BACKGROUND
Dignity is repeatedly mentioned in reference to end of life decisions for patients with terminal illness, such as advanced cancer. Public and professional views strongly equate dignity among the dying with their abilities to make decisions about medical and personal treatment consistent with their values (Johnson, 1998; Mairis, 1994). This has encouraged the concept of dignity-conserving care, which largely relies on effective patient-provider communication that can mutually inform goals of care (Chochinov, 2007). However, the actual meaning of dignity has been repeatedly recognized as a relative unknown. Criticisms include the lack of agreed upon or weak definitions (Östlund et al., 2012), undermining how to define targets for dignity-conserving care.
This ambiguity is recognized, as Chochinov (2007) states that patients “likely ascribe their own unique meaning” to define dignity. The meanings patients assign to their personal sense of dignity are determined by cognitive processes that can influence psychological adjustment (Hagger et al., 2017). Cognitive processes refer to mental actions that inform our understanding of circumstances by integrating thoughts, experiences, and perceptions with prior knowledge (Broadbent, 2019). Cognitive processes are relevant to a major category of symptoms that patients with advanced cancer ascribe to their dignity-related distress (Chochinov et al., 2002). Patients reference cognitive changes to their ability to think clearly (i.e., cognitive complaints) as well as uncertainty regarding treatment decisions and future illness progression. Cognitive complaints reflect self-assessment of one’s ability to access knowledge (Mitchell, 2008) and lacking knowledge leads to the experience of uncertainty (Anderson et al., 2019). In this way, problems stemming from cognitive changes and uncertainty reflect specific cognitive processes that can interfere with patients’ abilities to understand their illness and treatment, necessary for engaging in the decisions of care that maintain their sense of dignity.
Understanding the meaning of dignity to patients may therefore require exploring relationships between these underlying cognitive processes that determine such meaning to them in the first place. Structural equational modeling is an exploratory approach to understand such relationships based on a given model. A model of dignity developed from interviews with patients with advanced cancer (Chochinov et al., 2002) informed the development of the Patient Dignity Inventory (Chochinov et al., 2008), which includes items related to cognitive complaints and uncertainty given their importance to dignity-related distress. Although cognitive complaints and uncertainty in illness have their own significant bodies of literature highlighting their importance to patients with cancer (Etkind et al., 2017; Janelsins et al., 2017) and associations with anxiety and depression (Wefel et al., 2015), their role specific to problems with perceived dignity has been overlooked. From this perspective, we can learn from other bodies of literature on uncertainty in illness and cancer-related cognitive changes to explore pathways to psychological adjustment as a model of targets for providing dignity-conserving care.
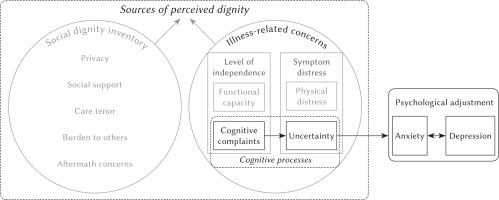
Uncertainty has been described as a neutral cognitive state (McCormick, 2002) arising from the threat of illness to the preexisting self that forces cognitive evaluations to restructure the meaning of life events (Mishel, 1990). From this perspective, uncertainty can be managed if the person feels they have the cognitive capacity to restructure events but exacerbated in the presence of perceived cognitive decline, as is the case with cognitive complaints. Consistent with this idea, we hypothesized that patients who reported dignity-related distress due to cognitive complaints would reflect difficulties with such processes as cognitive restructuring and meaning-making to causally influence levels of dignity-related distress related to uncertainty. Cognitive complaints can therefore act as an important antecedent to uncertainty. Meanwhile the outcomes of uncertainty in illness, especially anxiety and depression, have been identified on multiple occasions (Gramling et al., 2018; Kurita et al., 2013). Thus, the pathway of dignity-related distress from cognitive complaints to uncertainty should causally predict psychological outcomes consistent with this literature on uncertainty in illness. Specifically, we hypothesized a causal positive relationship between uncertainty and levels of depression through a mediating effect of levels of anxiety, which have been shown to be a risk factor for depression (Massie, 2004). This informed the proposed model, as can be seen in Figure 1. The objective of this study was to propose and test a model (Figure 1) as a first step toward promoting a novel path of investigation that defines targets for dignity-conserving care by considering underlying cognitive complaints as antecedents to uncertainty that impact psychological adjustment of patients with advanced cancer.
Figure 1
Conceptual model of the associations between cognitive processes underlying perceived dignity as determinants of psychological adjustment
Note. Sources of perceived dignity adapted from Chochinov et al., 2002.
PARTICIPANTS AND PROCEDURE
PARTICIPANTS
Data from 257 patients recruited between January 2016 and June 2017 at a comprehensive cancer center were used for the present analysis. The study protocol was approved by the Institutional Ethics Committee in accordance with the Declaration of Helsinki (approval code: PR216/15), and all patients provided verbal and written informed consent. Patients were eligible for the study if they had: (a) a diagnosis of advanced cancer (the presence of distant metastasis and/or an estimated life expectancy ≤ 12 months), (b) understanding of their cancer diagnosis and its potential progression and (c) physical and emotional stability according to the treating physician. Patients were excluded if they had: cognitive failure defined as > 5 fails on the Pfeiffer Short Portable Mental Status Questionnaire – Spanish version or an active diagnosis and treatment for psychiatric disorder in their medical record.
MEASURES
Eligible patients who agreed to participate had sociodemographic data recorded and were administered the Spanish version of a series of measures. Data related to other variables, namely measuring the wish to hasten death, have been described in previous studies (Bellido-Pérez et al., 2018; Crespo et al., 2020; Monforte-Royo et al., 2018; Pergolizzi et al., 2021). For the purposes of the current study, only a subset of the data from the following measures was used.
The Patient Dignity Inventory (PDI) is an instrument by which we measured the perceived impact of cognitive complaints and uncertainty specific to perceived dignity (Chochinov et al., 2008; Rullán et al., 2015). Patients indicated the extent to which they experienced 25 unique items as a problem on a scale of 1 (no problem) to 5 (overwhelming problem). To specifically understand uncertainty and cognitive complaints only item number seven, “feeling uncertain about illness and treatment”, and item number nine, “not being able to think clearly”, respectively, were used in our current analysis. Use of a single item is consistent with various measures of psychological constructs (Klepsch et al., 2017; Konrath et al., 2018; Lucas & Donnellan, 2012; Reysen et al., 2013) and has been used in structural question modeling (Oh, 2017).
The Hospital Anxiety and Depression Scale. Anxiety and depression was assessed using the Hospital Anxiety and Depression Scale (HADS), providing separate scores for anxiety (HADS-A) and depression (HADS-D), with higher scores indicating higher levels of anxiety or depression (Herrero et al., 2003). Total scores for HADS-A and HADS-D were included in analyses.
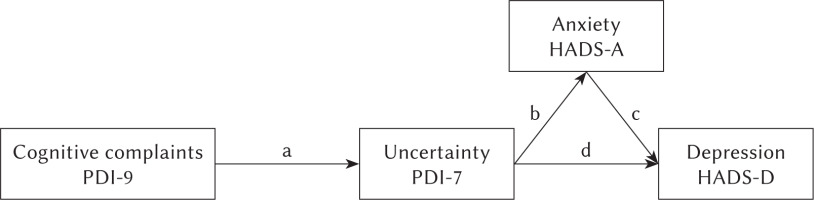
STATISTICAL ANALYSIS
Descriptive statistics (percentages and frequencies for categorical variables) were used to describe the demographic and clinical characteristics of the sample. Structural equation modeling was conducted to indicate the strength of influence among variables of interest using EQS 6.4. Among the benefits of structural equation modeling is that it allows for statistical testing of both direct and indirect paths simultaneously (Westland, 2015). Accordingly, a path analysis model was developed, as shown in Figure 2. To assess direct and indirect relationships, the path analysis assessed PDI-9 (cognitive complaints) as an antecedent of PDI-7 (uncertainty), HADS-A (anxiety) and HADS-D (depression) as direct outcomes from uncertainty, and where the effect of uncertainty on HADS-D is mediated through HADS-A (b*c in Figure 2). Additionally, the model assessed the indirect effect of cognitive complaints on HADS-A (a*b) and on HADS-D (a*b*c; a*d in Figure 2).
Figure 2
Path analysis model
Note. Letters on arrows are required to interpret results in Table 2. PDI-9 – Patient Dignity Inventory item 9 “not being able to think clearly”; PDI-7 – Patient Dignity Inventory item 7 “feeling uncertain about illness and treatment”; HADS – Hospital Anxiety Depression Scale.
RESULTS
PARTICIPANT CHARACTERISTICS
The demographic and clinical characteristics of the sample are presented in Table 1. The average age of the sample was 63.11 years, ranging from 29 to 87 years. A larger proportion of patients were male, had primary school education, were on active treatment and had a diagnosis of advanced cancer for one year or longer. The most common neoplasms were digestive, lung/intrathoracic, or genitourinary.
Table 1
Demographic and clinical characteristics of patients
MODEL HYPOTHESIS
The model was estimated by applying the robust maximum likelihood method to the asymptotic variance-covariance matrix. To assess data fitness, the following indices were calculated: the Satorra-Bentler χ2 was 14.38, with 2 degrees of freedom, and a p-value of < .001; the root mean square error of approximation was .155 and its 95% CI was .087 to .235; the comparative fit index was .912; and the Bentler-Bonett normed fit index was .902. Taking into account the values of all these global indicators, it can be said that the overall fit of the model was acceptable.
SIGNIFICANT DIRECT AND INDIRECT EFFECTS
Significant effects in the model with decomposition of the direct and indirect effects are presented in Table 2. All variables showed significant positive direct and indirect effects, confirming hypothesized relationships proposed by the model. It can be said that: (1) PDI-9 (cognitive complaints) is an antecedent to PDI-7 (un-certainty), (2) PDI-7 directly impacts both HADS-A (anxiety) and HADS-D (depression), (3) PDI-7 indirectly impacts HADS-D through HADS-A, and (4) PDI-9 indirectly impacts HADS-D through PDI-7. Factor loadings were highest for the direct effect of PDI-7 on HADS-A, followed the direct effects on HADS-D by HADS-A and PDI-7, respectively. The model had moderate explanatory power, R2 = .31, for depression.
Table 2
Decomposition of the parameters of the model as a standardized parameter (t-value)
DISCUSSION
In the context of perceived dignity in advanced cancer, the current study demonstrated a direct pathway between underlying patient reported problems with cognitive changes to uncertainty. Additionally, the item related to uncertainty had both direct and indirect effects on depression, largely mediated by a direct effect on anxiety. We acknowledge that the use of the single items from the Patient Dignity Inventory “not being able to think clearly” and “feeling uncertain about illness and treatment” broadly represent complaints related to problems with cognitive changes and uncertainty that impact perceived dignity, respectively. These items cannot define the levels and extent of uncertainty or cognitive changes. Rather we aimed to use these items as proxies for these important symptoms to drive theory and priorities for further research for understanding targets for dignity conserving care.
The model highlights the importance of cognitive processes in the larger scheme of dignity-related distress. Little is known about how uncertainty is derived, with antecedents rarely described (Jabloo et al., 2017; Mishel & Braden, 1988), nor is it explored in the context of its role in perceived dignity. The direct path from cognitive changes to uncertainty is therefore relevant to understanding sources of uncertainty in general and the interrelationships of illness-related concerns that patients with advanced cancer must manage to maintain perceived dignity. Consistent with the model of dignity in advanced cancer (Chochinov et al., 2002), illness-related concerns are represented by loss of independence and symptom distress, which are buffered by a dignity conserving repertoire that influences perceived dignity. Loss of independence includes perceived cognitive changes, highlighting the importance of cognitive abilities to patient autonomy. Autonomy is largely defined by patients’ ability to make decisions for themselves (Houska & Loučka, 2019). Decision-making is inherently a cognitive process. The range of decisions for any patient with advanced cancer are extremely difficult and diverse, ranging from choosing between treatment options to advance care planning to place of death. These decisions are often expected earlier rather than near death considering that cognitive failure is among the most common complications seen in patients as cancer progresses (Hosie et al., 2013). Recognizing cognitive changes is also common in patients with cancer (Janelsins et al., 2017) and leads to uncertainty, which, as shown here, has implications for decision-making in advanced cancer. Clearly decisions must not only be made early but also be accompanied with sufficient support to compensate for uncertainties in order to maintain perceived dignity while also ensuring that last wishes are met.
Cognitive processes also fundamentally determine patients’ perceptions and representations of their illness. This includes patients’ perceptions of their self as well as treatment by others that are crucial to deriving a sense of dignity and respect (Chochinov, 2007). Recognizing cognitive changes with the Patient Dignity Inventory shows that patients are aware of their inability to think clearly, which can certainly threaten their self-perception. Even more so, however, advanced cancer is not a static process but changes progressively so that patients may need more information with the appearance of more symptoms. If the patient feels they have trouble thinking clearly as an additional symptomatic issue, they may need that information tailored to their ability to pay attention and remember later. This is crucial to dignity-conserving care as patients do not always receive information in a way that they can understand or are given opportunities to ask questions should something need to be clarified (Chochinov, 2007). This is particularly important for patients with advanced illness to form correct representations of their illness, particularly in terms of limited prognosis that many fail to recognize and is related to exponentially greater rates of depression (Chochinov et al., 2000). This suggests that changes to cognitive processes can impact perceived dignity from multiple sources, not limited to a perception of self compared to what they previously could understand, whether others respect these changes to convey information in a way they can understand, which together influences whether they now can understand and adjust to their illness.
The model also has value for indirect pathways that develop an understanding of contributors to depression. Depression has long been recognized to have a moderate prevalence in patients with advanced illness (Salvo et al., 2012). If not appropriately addressed, patients can lose meaning in life and experience a wish to hasten their death (Guerrero-Torrelles et al., 2017). The indirect relationship from uncertainty through anxiety showed the highest factor loading in our model and explained 30.7% of depression scores, consistent with multiple determinants of depression in advanced cancer. In other words, dignity-related distress from uncertainty and anxiety are among several factors that can influence levels of depression (Robinson et al., 2017). These pathways highlight that addressing depression in advanced cancer relies on recognition of multiple sources of distress, including anxiety originating from uncertainty.
As mentioned above, items used from the Patient Dignity Inventory are only surrogate markers for the complex nature of cognitive changes and uncertainty underlying dignity-related distress. Nevertheless, the model tested provides preliminary confirmation for further research on the cognitive processes that have specific roles in how patients can define and experience dignity, such as when accessing memories using dignity therapy. The data used are only representative of a single center, and further studies should explore the importance of these variables to patients with advanced cancer in other inpatient, outpatient, and community settings.
CLINICAL IMPLICATIONS
This model has implications for psychosocial care at the end of life. First, the impact of specific aspects underlying dignity, especially cognitive processes that are fundamental to decisions for care, can be identified using the Patient Dignity Inventory. Second, our model shows that understanding the relationships between these processes can capture clinical targets for dignity-conserving care. This is important because cognitive processes are modifiable. Evidence-based interventions already exist to support rehabilitation for cognitive complaints (Janelsins et al., 2014) and ameliorate uncertainty (Etkind & Koffman, 2016). These interventions show benefits for anxiety and depression suggesting additional importance specific to psychological outcomes. This should encourage research to clarify precise changes to cognitive processes that impact perceived dignity for patients with advanced cancer, which has implications for research on cancer and treatment related cognitive changes. In general, this field is relatively understudied, with the majority of work in breast cancer cohorts (Ahles et al., 2012). As a result, there have been multiple calls for research of cognitive changes in other populations with cancer (Ahles et al., 2012; Pergolizzi & Crespo, 2020; Vardy & Dhillon, 2018). This suggests that psychosocial providers can promote dignity-conserving care in advanced cancer through support or rehabilitation for cognitive complaints as a promising target not only to maintain perceived dignity, but also as a way to prevent downstream negative effects.
LIMITATIONS AND CONCLUSIONS
As mentioned above, the items used from the Patient Dignity Inventory are only surrogate markers for the complex nature of cognitive changes and uncertainty. Nevertheless, the model tested provides preliminary confirmation for further research on the relationships between cognitive function, uncertainty in illness, and negative psychological outcomes. The data used are only representative of a single center, and further studies should explore the importance of these variables to patients with advanced cancer in other inpatient, out-patient, and community settings. Uncertainty is ubiquitous in life and may be exacerbated by a diagnosis such as advanced cancer. Understanding its antecedents and outcomes can inform complex interventions to holistically support patients. Adapting non-pharmacological interventions for cancer and treatment-related cognitive changes is an appealing option.


