Introduction
The number of geriatric patients who present to emergency departments increases every day due to the increasing proportion of the geriatric population among the general population in addition to the prolongation of life [1]. Whereas 8.2% of the population in Turkey was over 65 years of age in 2015, this percentage is expected to reach 10.1% in 2023 [2]. The city of Izmir is highly popular among the geriatric population due to its climate and living conditions and the rate of increase of the geriatric population in Izmir is 10% according to the data obtained from the Turkish Statistical Institute [2]. The rates for presentation of geriatric patients to emergency departments identified in studies carried out abroad vary between 8% and 19% [3, 4].
In addition to the high mortality rates, traumas that induce a loss of functions and independent living conditions from other people may result in significant morbidity in geriatric patients. Mortality rates during hospitalization range from 15% to 45% in studies carried out on geriatric trauma patients [5]. Traumas are ranked fifth among the causes of death in patients over the age of 65 [3]. Geriatric patients are more prone to risk of trauma due to age-related motor and cognitive impairments as well as the more active lives they nowadays lead [6]. Even minor traumas can cause severe injuries in geriatric patients, and when compared with other age groups, the mortality and morbidity rates are higher [7]. This is not specific to our country; it is a universal fact common to all hospitals, emergency departments and healthcare staff all over the world [7, 8].
The objective of this study was to determine the demographic and epidemiological features of geriatric patients with traumas admitted to our hospital.
Material and methods
Study plan
In the study, patient cards prepared at the emergency department for trauma patients aged 65 and above who presented to the emergency department between the dates of September 30, 2014 and October 01, 2015 along with data obtained from the hospital information management system were evaluated retrospectively. Ethical council approval was not obtained since our study was planned retrospectively, but the Helsinki Declaration was followed as the guideline in this study.
Patients for whom no additional data could be acquired other than them being a “trauma case”, those with missing data in their folders and those who left the hospital on their own accord without any physical examination were excluded from the study.
Data related to the age, gender, time of admission to the emergency department, medical history and medications of patients were classified. Data regarding the consultation departments, the imaging techniques that were used for the patients, diagnoses of admitted discharged or exitus patients as well as the mechanisms of trauma were evaluated. The subjects were classified according to their age into two groups as patients aged 65–79 and patients over 80, after which their differences were analyzed with regard to the variables.
The mechanisms of trauma were classified as fall, trauma of the extremity, blow, traffic accident, gunshot injuries, stabbing, or burns, and the inflicted body parts were classified as head and neck, thorax, abdomen, extremity and multiple traumas.
Statistical analysis
Data obtained were evaluated via SPSS 18.0, while the demographic distributions of patients was assessed through mean ± standard deviation, and differences between the two groups were analyzed by the Mann-Whitney U test. The χ2 test was used to examine the relationship between trauma mechanisms and the resulting injury. Pearson’s χ2 test and Fisher’s exact test were used to group and compare the data. All hypotheses were bidirectional and the value of p ≤ 0.05 was accepted as statistically significant.
Results
A total of 240 314 patients were admitted to the emergency department during our study. Among these patients, 9.1% (n = 21 850) were over 65 years of age and 4.1% (n = 1630) were trauma patients. Of the 912 trauma patients who were included in the study, 60.4% were female, and 39.6% were male. The mean age was 77.16 (65–100). 60.4% of all the admitted patients were over 65 years of age, and 39.6% were over 80 years of age.
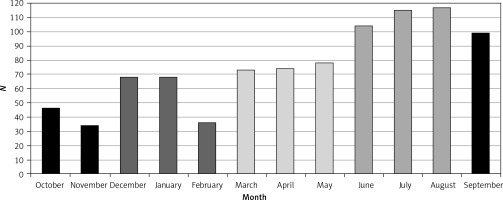
The highest number of admissions occurred during summer (36.8%) and spring (24.7%). The months during which the highest number of admissions took place were August (12.8%), July (12.6%) and June (11.4%) (Figure 1).
An ambulance was used to bring in 45.5% of the patients, whereas 54% arrived by other means. There was at least one disease diagnosed in the medical history of 69.4% of the patients. The underlying first three diseases were hypertension (HT) (32.1%), coronary artery disease (CAD) (16.8%) and diabetes mellitus (DM) (16.4%). Statistically significant differences were found when the prevalences of cerebrovascular disease (p = 0.034), Alzheimer disease-dementia (p = 0.001) and asthma-chronic obstructive pulmonary disease (COPD) (p = 0.015) were compared for patients who were 80 or over with those aged 65–79. No statistically significant difference was found between the age groups with regard to other coexisting diseases (p > 0.05) (Table I).
Table I
General characteristics of the geriatric trauma patients according to age groups
| Geriatric trauma patients | Total n (%) | Age 65–79 years n (%) | Age over 80 years n (%) |
|---|---|---|---|
| Gender: | |||
| Female | 551 (60.4) | 331 (60.1) | 220 (60.9) |
| Male | 361 (39.6) | 220 (39.9) | 141 (39.1) |
| Arrival type: | |||
| Other transportation | 497 (54.5) | 334 (60.6) | 163 (45.2) |
| Ambulance | 415 (45.5) | 217 (39.4) | 198 (54.8)* |
| Coexisting disease: | |||
| Hypertension | 293 (32.1) | 168 (30.5) | 125 (34.6) |
| Coronary artery disease | 153 (16.8) | 83 (15.1) | 70 (19.4) |
| Diabetes | 150 (16.4) | 101 (18.3) | 49 (13.6) |
| Alzheimer-dementia | 53 (5.8) | 15 (2.7) | 38 (10.5)* |
| Asthma-COPD | 50 (5.5) | 22 (4) | 28 (7.8)* |
| Cerebrovascular disease | 21 (2.3) | 8 (1.3) | 13 (3.6)* |
| Using drug: | |||
| Antihypertensive/antiarrhythmic | 386 (42.3) | 222 (40.3) | 164 (45.4) |
| Antiepileptics/antipsychotic antiparkinson/dementia | 85 (9.3) | 28 (5.1) | 57 (15.8)* |
| Inhalers/steroids | 50 (5.5) | 22 (4) | 28 (7.8)* |
| Antiaggregants | 34 (3.7) | 21 (3.8) | 13 (3.6) |
| Oral antidiabetics/insulin | 149 (16.3) | 100 (18.1) | 49 (13.6) |
| Site of trauma: | |||
| Extremity | 533 (58) | 320 (58.1) | 213 (59) |
| Head-neck | 239 (26.2) | 136 (24.7) | 103 (28.5) |
| Thorax | 70 (7.6) | 49 (8.9) | 21 (5.8) |
| Multiple | 62 (6.7) | 41 (7.4) | 21 (5.8) |
| Abdomen | 8 (0.8) | 5 (0.9) | 3 (0.8) |
| Mechanism of trauma: | |||
| Fall | 780 (86) | 438 (71.5) | 342 (94.7)* |
| Traffic accident | 67 (7.3) | 56 (10.2) | 11(3)* |
| Burn | 29 (3.1) | 23 (4.2) | 6 (1.7)* |
| Blow | 20 (2.1) | 20 (3.6) | 0 |
| Trauma of extremity | 9 (1) | 7 (1.3) | 2 (0.6) |
| Gunshot injuries | 4 (0.4) | 4 (0.7) | 0 (0) |
| Being stabbed | 3 (0.3) | 3 (0.5) | 0 (0) |
| Imaging: | |||
| X-ray | 649 (71.2) | 396 (71.9) | 253 (70.1) |
| Computed tomography | 575 (62.9) | 328 (59.5) | 246 (68.1)* |
| Ultrasonography | 91 (10) | 71 (12.9) | 20 (5.5)* |
| Consultation: | |||
| Yes | 509 (55.8) | 276 (50.1) | 233 (61.5)* |
| No | 453 (44.2) | 275 (49.9) | 128 (31.5) |
| Final outcome: | |||
| Admission | 264 (28.9) | 130 (23) | 134 (36.5) |
| Discharge | 630 (69.1) | 421 (74.9) | 227 (61.8) |
| Exitus | 18 (2) | 12 (2.1) | 6 (1.6) |
Of the patients, 67.1% were using at least one drug and 32.9% were using two or more drugs. The two most common medications among trauma patients aged above 65 were cardiac drugs (antihypertensive, antiarrhythmic etc.) (42.3%) and antidiabetic drugs (oral antidiabetics, insulin) (16.3%). The top three most frequent mechanisms for trauma were falls (85.5%), traffic accidents (7.3%) and burns (3.2%) (Table I).
Whereas female patients were admitted to the emergency department mostly due to falls, the most common reason of admission for male patients was traffic accidents (Table II). The first three leading diseases among patients admitted to the hospital due to falls were HT (33.5%), CAD (16.7%) and DM (16.8%). Falls were commonly observed in patients in the age group below 80, whereas traffic accidents and burns were common for the above 80 age group. All blow-related admissions took place for patients under the age of 80 (Table I).
Table II
Final diagnosis incidences according to age groups and final outcomes in all patients
According to the sites of trauma, the most common site was extremities (58%) followed by head and neck (26%). Female patients commonly presented with extremity traumas whereas male patients commonly presented with head and neck traumas (Table III).
Table III
Gender distribution according to mechanism of trauma and site of the trauma in geriatric trauma patients
| Geriatric trauma patients | Gender | Total n (%) | |
|---|---|---|---|
| Female n (%) | Male n (%) | ||
| Mechanism of trauma: | |||
| Fall | 484 (87.8)* | 296 (82.0) | 780 (85.5) |
| Traffic accident | 32 (5.8) | 35 (9.7)* | 67 (7.3) |
| Burn | 19 (3.4) | 10 (2.8) | 29 (3.2) |
| Blow | 12 (2.2) | 8 (2.2) | 20 (2.1) |
| Extremity trauma | 3 (0.5) | 6 (1.7) | 9 (0.9) |
| Gunshot injury | 0 (0) | 4 (1.1)* | 4 (0.4) |
| Being stabbed | 1 (0.2) | 2 (0.6) | 3 (0.3) |
| Site of trauma: | |||
| Extremity | 357 (64.8)* | 176 (48.8) | 533 (58.4) |
| Head neck | 114 (20.7) | 125 (34.6)* | 239 (26.2) |
| Thorax | 38 (6.9) | 32 (8.9) | 70 (7.6) |
| Multiple | 39 (7.1) | 23 (6.4) | 62 (6.7) |
| Abdomen | 3 (0.5) | 5 (1.4) | 8 (0.8) |
At least one consultation was carried out for 55% of the patients. The consultation departments were orthopedics (40.2%), brain surgery (14.3%) and general surgery (4.5%). Consultation request was determined to be statistically significant for the age group of 80 and above (p = 0.03). At least a single plain radiograph was requested for 71.2% of the patients who presented with trauma. Computed tomography (CT) was requested for 62.9% of the patients and ultrasonography (USG) was requested for 10% of the patients. X-ray radiography was requested for 72.4% of the patients who were admitted to the emergency due to falls, CT for 63.6% and USG for 5%. The CT request rate was high for the age group of 80 and above (p = 0.008), whereas USG request was high for the age group of below 80.
The first five diagnoses of our patients were soft tissue trauma (40.4%), femur fracture (13.8%), minor head trauma (8.1%), pelvic fracture (7.9%) and forearm fracture (5.2%) (Table II).
A total of 28.9% of the patients were hospitalized and 2% were exitus. The first three departments of admission for patients were orthopedics (80.3%), brain surgery (14%) and general surgery (3%). Of the exitus patients, 77.8% were male and the mean age was 78 (68–95 years of age). The mechanisms of trauma were falls (77.7%), traffic accidents (11.1%) and gunshot injuries (11.1%). The first two leading diagnoses in both groups aged below and above the 80 were femur fractures and pelvic fractures. The leading diagnosis for patients who died was femur fracture with a rate of 33.3% (n = 6); the other diagnoses were subdural hemorrhage with a rate of 22.2% (n = 4), subarachnoid hemorrhage (SAH) with a rate of 11.1% (n = 2) and intracranial hemorrhage with a rate of 11.1% (n = 2). It was determined that 66.6% (n = 12) of the exitus patients were under the age of 80 and that the most common diagnosis was subdural hematoma (25%). The most common diagnosis for patients in the above 80 age group was femur fracture (66.7%). There was no statistically significant difference between the groups (p > 0.05) (Table II) with regard to the means of final diagnosis distribution.
Discussion
The response of elderly individuals to trauma are limited by their physiological reserves [9]. Decrease in cardiac output and decrease in the supply of sufficient tissue oxygenation during stress occur with increasing age. Muscular atrophy, osteoporosis and reduced subcutaneous tissue result in more significant injuries due to traumas in elderly individuals [10].
The admissions of geriatric patients to emergency departments increase over the years and it was found in studies carried out in foreign countries that the ratios varied between 8% and 23% [3, 11, 12]. In our study, 9.1% of those who applied for emergency admissions were above 65 years of age. This rate was between 2.1% and 5% in studies that were carried out in Turkey [13, 14]. It was observed in our study that 4.1% of geriatric admissions were geriatric trauma patients. This proportion is lower than the figures in comprehensive series in the literature, though it shows similarities with studies that involve the city of Izmir as well as the nearby cities [11, 12].
There was a female predominance (60.4%) in geriatric trauma admissions in our study with a mean age of 77.1. There was also a female predominance for the age groups 65–79 and above 80 years of age. The male gender ratio was determined to be high in studies carried out by Yıldız et al. (63.9%), Akkose Aydın et al. (62.3%), Ekci et al. (51.7%), Aktaş et al. (52.7%) and Guneytepe et al. (52%) [15–19]. However, 65.23% of all patients in the study by Fama et al. and 76% of all patients in the study by McGwin et al. were women, and these results were in accordance with those of our study [20, 21].
The mobility of patients decreases with increasing age, additional diseases increase and their motor abilities reduce. Trauma rates increase with increasing age due to all the aforementioned reasons [22, 23]. The average age in our study was about 77.1. It was reported as 71.9 by Akkose et al., Ekci et al. reported it as 73.3 years, Aktaş et al. as 73 years and Guneytepe et al. as 72.0 years [16–19]. Moreover, studies carried abroad have similar results in general [22, 24, 25].
The most frequent admissions took place during the summer season (36.8%); during the months of August and July. Akoğlu et al. reported that 32% of the geriatric trauma patient admissions took place in the months of spring and that 31% took place in autumn [6]. Admissions to the hospital were observed at different time frames and seasons in other studies carried out at the national level depending on the properties of the local regions [26, 27].
It was found in a study that the rate of ambulance service usage of geriatric patients in our city was approximately 51% [28]. The rate of admission via ambulance was 45.5% in our study and the rate of admission via ambulance was higher for patients above the age of 80. There are studies indicating the rates for emergency department admissions via ambulance that are greater than 54% for geriatric patients [29]. It can be suggested that the ambulance service usage rate can change with some other factors such as the extent of the city, transport facilities, and the practice of the patients to use health facilities.
Morris et al. carried out a study in which it was shown that the existence of accompanying diseases is a risk factor that increases the mortality and that significant results may occur due to low energy injuries. In contrast, Milzman et al. carried out a study in which it was determined that the existence of accompanying diseases is an independent risk factor with regard to mortality in elderly individuals [30, 31]. Neuronal degeneration occurs in the central nervous system with increasing age as well as a decrease in the respiratory system capacity [32]. The rate of the presence of at least one chronic disease was 69.4% in our study. The leading three diseases were HT, CAD and DM. The first three diseases observed in the study carried out by Abdulhayoğlu et al. were the same [13]. There were statistically significant differences in the incidences of cerebrovascular disease, Alzheimer’s disease-dementia and asthma-COPD in the group aged above 80.
In our study, 67.1% of the patients were taking at least one medication. The two most common medications were cardiovascular drugs (antihypertensive, antiarrhythmic etc.) and diabetes drugs (oral antidiabetics, insulin). These findings were in accordance with those of the previous studies [11, 14].
The order of frequency of trauma mechanisms show significant differences depending on the clinics, countries and years [33]. Falls are the most commonly observed injuries and the most frequent cause of age-related deaths [34]. Personal factors are as important in their formation as environmental factors. Accompanying diseases observed in patients increase the risks of physiological changes and drug use as well [35]. Falls generally take place on flat surfaces and from relatively low heights such as steps of stairs [35]. In our study, the first three causes of application to the emergency department were falls, traffic accidents and burns. This pattern shows similarities with the other studies on geriatric trauma causes carried out in our country [12, 14, 33].
Risk of falling increases with aging due to the progression of physiological changes such as decreases in vision and hearing perceptions, decreases in motor strength as well as due to the medications being used [36, 37]. It has been stated that this risk is higher in patients above 75 years of age [11, 12]. Admissions due to falls were higher in patients above 80 years of age in our study in accordance with the relevant literature. 1.8% of the patients who presented with falls died. This rate was reported as 3.3% in the study carried out by Abdulhayoğlu et al. [13].
The admission rates due to falls were higher in female patients compared to males. This was thought to be related to weaker abilities of muscle strength and motor activity of women compared with men and the fact that these abilities decrease with aging [7, 23]. Male patients were admitted more frequently due to motor vehicle accidents. Various other studies have also been published which show that traffic accidents are observed more frequently in elderly individuals with traumas [22, 25].
When body parts affected by trauma were examined, it was observed that geriatric patients were exposed to traumas of the extremities as well as those of the head and neck and that the findings were in accordance with the relevant literature [38, 39]. Trauma of the extremities was observed more frequently in female patients, whereas trauma of the head and neck was more frequent in male patients. The body parts exposed to trauma according to the distribution of gender showed similarities with the mechanisms of trauma according to the distribution of gender.
The most common consultation department was orthopedics. The results for the consultation rate and the consultation departments were in accordance with relevant studies in the literature [28, 29].
At least one X-ray radiography was requested for 71.2% of the patients. These findings were similar to those of the studies carried out by Abdulhayoğlu et al. and Aktürk et al. [13, 33]. Abdulhayoglu et al. reported that radiography (82.1%), CT (44.4%) and USG examinations (2.7%) were requested from the patients.
28.9% of the patients were hospitalized. The first three departments were orthopedics (80.3%), brain surgery (14%) and general surgery (3%). The hospitalization rate was higher at a statistically significant level for female patients above 80 years of age. It is known that female patients have a higher risk of trauma of the extremities due to the age-related alterations in the bone and joint configurations, osteoporosis and osteopenia; that they have a tendency for fractures and that most of the fractures require an operation [37, 40]. In the study carried out by Abdulhayoglu et al., 67.3% of the patients were discharged from the emergency department, 22.4% of the patients were hospitalized (68.7% of them in the orthopedics department, 13.3% of them in the brain surgery department, 5.3% of them in the general surgery department). These results were similar to those of our study.
Pelvic and femur fractures resulting from direct falls were more common in geriatric patients due to age-related physical disabilities and the diminished defense reflex that is thought to be related to physiological changes. Pelvic and femur fractures were more common for patients above the age of 80 in our study.
Compared with younger patients, elderly patients showed higher rates of morbidity and mortality due to falls and motor vehicle accidents, with reported mortality rates ranging from 2.6% to 38%. The mortality rate was determined as 2% in our study [22, 25, 39, 41].
The mean age of the patients in our study was 78 and the death rate was higher for the male gender. The leading diagnoses for exitus patients were femur fracture complications, whereas other diagnoses were subdural hemorrhage and subarachnoid hemorrhage [3, 5, 8, 12].
There were a few limitations in our study. The first one was that it was a single centre study and another one was that it was retrospective. The last limitation was that our recordings were not sufficient for a wider study.
In conclusion, the number of geriatric patients with trauma is increasing continuously. The response of the geriatric population to trauma and physiological reserves is insufficient. Failure of the body’s adaptation mechanism to traumas increases the severity of injuries. A multidisciplinary and aggressive diagnosis and treatment approach should be followed for the care of these patients when all comorbidities are taken into consideration.