Introduction
Sleeve gastrectomy (SG) has recently become one of the most common bariatric procedures worldwide. Some authors consider SG to be an ideal bariatric procedure [1–3]. In 2013, there was a significant increase in the utilisation of laparoscopic SG in the largest academic centres of the United States; as a result, the popularity of SG surpassed that of laparoscopic Roux-en-Y gastric bypass [4]. SG allows the patient to achieve satisfactory loss of excess body weight and resolution of obesity-related comorbidities, including type 2 diabetes mellitus, hypertension, and dyslipidaemia [5]. Staged approaches to the surgical treatment of morbid obesity often include SG as an initial procedure, but SG is also implemented as a singular and primary bariatric operation [6, 7]. Moreover, SG seems to be a more cost-effective choice of treatment compared with laparoscopic Roux-en-Y gastric bypass [8, 9].
Despite the high effectiveness of SG in both the short and long term, thorough scientific investigation is required to correctly understand the mechanisms underlying this bariatric procedure. These mechanisms should be the main focus of current research, in contrast to the development of new operations and techniques [10]. At present, SG is one of the most frequently and thoroughly studied areas in bariatric surgery.
Many recent publications have focused on the 100 most frequently cited papers investigating various surgical topics. The role of this type of research is to underline which authors, bariatric centres, countries, or journals have most strongly influenced advances in surgery [11–13]. Previous studies conducting bibliometric analyses in the field of bariatric and metabolic surgery focused on this subject as a whole and had several methodological shortcomings [14]. We believe that bibliometric analysis of a specific bariatric operation, which has rapidly gained popularity in recent years, would provide valuable insight into the current development of trends in the surgical treatment of obesity.
Aim
Our objective was to analyse and summarise the characteristics of the most frequently cited studies focusing on SG.
Material and methods
Study design
We used the Web of Science database (Thomson Reuters, Philadelphia, PA, USA) to identify all studies focused on SG as a bariatric procedure, published from 2000 to 2018. The terms “sleeve gastrectomy”, “vertical gastrectomy”, “parietal gastrectomy”, and “reduction gastrectomy” were used to conduct the search on 31 December 2018. The search strategy did not include any limitations on language and abstract availability. The inclusion criterion was an original study or secondary source (review or meta-analysis) with the primary focus on SG as a bariatric operation. The search strategy was limited to the period 2000–2018. We excluded publications that did not consider SG as a separate procedure, studies focusing on open surgeries, and animal studies. Articles were ranked based on the number of citations; if two or more articles had the same number of citations, they were then ranked based on the year of publication. We excluded studies with fewer than 50 citations. Two independent reviewers assessed the list and selected the 100 most frequently cited studies with a focus on SG by reviewing the titles and abstracts of all identified records. A third reviewer compared the two lists, discussed the differences, and resolved any conflicts. All articles included in the list of 100 were retrieved.
Outcomes of interest
Data were extracted independently by the two reviewers. When a disagreement was encountered, a consensus was reached by discussion with a third reviewer. During the full-text screening, the reviewers extracted the following data: title, primary and senior authors’ names, total number of authors and their department of origin (academic/non-academic, surgical/non-surgical, and single-centre/multi-centre), year of publication, number of citations, citations per year, continent, country, journal, focus of the journal (bariatric surgery, general surgery, general medicine), journal origin, impact factor in 2017, immediacy index, study type (clinical experience, basic science, review), article type (case series, observational study, randomised clinical trial, basic science, review/expert opinion, systematic review, meta-analysis), funding source, and level of evidence (I–V) assessed in accordance with publication by Wright et al. [15] and the subject of the study.
Statistical analysis
Statistical analysis was performed using Statistica 12 Software (StatSoft Inc., Tulsa, OK, USA). The Shapiro-Wilk test was used to assess the data distribution. Continuous variables are presented as arithmetical means with standard deviations. Correlations were assessed using Spearman’s test. The Mann-Kendall trend test was used to determine time-dependent trends. A p-value of < 0.05 was considered statistically significant.
Results
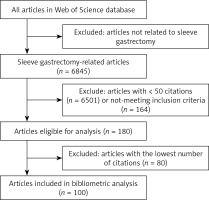
Our search strategy revealed 6845 records related to SG. Overall, 180 publications were focused on SG and contained a total of ≥ 50 citations. The 100 most frequently cited publications were included in the final list (Table I) [15–117]. A flowchart of the study is presented in Figure 1.
Table I
The 100 most cited articles in laparoscopic sleeve gastrectomy
| Rank | First author | Publication year | Title | Journal | Impact factor (publication year) | Total citations |
|---|---|---|---|---|---|---|
| 1 | Karamanakos [16] | 2008 | Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy – a prospective, double blind study | Ann Surg | 8.460 | 493 |
| 2 | Himpens [20] | 2006 | A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years | Obes Surg | 3.723 | 413 |
| 3 | Cottam [21] | 2006 | Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity | Surg Endosc | 1.969 | 396 |
| 4 | Rosenthal [22] | 2012 | International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of > 12,000 cases | Surg Obes Relat Dis | 4.121 | 393 |
| 5 | Himpens [23] | 2010 | Long-term results of laparoscopic sleeve gastrectomy for obesity | Ann Surg | 7.474 | 381 |
| 6 | Ryan [118] | 2014 | FXR is a molecular target for the effects of vertical sleeve gastrectomy | Nature | 41.456 | 365 |
| 7 | Langer [24] | 2005 | Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels | Obes Surg | 3.759 | 350 |
| 8 | Peterli [25] | 2009 | Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy a prospective randomized trial | Ann Surg | 7.900 | 347 |
| 9 | Hutter [26] | 2011 | First report from the American College of Surgeons Bariatric Surgery Center Network Laparoscopic Sleeve Gastrectomy has morbidity and effectiveness positioned between the band and the bypass | Ann Surg | 7.492 | 311 |
| 10 | Baltasar [27] | 2005 | Laparoscopic sleeve gastrectomy: a multi-purpose bariatric operation | Obes Surg | 3.759 | 300 |
| 11 | Brethauer [28] | 2009 | Systematic review of sleeve gastrectomy as staging and primary bariatric procedure | Surg Obes Relat Dis | 3.826 | 287 |
| 12 | Bohdjalian [29] | 2010 | Sleeve gastrectomy as sole and definitive bariatric procedure: 5-year results for weight loss and ghrelin | Obes Surg | 3.078 | 268 |
| 13 | Aurora [30] | 2012 | Sleeve gastrectomy and the risk of leak: a systematic analysis of 4,888 patients | Surg Endosc | 3.427 | 253 |
| 14 | Weiner [31] | 2007 | Laparoscopic sleeve gastrectomy – influence of sleeve size and resected gastric volume | Obes Surg | 2.852 | 248 |
| 15 | Melissas [32] | 2007 | Sleeve gastrectomy – a restrictive procedure? | Obes Surg | 2.852 | 239 |
| 16 | Lee [33] | 2011 | Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus a randomized controlled trial | Arch Surg | 4.422 | 236 |
| 17 | Gagner [34] | 2009 | The Second International Consensus Summit for Sleeve Gastrectomy, March 19–21, 2009 | Surg Obes Relat Dis | 3.826 | 222 |
| 18 | Deitel [35] | 2008 | The First International Consensus Summit for sleeve gastrectomy (SG), New York city, October 25–27, 2007 | Obes Surg | 2.913 | 219 |
| 19 | Silecchia [36] | 2006 | Effectiveness of laparoscopic sleeve gastrectomy (first stage of biliopancreatic diversion with duodenal switch) on co-morbidities in super-obese high-risk patients | Obes Surg | 3.723 | 218 |
| 20 | Peterli [37] | 2012 | Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, prospective trial | Obes Surg | 3.102 | 217 |
| 21 | Birkmeyer [38] | 2010 | Hospital complication rates with bariatric surgery in Michigan | JAMA | 30.011 | 211 |
| 22 | Han [39] | 2005 | Results of laparoscopic sleeve gastrectomy (LSG) at 1 year in morbidly obese Korean patients | Obes Surg | 3.759 | 205 |
| 23 | Nocca [40] | 2010 | A prospective multicenter study of 163 sleeve gastrectomies: results at 1 and 2 years | Obes Surg | 2.913 | 200 |
| 24 | DeMaria [41] | 2010 | Baseline data from American Society for Metabolic and Bariatric Surgery-designated Bariatric Surgery Centers of Excellence using the Bariatric Outcomes Longitudinal Database | Surg Obes Relat Dis | 3.173 | 196 |
| 25 | Deitel [42] | 2011 | Third International Summit: current status of sleeve gastrectomy | Surg Obes Relat Dis | 3.929 | 194 |
| 26 | Kehagias [43] | 2011 | Randomized clinical trial of laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy for the management of patients with BMI < 50 kg/m(2) | Obes Surg | 3.286 | 186 |
| 27 | Peterli [44] | 2013 | Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS) a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass | Ann Surg | 7.188 | 185 |
| 28 | Gehrer [45] | 2010 | Fewer nutrient deficiencies after laparoscopic sleeve gastrectomy (LSG) than after laparoscopic Roux-y-gastric bypass (LRYGB) – a prospective study | Obes Surg | 3.078 | 182 |
| 29 | Vidal [46] | 2008 | Type 2 diabetes mellitus and the metabolic syndrome following sleeve gastrectomy in severely obese subjects | Obes Surg | 2.913 | 182 |
| 30 | Saber [47] | 2008 | Single incision laparoscopic sleeve gastrectomy (SILS): a novel technique | Obes Surg | 2.913 | 179 |
| 31 | Gumbs [48] | 2007 | Sleeve gastrectomy for morbid obesity | Obes Surg | 2.852 | 176 |
| 32 | Abbatini [49] | 2010 | Long-term effects of laparoscopic sleeve gastrectomy, gastric bypass, and adjustable gastric banding on type 2 diabetes | Surg Endosc | 3.436 | 175 |
| 33 | Parikh [50] | 2013 | Surgical strategies that may decrease leak after laparoscopic sleeve gastrectomy a systematic review and meta-analysis of 9991 cases | Ann Surg | 7.188 | 173 |
| 34 | Yehoshua [51] | 2005 | Laparoscopic sleeve gastrectomy – volume and pressure assessment | Obes Surg | 2.913 | 171 |
| 35 | Shi [52] | 2010 | A review of laparoscopic sleeve gastrectomy for morbid obesity | Obes Surg | 3.078 | 170 |
| 36 | Mognol [53] | 2005 | Laparoscopic sleeve gastrectomy as an initial bariatric operation for high-risk patients: initial results in 10 patients | Obes Surg | 3.759 | 169 |
| 37 | Pratt [54] | 2009 | Best practice updates for pediatric/adolescent weight loss surgery | Obesity | 3.366 | 163 |
| 38 | Roa [55] | 2006 | Laparoscopic sleeve gastrectomy as treatment for morbid obesity: technique and short-term outcome | Obes Surg | 3.723 | 162 |
| 39 | Lalor [56] | 2005 | Complications after laparoscopic sleeve gastrectomy | Surg Obes Relat Dis | 3.862 | 159 |
| 40 | Sakran [57] | 2013 | Gastric leaks after sleeve gastrectomy: a multicenter experience with 2,834 patients | Surg Endosc | 3.313 | 156 |
| 41 | Gagner [58] | 2008 | Laparoscopic sleeve gastrectomy is superior to endoscopic intragastric balloon as a first stage procedure for super-obese patients (BMI ≥ 50) | Obes Surg | 3.759 | 156 |
| 42 | Melissas [59] | 2008 | Sleeve gastrectomy – a food limiting operation | Obes Surg | 2.913 | 155 |
| 43 | Lee [60] | 2007 | Vertical gastrectomy for morbid obesity in 216 patients: report of two-year results | Surg Endosc | 2.242 | 150 |
| 44 | Carlin [61] | 2013 | The comparative effectiveness of sleeve gastrectomy, gastric bypass, and adjustable gastric banding procedures for the treatment of morbid obesity | Ann Surg | 7.188 | 149 |
| 45 | Consten [62] | 2004 | Decreased bleeding after laparoscopic sleeve gastrectomy with or without duodenal switch for morbid obesity using a stapled buttressed absorbable polymer membrane | Obes Surg | 3.726 | 148 |
| 46 | Gagner [63] | 2013 | Survey on laparoscopic sleeve gastrectomy (LSG) at the Fourth International Consensus Summit on Sleeve Gastrectomy | Obes Surg | 3.739 | 147 |
| 47 | Fuks [64] | 2009 | Results of laparoscopic sleeve gastrectomy: a prospective study in 135 patients with morbid obesity | Surgery | 3.603 | 143 |
| 48 | D’Hondt [65] | 2011 | Laparoscopic sleeve gastrectomy as a single- stage procedure for the treatment of morbid obesity and the resulting quality of life, resolution of comorbidities, food tolerance, and 6-year weight loss | Surg Endosc | 4.013 | 140 |
| 49 | Langer [66] | 2006 | Does gastric dilatation limit the success of sleeve gastrectomy as a sole operation for morbid obesity? | Obes Surg | 3.723 | 140 |
| 50 | Gill [67] | 2010 | Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review | Surg Obes Relat Dis | 3.173 | 139 |
| 51 | Casella [68] | 2009 | Nonsurgical treatment of staple line leaks after laparoscopic sleeve gastrectomy | Obes Surg | 2.934 | 139 |
| 52 | Jimenez [69] | 2012 | Long-term effects of sleeve gastrectomy and Roux-en-Y gastric bypass surgery on type 2 diabetes mellitus in morbidly obese subjects | Ann Surg | 6.329 | 135 |
| 53 | Nguyen [70] | 2013 | Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy | J Am Coll Surg | 4.454 | 134 |
| 54 | Hamoui [71] | 2006 | Sleeve gastrectomy in the high-risk patient | Obes Surg | 3.723 | 134 |
| 55 | Braghetto [72] | 2009 | Scintigraphic evaluation of gastric emptying in obese patients submitted to sleeve gastrectomy compared to normal subjects | Obes Surg | 2.934 | 131 |
| 56 | Burgos [73] | 2009 | Gastric leak after laparoscopic-sleeve gastrectomy for obesity | Obes Surg | 2.934 | 128 |
| 57 | Lakdawala [74] | 2010 | Comparison between the results of laparoscopic sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass in the Indian population: a retrospective 1 year study | Obes Surg | 3.078 | 118 |
| 58 | Chiu [75] | 2011 | Effect of sleeve gastrectomy on gastroesophageal reflux disease: a systematic review | Surg Obes Relat Dis | 3.929 | 114 |
| 59 | Dapri [76] | 2010 | Reinforcing the staple line during laparoscopic sleeve gastrectomy: prospective randomized clinical study comparing three different techniques | Obes Surg | 3.078 | 114 |
| 60 | Nannipieri [77] | 2013 | Roux-en-Y gastric bypass and sleeve gastrectomy: mechanisms of diabetes remission and role of gut hormones | J Clin Endocrinol Metab | 6.310 | 113 |
| 61 | Franco [78] | 2011 | A review of studies comparing three laparoscopic procedures in bariatric surgery: sleeve gastrectomy, Roux-en-Y gastric bypass and adjustable gastric banding | Obes Surg | 3.286 | 113 |
| 62 | Serra [79] | 2009 | Treatment of gastric leaks with coated self-expanding stents after sleeve gastrectomy | Obes Surg | 2.852 | 112 |
| 63 | Inge [80] | 2014 | Perioperative outcomes of adolescents undergoing bariatric surgery. The Teen-Longitudinal Assessment of Bariatric Surgery (Teen-LABS) Study | JAMA Pediatr | 7.148 | 107 |
| 64 | Chen [81] | 2009 | Reinforcement does not necessarily reduce the rate of staple line leaks after sleeve gastrectomy. A review of the literature and clinical experiences | Obes Surg | 2.934 | 107 |
| 65 | DePaula [82] | 2008 | Laparoscopic treatment of type 2 diabetes mellitus for patients with a body mass index less than 35 | Surg Endosc | 3.231 | 106 |
| 66 | Tucker [83] | 2008 | Indications for sleeve gastrectomy as a primary procedure for weight loss in the morbidly obese | J Gastrointest Surg | 2.311 | 105 |
| 67 | Csendes [84] | 2010 | Management of leaks after laparoscopic sleeve gastrectomy in patients with obesity | J Gastrointest Surg | 2.733 | 102 |
| 68 | DuPree [85] | 2014 | Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease a national analysis | JAMA Surg | 3.936 | 100 |
| 69 | Lee [86] | 2010 | Laparoscopic sleeve gastrectomy for diabetes treatment in nonmorbidly obese patients: efficacy and change of insulin secretion | Surgery | 3.406 | 100 |
| 70 | Eid [87] | 2012 | Laparoscopic sleeve gastrectomy for super obese patients forty-eight percent excess weight loss after 6 to 8 years with 93% follow-up | Ann Surg | 6.329 | 98 |
| 71 | Pournaras [88] | 2012 | Effect of the definition of type II diabetes remission in the evaluation of bariatric surgery for metabolic disorders | Br J Surg | 4.839 | 98 |
| 72 | Finks [89] | 2011 | Predicting risk for serious complications with bariatric surgery results from the Michigan Bariatric Surgery Collaborative | Ann Surg | 7.492 | 98 |
| 73 | Lee [90] | 2011 | Changes in postprandial gut hormones after metabolic surgery: a comparison of gastric bypass and sleeve gastrectomy | Surg Obes Relat Dis | 3.929 | 98 |
| 74 | Frezza [91] | 2009 | Complications after sleeve gastrectomy for morbid obesity | Obes Surg | 2.934 | 98 |
| 75 | Bellanger [92] | 2011 | Laparoscopic sleeve gastrectomy, 529 cases without a leak: short-term results and technical considerations | Obes Surg | 3.286 | 97 |
| 76 | Woelnerhanssen [93] | 2011 | Effects of postbariatric surgery weight loss on adipokines and metabolic parameters: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy-a prospective randomized trial | Surg Obes Relat Dis | 3.929 | 97 |
| 77 | Fischer [94] | 2012 | Excessive weight loss after sleeve gastrectomy: a systematic review | Obes Surg | 3.102 | 96 |
| 78 | Sanchez- Santos [95] | 2014 | Short- and mid-term outcomes of sleeve gastrectomy for morbid obesity: the experience of the Spanish National Registry | Obes Surg | 2.934 | 93 |
| 79 | Black [96] | 2013 | Bariatric surgery for obese children and adolescents: a systematic review and meta-analysis | Obes Rev | 3.739 | 93 |
| 80 | Yousseif [97] | 2014 | Differential effects of laparoscopic sleeve gastrectomy and laparoscopic gastric bypass on appetite, circulating acyl-ghrelin, peptide YY3-36 and active GLP-1 levels in non-diabetic humans | Obes Surg | 3.747 | 92 |
| 81 | Damms-Machado [98] | 2012 | Pre- and postoperative nutritional deficiencies in obese patients undergoing laparoscopic sleeve gastrectomy | Obes Surg | 3.102 | 92 |
| 82 | Braghetto [99] | 2007 | Laparoscopic sleeve gastrectomy: surgical technique, indications and clinical results | Obes Surg | 2.852 | 92 |
| 83 | Gagner [100] | 2003 | Laparoscopic reoperative sleeve gastrectomy for poor weight loss after biliopancreatic diversion with duodenal switch | Obes Surg | 2.421 | 92 |
| 84 | Sarela [101] | 2012 | Long-term follow-up after laparoscopic sleeve gastrectomy: 8–9-year results | Surg Obes Relat Dis | 4.121 | 91 |
| 85 | Arterburn [102] | 2014 | Bariatric surgery for obesity and metabolic conditions in adults | Br Med J | 17.445 | 90 |
| 86 | Alqahtani [103] | 2012 | Laparoscopic sleeve gastrectomy in 108 obese children and adolescents aged 5 to 21 years | Ann Surg | 6.329 | 90 |
| 87 | Braghetto [104] | 2010 | Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients | Obes Surg | 3.078 | 90 |
| 88 | Arias [105] | 2009 | Mid-term follow-up after sleeve gastrectomy as a final approach for morbid obesity | Obes Surg | 2.934 | 89 |
| 89 | Kotidis [106] | 2006 | Serum ghrelin, leptin and adiponectin levels before and after weight loss: Comparisons of three methods of treatment – a prospective study | Obes Surg | 3.723 | 89 |
| 90 | Rawlins [107] | 2013 | Sleeve gastrectomy: 5-year outcomes of a single institution | Surg Obes Relat Dis | 4.942 | 88 |
| 91 | Romero [108] | 2012 | Comparable early changes in gastrointestinal hormones after sleeve gastrectomy and Roux-En-Y gastric bypass surgery for morbidly obese type 2 diabetic subjects | Surg Endosc | 3.427 | 88 |
| 92 | Moize [109] | 2013 | Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-En-Y gastric bypass in a mediterranean population | J Acad Nutr Diet | 2.444 | 87 |
| 93 | Dunn [110] | 2010 | Decreased dopamine type 2 receptor availability after bariatric surgery: preliminary findings | Brain Res | 2.623 | 86 |
| 94 | Trastulli [111] | 2013 | Laparoscopic sleeve gastrectomy compared with other bariatric surgical procedures: a systematic review of randomized trials | Surg Obes Relat Dis | 4.942 | 84 |
| 95 | Manuel Ramon [112] | 2012 | Effect of Roux-en-Y gastric bypass vs sleeve gastrectomy on glucose and gut hormones: a prospective randomised trial | J Gastrointest Surg | 2.361 | 84 |
| 96 | Boza [113] | 2012 | Laparoscopic sleeve gastrectomy as a stand-alone procedure for morbid obesity: report of 1000 cases and 3-year follow-up | Obes Surg | 3.102 | 83 |
| 97 | Soricelli [114] | 2013 | Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or hiatal hernia | Surg Obes Relat Dis | 4.942 | 82 |
| 98 | Vidal [115] | 2007 | Short-term effects of sleeve gastrectomy on type 2 diabetes mellitus in severely obese subjects | Obes Surg | 2.852 | 81 |
| 99 | Akkary [116] | 2008 | Deciphering the sleeve: technique, indications, efficacy, and safety of sleeve gastrectomy | Obes Surg | 2.913 | 80 |
| 100 | Tan [117] | 2010 | Diagnosis and management of gastric leaks after laparoscopic sleeve gastrectomy for morbid obesity | Obes Surg | 3.078 | 79 |
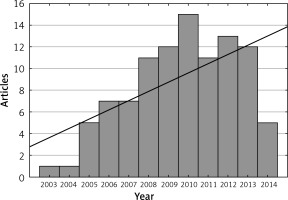
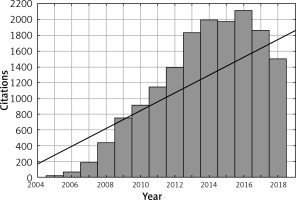
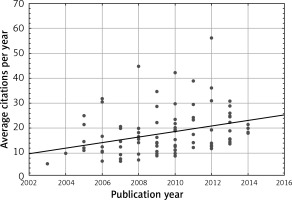
The most frequently cited publication was a study by Karamanakos et al. [16] (493 citations). The article by Ryan et al. [118] had the highest mean number of citations per year (73.00 citations) (Table II). Studies were most frequently published in the years 2010 (15 studies) and 2012 (13 studies) (Figure 2). Articles were most frequently cited in the years 2014 to 2016 (Figure 3). We observed a positive correlation between the citation density and time (r = 0.314, p < 0.05) (Figure 4). The number of citations per year increased with time (r = 0.852, p < 0.05). The number of articles also rose in subsequent years (r = 0.581, p < 0.05).
Table II
Top 10 articles in laparoscopic sleeve gastrectomy based on average citations per year
| Rank | First author | Publication year | Title | Journal | Total citations | Average citations per year |
|---|---|---|---|---|---|---|
| 1 | Ryan [118] | 2014 | FXR is a molecular target for the effects of vertical sleeve gastrectomy | Nature | 365 | 73.00 |
| 2 | Rosenthal [22] | 2012 | International sleeve gastrectomy expert panel consensus statement: best practice guidelines based on experience of >12,000 cases | Surg Obes Relat Dis | 393 | 56.14 |
| 3 | Karamanakos [16] | 2008 | Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy – a prospective, double blind study | Ann Surg | 493 | 44.82 |
| 4 | Himpens [23] | 2010 | Long-term results of laparoscopic sleeve gastrectomy for obesity | Ann Surg | 381 | 42.33 |
| 5 | Hutter [26] | 2011 | First report from the American College of Surgeons Bariatric Surgery Center Network Laparoscopic Sleeve Gastrectomy has morbidity and effectiveness positioned between the band and the bypass | Ann Surg | 311 | 38.88 |
| 6 | Aurora [30] | 2012 | Sleeve gastrectomy and the risk of leak: a systematic analysis of 4888 patients | Surg Endosc | 253 | 36.14 |
| 7 | Peterli [25] | 2009 | Improvement in glucose metabolism after bariatric surgery: comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy a prospective randomized trial | Ann Surg | 347 | 34.70 |
| 8 | Himpens [20] | 2006 | A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: results after 1 and 3 years | Obes Surg | 413 | 31.77 |
| 9 | Peterli [37] | 2012 | Metabolic and hormonal changes after laparoscopic Roux-en-Y gastric bypass and sleeve gastrectomy: a randomized, prospective trial | Obes Surg | 217 | 31.00 |
| 10 | Peterli [44] | 2013 | Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS) a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass | Ann Surg | 185 | 30.83 |
Overall, 64 of the included articles were observational studies, 11 were randomised clinical trials, and eight were systematic reviews. Most of the included publications reported neither commercial nor public funding (79 publications). Public foundations financed 19 studies, and commercial companies financed three studies (Table III).
Table III
Studies characteristics
The included articles were most commonly published in Obesity Surgery (49 articles), followed by Surgery for Obesity and Related Diseases (14 articles) and Annals of Surgery (11 articles). The scope of the journals that published the included studies was mostly focused on bariatric surgery (63 journals) or general surgery (28 journals). Most journals originated from the United States (96 journals) (Table IV).
Table IV
Journals of publication
The most frequent country of origin among the included studies was the United States (38 studies). Eight studies were conducted by institutions from Spain, six by institutions from Italy, and six from Chile (Table V). Most articles were written by authors from academic departments (51 articles). Most articles were published by authors working in a surgical institution (89 articles). They were predominantly conducted in multiple centres (65 studies). The mean number of authors in the included articles was 6.56 ±3.36. Four people were listed as the first author of three articles in our list: Italo Braghetto, Michel Gagner, Wei-Jei Lee, and Ralph Peterli (Table VI). Raul Rosenthal was a senior author in five articles, and Michel Gagner and Nicola Basso were senior authors in four publications (Table VII).
Table V
Countries of origin of included articles
| Country | Number of articles |
|---|---|
| USA | 38 |
| Spain | 8 |
| Chile | 6 |
| Italy | 6 |
| Greece | 5 |
| Switzerland | 5 |
| Belgium | 4 |
| Canada | 4 |
| France | 4 |
| Austria | 3 |
| England | 3 |
| Germany | 3 |
| Taiwan | 3 |
| Israel | 2 |
| Argentina | 1 |
| Australia | 1 |
| Brazil | 1 |
| China | 1 |
| India | 1 |
| Korea | 1 |
Table VI
Authors with more than one first-name article
| First author | Number of articles |
|---|---|
| Braghetto I. | 3 |
| Gagner M. | 3 |
| Lee W. | 3 |
| Peterli R. | 3 |
| Deitel M. | 2 |
| Himpens J. | 2 |
| Langer F.B. | 2 |
| Melissas J. | 2 |
| Vidal J. | 2 |
Table VII
Authors with more than one senior- author article
| Senior author | Number of articles |
|---|---|
| Rosenthal R. | 5 |
| Basso N. | 4 |
| Gagner M. | 4 |
| Beglinger C. | 3 |
| Birkmeyer N. | 3 |
| Crosby R. | 3 |
| Prager G. | 3 |
| Schauer P. | 3 |
| Vidal J. | 3 |
| Karmali S. | 2 |
| Lacy A. | 2 |
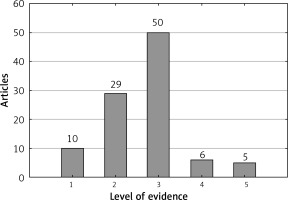
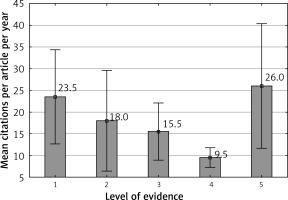
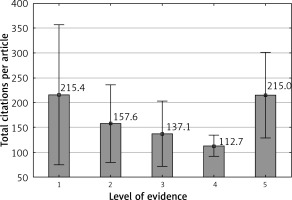
The most common level of evidence among the studies was III (50 studies), followed by II (29 studies) and I (10 studies) (Figure 5). The mean number of citations per year was highest among articles with a level of evidence of V (26 citations) (Figure 6). The mean number of citations per article was highest among articles with a level of evidence of I (215.4 citations) (Figure 7).
Most of the included studies focused on the short- and long-term clinical outcomes of SG (36 studies). Metabolic and hormonal changes were investigated by one-fourth (22) of the included articles. Overall, 18 of the included publications were reviews investigating the subject of SG in its entirety (Table VIII).
Discussion
The present report summarises the characteristics of the 100 most frequently cited publications focused on SG published up to date. These results may be useful in the process of designing further studies, and they provide a new understanding of the increased popularity of SG. Our study gives new insight into which articles, authors, countries, and journals have played a key role in understanding the advantages of SG and in promoting its use. Ahmad et al. [119] suggested the constant need to update bibliometric articles because of their limited life span. Conducting updates could help to identify changes in research trends [119]. We believe that further studies concentrating on bariatric surgery should also investigate the most popular procedures separately because of the vastness of the currently published literature devoted to bariatric surgery and the multiplicity of bariatric operations that are now performed.
Some of the most frequently cited studies were reviews that considered the subject of bariatric surgery in its entirety. Such reviews allow for a new understanding of the evolution of bariatric surgery as a field of study, which has undergone considerable change during recent years [14, 119]. Academic interest in bariatric surgery has been rapidly growing since the beginning of the 21st century, although surgical treatment of obesity has been performed for more than six decades [120, 121]. Additionally, bibliometric analyses have helped to outline which publications should be included in educational programs as mandatory reading material for surgeons, surgical trainees, and allied health professionals working in the field of bariatric surgery [121].
SG (parietal gastrectomy) was first introduced in 1988 as a restrictive component of biliopancreatic diversion with duodenal switch [121, 122]. Bariatric surgeons started to consider SG as an independent bariatric operation in the 21st century. Therefore, most research investigating SG is relatively recent [123]. Most of the studies included in our list were published after 2006. Our results indicate growing scientific interest in SG both in terms of the number of publications and the number of citations.
Although the receipt of external commercial funding, if clearly described, should not decrease the value of presented data, the vast majority of the most influential studies on SG were not funded commercially [124, 125].
During submission of a manuscript, it is critical to choose a journal with a scope matching the subject of the article [126]. Authors often desire to submit their work to prestigious journals. Unfortunately, there is no ideal parameter with which to measure the value of a journal. Currently, the most commonly used measure of a journal’s scientific influence is the impact factor, although this parameter has multiple imperfections [127]. Previously published bibliometric analyses of bariatric surgery, as well as most of the articles included in our list, were published in the most influential journals devoted to bariatric surgery: Surgery for Obesity and Related Diseases (established in 2005, the official journal of the American Society for Metabolic and Bariatric Surgery) and Obesity Surgery (established in 1999, the official journal of the International Federation for the Surgery of Obesity and Metabolic Disorders) [14, 109].
First authorship is often vigorously pursued by researchers as confirmation of a substantial contribution to the study and a crucial role during the research [128]. Senior authorship (last author) is usually associated with the role of supervisor or overseer of the study. According to Zbar and Frank, the senior author often has a minor or no contribution to the study; instead, he or she may have provided funding or is a laboratory head or mentor. The last author is often chosen based on seniority in the field [129]. We analysed the first and senior authorship among the included papers. Several authors repeatedly appeared in multiple publications included in our list, proving that they have played a substantial role in investigating SG and promoting advancements in bariatric surgery and recognition of SG.
Most of the included articles were published by authors from the United States. In accordance with the study by Angrisani et al. [1], the United States/Canada was also the region with the highest number of bariatric procedures. A recent analysis of bariatric practice in the United States demonstrated that laparoscopic SG has become the most common bariatric procedure performed in this country [130]. Moreover, it seems that academic institutions in the United States play a leading role in various fields of medical research other than bariatric surgery [131–133].
In 2003, The Journal of Bone & Joint Surgery introduced level of evidence ratings that have been extensively used in further publications and bibliometric analyses [15]. Most of the articles included in our list had a level of evidence of III. In contrast, most of the articles in the study by Ahmad et al. [119], who investigated bariatric surgery in general, had a level of evidence of IV. These results indicate the need to conduct further trials in bariatric surgery, preferably randomised clinical trials, because they are associated with the highest levels of evidence according to the current principles of evidence-based medicine [134].
Most of the literature included in our list comprised clinical experience/observational studies that presented outcomes of bariatric treatment in the clinical environment or metabolic and hormonal changes following the operation. Consistent with a previous publication by Carlson [10], we believe that further research should explain the mechanisms associated with SG, which would advance our current understanding of the physiological changes that occur after the procedure. Additionally, further improvement of techniques used in bariatric treatment should be encouraged [18, 19, 135].
The present study has several limitations. First, the number of citations provided by the Web of Science might not be extensive. In contrast to some previous articles, we decided not to verify the number of citations using Google Scholar. This is a database that does not standardise authors’ names, that includes every citation whether scholarly or not, and includes every version of an article, resulting in multiple duplicate entries and thus a duplicated number of citations [20]. Nevertheless, a similar search strategy conducted in a different database would probably result in a different outcome. Second, the number of citations is a limited measure of the relevance of a study. Finally, recently published studies that will significantly influence the development of bariatric surgery in the future might have been omitted.
Conclusions
Our study indicates an increase in medical researchers’ interest in the subject of SG since the year 2000 (especially since 2006). Crucial scientific papers investigating SG are usually observational clinical studies conducted in academic surgical centres. Influential scientific evidence seems to be authored mostly by scientists from the United States and published in bariatric surgery-oriented journals. Our study underlines the need to perform studies with a high level of evidence, preferably randomised clinical trials, to further analyse the outcomes of SG and basic science research to properly investigate the mechanism underlying metabolic changes after SG.