups in the Shapiro-Wilk, Kolmogorov-Smirnov, and Lilliefors tests. A univariate logistic regression was performed for quantitative predictors and in grouping variables when statistical significance was present. The univariate logistic regression analysis was performed with an online program (Logistic Regression by John C. Pezzullo, Version 05.07.20, http://statpages.org/logistic.html). The genetic associations were calculated with the online Asso-test (http://www.ekstroem.com/assotest/assotest.html). The statistical significance level was set at α = 0.05. Missing data were removed in pairs for statistical analysis.
Results
The characteristics of the study group are presented in Table I. Cases and controls were age- and sex-matched, so there were no significant differences in these two variables between groups (p > 0.05). Statistical analysis showed no differences between groups with respect to the following anthropometric features: mean weight, mean height, mean body mass index (BMI) value, mean hip circumference, and mean waist-hip ratio (WHR). Waist circumference was higher in the study group compared to controls; however, the relationship was not significant and may be biased due to the missing data.
Table I
Characteristics of the study groups
For the nonparametric variables, we found no differences between groups with respect to the following features: tobacco smoking (current, past, and passive); oral contraceptive intake; liver cirrhosis; alcoholic liver disease; toxic liver injury; viral hepatitis; hypertension; congestive heart failure; chronic renal disease; colonic polyps or family history of colonic polyps; familial adenomatous polyposis; hereditary nonpolyposis colorectal cancer; diverticulosis or family history of diverticulosis; hemorrhoids; family history of ulcerative colitis; Crohn’s disease (CD); family history of lung, breast, prostate, stomach, or thyroid gland cancers; weight loss in the last 6 months; diarrhea; and fresh blood in stool. We also found no differences in the intake of glucocorticoids, hypolipidemic drugs, or aspirin between groups.
The use of non-steroidal anti-inflammatory drugs (NSAIDs) was more frequently reported in the control group (11/34 in the study group vs. 99/97 in the control group; p = 0.002). Constipation was also more frequently reported in the control group (7/27 vs. 86/109; p = 0.01). Ulcerative colitis (8/35 vs. 8/181; p = 0.001, odds ratio (OR) = 5.17; 95% confidence interval (CI): 1.82–14.70) and positive family history of CRC (11/33 vs. 26/172; p = 0.05; OR = 2.25; 95% CI: 0.99–4.90) were more frequent in the study group.
Diabetes (12/34 vs. 28/170; p = 0.04) increased the risk of CRC 2.14-fold (OR = 2.14; 95% CI: 0.99–4.63). In both cohorts, diabetes mellitus (DM) type 2 was the dominant diabetes subtype.
Past hormone replacement therapy was observed more frequently in the study group, but this difference was not statistically significant (31/23 vs. 20/79; p = 0.06). Family histories of CD and pancreatic cancer were observed more frequently in the study group than in the control group (1/44 vs. 0/200; p = 0.03 and 2/43 vs. 0/197; p = 0.003, respectively).
The frequency of alleles in the control group was similar to the diversity of the rs1045642 polymorphism in the European population based on the NCBI db SNP Short Genetic Variation allele frequencies (HapMap-CEU ss35072275: C/C 0.15; C/T 0.56; T/T 0.29 vs. controls, p > 0.05).
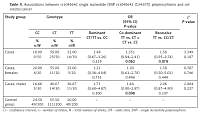
In the present study, allele T of SNP rs1045642 was observed slightly more frequently in the study group; however, this finding was not statistically significant. This relationship between the T allele and CRC was most visible in the co-dominant and recessive models. An association between the T allele and male sex was also revealed in a co-dominant model. The associations of SNP rs1045642 in the study and control groups are presented in Table II.
Table II
Associations between rs1045642 single nucleotide (SNP rs1045642 (C3435T)) polymorphisms and colorectal cancer
Discussion
The general risk factors of CRC are well known; among them, obesity plays an important role [44]. The correlation between gender and BMI in the risk of CRC has been noted in the literature, and it primarily concerns men [45–47]. This difference may be due to hormonal differences between sexes and the resultant changes in the distribution of fat tissue within the body (e.g. abdominal obesity in men) [44, 48].
In this study, we observed a correlation between waist circumference and risk of CRC. In 2014, Brandstedt et al. explored the correlation between anthropometric factors and CRC caused by KRAS and BRAF mutations [44]. They observed that high weight, hip, waist, WHR, and BMI values were associated with an increased risk of BRAF wild type tumors, but none of the anthropometric factors were associated with risk of BRAF-mutated CRC, either in the overall or in the sex-stratified analysis. While all anthropometric measures (except height) were associated with an increased risk of KRAS-mutated tumors, only BMI was associated with an increased risk of KRAS wild type tumors overall [44].
When analyzing a German population, Sainz et al. confirmed that men carrying the C allele of the rs1045642 polymorphism are less prone to develop CRC (OR = 0.85, 95% CI: 0.74–0.97, per allele), whereas men with the minor G allele of the rs9282564 polymorphism had an increased risk of CRC [49]. It is suggested that these variants may influence the ABCB1-mediated estrogen efflux from the colonic epithelial cells and therefore modify the risk for CRC. However, the authors claimed that as P-glycoprotein is a transporter of several substances, the effects may not necessarily be solely attributable to altered estrogen transport, especially in men [49].
In contrast, Martinelli et al. observed that the MDR1/ABCB1 polymorphisms rs1128503, rs2032582, and rs1045642 had no impact on CRC risk [50]. However, the study described an association of MDR1/ABCB1 with CRC localization in the sigmoid colon and an influence on gender ratio in CRC patients [50]. These results confirm sex-specificity of MDR1/ABCB1 in CRC patients, supporting the data presented in this study.
A Danish population based study by Kopp et al. showed that the MDR1/ABCB1 rs1045642 and ABCG2 rs2231137 haplotypes were associated with a risk of CRC, and that rs1045642 interacted with intake of cereals and fiber [51]. Meanwhile, Zhao et al. provided evidence that rs1045642 is not associated with an increased risk of CRC in a study involving 11,339 individuals in the Asian and Caucasian population [52]. A meta-analysis of 39 case-control studies by Sheng et al. confirmed the impact of this polymorphism on the overall risk of cancer in TT carriers compared to CT and CC genotypes; however, the results suggested a stronger association with hematologic malignancies [53].
In this study, we more frequently observed the presence of ulcerative colitis in patients with CRC compared to the control group. Inflammatory bowel diseases (IBD), including ulcerative colitis and CD, are known to increase the risk of CRC. Indeed, according to a meta-analysis performed in 2013 by Johnson et al., IBD increases the risk of CRC 2.93-fold [54]. This meta-analysis also showed that the development of CRC in first-degree relatives is associated with an increased CRC risk of up to 1.79-fold [54]. Likewise, we found that a positive family history of CRC was observed more frequently in CRC patients compared to the control group. Finally, diabetes was observed more often in CRC patients than in the control group, which is in accordance with previous studies showing that individuals with diabetes are at a 27% higher risk of developing CRC [55].
In conclusion, our study indicates that the T allele of rs 1045642 is more frequent in males with CRC. This suggests that the MDR1/ABCB1 gene polymorphism rs 1045642 may be involved in the pathogenesis of CRC in a sex-specific manner. Further population studies are necessary to explore this association.