Introduction
The evolving obesity pandemic has become a burning issue worldwide. Nowadays, obesity is being considered a chronic disease with serious health consequences affecting the cardiovascular system (hypertension, ischaemic heart disease), metabolism of glucose, lipids and minerals (diabetes, hyperlipidaemia with subsequent atherosclerosis), the respiratory (sleep apnoea) and musculoskeletal system (arthrosis), as well as mental health (depression), resulting in shortened life expectancy and decreased quality of life. Also of note, obesity leads to impaired fertility and adversely affects pregnancy [1, 2]. The prevalence of obesity worldwide has nearly tripled since 1975. According to the World Health Organisation (WHO), 39% of adults (aged 18 years and more) were overweight in 2016, while 13% were obese [3].
Although a conservative approach is usually the first choice therapeutic option for obese patients, it remains associated with a high failure rate in the long term, due to rebound weight gain resulting in a vicious circle. As such, bariatric/metabolic (B/M) surgery represents the most effective sustainable treatment option for the time being [4–6]. Several bariatric procedures were described and proven effective, such as laparoscopic sleeve gastrectomy (LSG), Roux-en-Y gastric bypass (RYGB) and laparoscopic greater curvature plication (LGCP), which recently gained significant popularity in the Czech Republic. Other surgical methods were reported and utilised as well, but have not gained wider implementation. The surgical approach to obesity favours a laparoscopic approach due to well-documented advantages, including faster recovery, decreased postoperative pain, fewer surgical-site infections and diminished wound complications [7].
Effective B/M procedures may lead to changes in body composition. Desired fat loss is often accompanied by a decrease of muscle mass as well, which may be so significant that the patients are at risk of sarcopenia development [8]. Dual-energy X-ray absorptiometry (DEXA) offers the best reproducibility and accuracy to detect such changes [9, 10]. Some authors advocate the need for preventive programmes to overcome the problem of sarcopenia [11], such as the combination of aerobic and power exercises, which appears to be the most effective approach [12–14].
Aim
The aim of the study is to detect the occurrence of sarcopenia in patients 24 months after different B/M procedures by DEXA.
Material and methods
Consecutive patients scheduled for a B/M procedure due to obesity were enrolled in the prospective study approved by the Multicentre Ethics Committee of Vitkovice Hospital (ethical approval number: EK/234/2018), after obtaining their informed consent. Indications for surgery, based on BMI and comorbidities (7× arterial hypertension, 4× type 2 diabetes, 4× hyperlipidaemia), were approved by the multidisciplinary bariatric team, following the guidelines of the International Federation for the Surgery of Obesity (IFSO) [15], while respecting personal preference of the patients with regards to the type of procedure. All procedures were aimed to be performed laparoscopically, applying previously described standard techniques [16, 17].
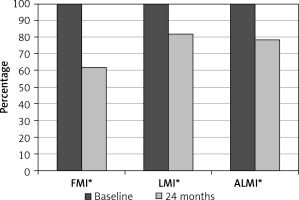
DEXA measurements were performed before and 24 months after the B/M procedure using the Hologic Discovery A densitometer (Mississauga, Ontario, Canada), calibrated according to the manufacturer’s recommendations. The precision error and coefficient of variation were established, which allowed the value of the minimal significant change to be calculated as described in previous studies [18–20]. Recorded measurements included fat mass index (FMI) – a measure of relative fat content, independent of fat free mass, estimated visceral adipose tissue (Est VAT) – estimated amount of visceral fat, lean mass index (LMI) – a measure of relative lean content, independent of fat mass, appendage lean mass index (ALMI) – a measure of relative lean mass in arm and legs, bone mineral content (BMC), Z score – for patients aged under 50 and T score – for those above 50 as measures of osteoporosis. Furthermore, every patient underwent anthropometric assessment which included a record of body weight, height, body mass index (BMI), excess body weight (EBW) calculated over BMI 25 kg/m2, waist and hip circumference, as well as biceps, triceps, supraspinatus and subscapular skinfold. Excess weight loss (EWL) was calculated as the percentage of weight loss to EBW. To assess physical activity after surgery, the International Physical Activity Questionnaire (IPAQ) was answered at 24 months [21].
Statistical analysis
Obtained data were tested for significant differences using licensed software (Statistica 12, Stat-Soft, CZ). The Wilcoxon signed rank test was used as the analysed data did not follow a normal distribution. Differences were considered statistically significant for a p-value under 0.05.
Results
Nineteen patients (4 males and 15 females, mean age: 46.3 ±8.9 years), after different B/M procedures (3× LGCP, 15× LSG, 1× RYGB), were enrolled in the study with no drop-off at follow-up at 24 months. Mean BMI dropped from 42.4 ±6.3 to 30.3 ±4.9 kg/m2 (p < 0.001) with mean EWL of 72 ±25%. Relevant anthropometric measurements decreased significantly as well (Table I). As for DEXA parameters (Figure 1, Table II), highly significant changes (p < 0.001) were observed for FMI, 19.5 ±4.7 vs. 12.1 ±3.7 kg/m2, Est VAT, 235.8 ±70.0 vs. 126.5 ±50.4 cm2, LMI 22.1 ±2.4 vs. 18.1 ±2.3 kg/m2, ALMI 9.7 ±1.3 vs. 7.7 ±1.1 kg/m2, BMC 1.22 ±0.1 vs. 1.12 ±0.1 kg, Z score – for age under 50 (2.32 vs. 0.96) and T score – for age above 50 (0.58 vs. –0.58). The results confirm significant changes in body composition at 24 months after B/M surgery, where desired fat loss is clearly associated with a significant decrease of skeletal muscle mass and bone mineral mass as well. Also of note, a low level of physical activity was recorded within the patient group, based on the results of IPAQ at 24 months after surgery (Table III).
Table I
Anthropometric data at baseline and after 24 months
Table II
Median FMI, LMI and ALMI at baseline and after 24 months – overall and split by the procedure
| B/M procedure | N | FMI [kg/m2] Baseline | FMI [kg/m2] After 24 months | LMI [kg/m2] Baseline | LMI [kg/m2] After 24 months | ALMI [kg/m2] Baseline | ALMI [kg/m2] After 24 months |
|---|---|---|---|---|---|---|---|
| Overall | 19 | 19.1 | 12.3* | 21.3 | 18.1* | 9.39 | 7.45* |
| LSG | 15 | 19.5 | 11.5* | 21.7 | 17.6* | 9.58 | 7.45* |
| LGCP | 3 | 19.1 | 14.2 | 19.8 | 18.1 | 8.57 | 7.65 |
| RYGB** | 1 | 15.3 | 9.2 | 20.2 | 15.8 | 8.89 | 6.57 |
Discussion
B/M surgery represents the most effective therapeutic tool for morbid obesity and a promising approach towards obesity-related comorbidities, because, unlike conservative treatment, it assures significant, quick and relatively sustainable weight loss [19, 22–24]. Although this effect is predominantly based on the desirable fat mass reduction, it may also be associated with a decrease of other body components, such as muscles and bones [10, 19, 20]. Both obesity and sarcopenia increase health-related risks, especially when they co-exist. Therefore, the European Society for Clinical Nutrition and Metabolism (ESPEN) and the European Association for the Study of Obesity (EASO) call on researchers and clinicians to study and challenge sarcopenic obesity [11].
Although DEXA represents an excellent tool to detect changes in body composition [9, 10], it is used relatively infrequently to assess series of patients after mixed B/M procedures with respect to sarcopenia. Taking into account the advantages of this methodology, allowing for clear analysis of the weight loss structure, it should be used more systematically to reveal the true effects of B/M surgery.
The weight and fat loss effect observed in our study was excellent. BMI dropped from class III obesity to class I. Observed Est VAT (representing the fat around internal organs such as heart, lung, liver and others) decreased from the “high risk“ (above 160 cm2) to “increased risk“ category (above 100 cm2) for obesity complications [25, 26]. As for the BMC, values under the normal range were recorded before surgery, with a further decrease at 24 months after the B/M procedure. Although Z and T scores dropped as well, none of the patients qualified for risk of osteopenia or osteoporosis.
With regards to possible sarcopenia, LMI and ALMI were analysed in our study. While LMI represents the body mass without fat and without bones (includes internal organs), ALMI describes skeletal muscle mass of the extremities (independently of internal organs) – as a substantial number of study population underwent LSG, both LMI and ALMI were considered fundamental for possible sarcopenia detection. Baumgartner et al. described cut-off values for sarcopenia for men and women as 7.26 and 5.45 kg/m2 respectively [27]. None of our patients crossed over these values, but some were very close to the sarcopenia status at 24 months after surgery. This is an alarming finding that requires further attention of multidisciplinary teams dealing with patients subjected to B/M surgery.
Based on the IPAQ evaluation, a negligible impact of physical activity on weight loss in our study population was detected. At the same time, lack of physical activity might represent a contributing factor towards observed skeletal muscle mass reduction. To decrease the risk of muscle mass loss, power exercise in combination with aerobic exercise is recommended in some studies [12–14]. Whether this logical assumption translates into clinical practice remains unclear, so further studies are needed with proper design. Based on our findings, a structured rehabilitation programme controlled by physiotherapist is planned to be included in our standard postoperative care after B/M procedures for 24–48 months to assess their impact on sarcopenia development and to decrease the risk of postoperative weight gain.
Despite the statistically significant results, there are some limitations that should be taken into consideration. The sample size of the study population is relatively low, while the spectrum of B/M procedures is relatively wide. As such, our results should be considered as pilot data, drawing attention to the problem of muscle mass loss after B/M procedures in general, which seems to be associated with fat mass loss at 24 months after surgery.
DEXA, which was implemented for assessment of body composition changes after B/M surgery, with special focus on sarcopenia detection, was found to be a reliable, objective tool with a high acceptability rate among the patients (no drop-off from the study population on follow-up at 24 months). As a result, this methodology might be re-applied by other researchers, bearing in mind the financial burden.
Conclusions
B/M procedures lead to significant changes in body composition at 24 months after surgery. DEXA detects these changes effectively. Although desirable loss of fat mass is the most obvious, reduction of skeletal muscle mass and bone mineral mass is significant as well. As such, patients after B/M surgery can be at risk of sarcopenia. A low level of physical activity, which seems to be characteristic for this patient group, may also play a negative role. Therefore, preventive measures to avoid sarcopenia in patients after B/M procedures might be justified.