Introduction
Invasive mechanical ventilation (IMV) improves survival for respiratory distress syndrome (RDS) in premature infants, but is associated with various complications including ventilator-associated lung injury, infection, and bronchopulmonary dysplasia (BPD) [1]. American Academy of Pediatrics and European Consensus Guidelines recommend non-invasive ventilation (NIV) in the treatment of RDS [2, 3]. Nasal continuous positive airway pressure (NCPAP) is recommended as the optimal first mode of respiratory support; however, the failure rate of NCPAP and the need for intubation and IMV remain high, especially in extremely preterm infants [4, 5]. Noninvasive intermittent positive airway pressure ventilation (NIPPV) superimposes an intermittent peak pressure on CPAP. NIPPV is gaining wider acceptance as a second-line NIV after failure of NCPAP [6]. The recent meta-analyses indicated that early NIPPV did appear to be superior to NCPAP for decreasing the need for intubation among preterm infants with RDS [7]. However, Kirpalani et al. failed to demonstrate that NIPPV improved the rate of survival without BPD at 36 weeks of post-menstrual age, as compared with NCPAP in a large multicenter trial [8]. Nasal high-frequency oscillatory ventilation (NHFOV) is an emerging NIV mode that applies an oscillatory pressure wave form on CPAP [9]. Retrospective studies have shown that NHFOV might be a promising NIV mode to decrease intubation in preterm infants with RDS [10, 11]. Four small randomized trials have compared NHFOV with NCPAP for the initial management of infants with RDS, but the conclusions were not consistent [12–15]. Up to now, there has been only limited clinical evidence of superiority of NIPPV or NHFOV over NCPAP for the management of infants with RDS.
We conducted this multicenter retrospective study to compare the effectiveness of NCPAP/NIPPV/NHFOV used as initial treatment for infants with RDS. A propensity score analysis was used to balance patient characteristics and reduce bias when performing a retrospective comparison of patients treated with these regimens.
Material and methods
Study design
This multicenter retrospective cohort study was performed using data from four tertiary neonatal intensive care units (NICUs) in China from January 2016 to December 2018. 512 preterm infants (gestational age of 26 weeks 0 day to 33 weeks 6 days) with RDS who received NHFOV or NIPPV or NCPAP after birth were analyzed. The exclusion criteria were: 1) intubated for resuscitation or for other reasons; 2) crossover among the three NIV strategies; 3) major congenital malformations or known complex congenital heart disease. Approval for the study and sharing data with the coordinating institution was granted by the Children’s Hospital of Chongqing Medical University and registered at www.chictr.org.cn, No.: ChiCTR1900027079 (registration date, October 30, 2019).
Standard for diagnosis of RDS
The diagnosis of RDS was based on clinical manifestations and chest X-ray findings. The clinical signs and symptoms of RDS were respiratory distress, tachypnea, nasal flaring, groan, and cyanosis appearing within the first 24 h of life. The typical X-ray picture of RDS showed a grain shadow, air bronchogram or white lung.
Noninvasive ventilation strategies
The criteria for initiation of NIV: 1) Early prophylactic use in extremely premature infants with spontaneous breathing in the delivery room; 2) all babies at risk of RDS, such as those < 30 weeks’ gestation who do not need intubation for stabilization; 3) when FiO2 > 0.30 by nasal catheter, mask, or hood for oxygen, PaO2 < 50 mm Hg or TcSO2 < 0.90; 4) apnea of prematurity.
In the delivery room, all preterm infants were supported with NCPAP (PEEP: 6–8 cm H2O). Infants were transferred to the NICU within 1 h after birth, and then began to receive three different NIV strategies (NCPAP: n = 197; NIPPV: n = 163, NHFOV: n = 152) as initial treatment for RDS.
The NCPAP was provided by the continuous positive airway pressure system (Carefusion, USA). The respiratory parameter setting was a CPAP of 6–8 cm H2O.
The NIPPV was delivered by a time-cycled, pressure-limited and continuous-flow neonatal ventilator (Babylog 8000, Drager, Germany) in a non-synchronized mode. The respiratory parameter settings were: frequency of 10–30 breaths/min, peak inspiratory pressure (PIP) of 15–25 cm H2O, and positive end expiratory pressure (PEEP) of 4–6 cm H2O.
The NHFOV was administered using two different high-frequency ventilators via binasal prongs. Two sites used the Babylog 8000 (Drager, Germany), the other two sites used the SLE 5000 (UK) to deliver NHFOV. The respiratory parameter settings were: mean airway pressure of 6–10 H2O, frequency of 10 Hz, inspiratory time of 50% (1 : 1), and oscillation amplitude of 20–35 cm H2O.
In all three modes, the lowest FiO2 was adjusted in order to maintain a SaO2 of 90-94%.
Surfactant administration
The indication of surfactant administration was similar in the four NICUs. Surfactant (Curosurf; 200 mg/kg) was administered in the case of increased FiO2 greater than 0.40 to a target SpO2 of 90–94%, by the INSURE (intubation, surfactant, extubation) technique [2].
Caffeine treatment
Caffeine (Caffeine Citrate Injection, Chiesi Pharmaceuticals, Parma, Italy) was administered when infants presented with any apnea. The initial loading dose was 20 mg/kg, and the maintenance dose was 5 mg/kg/day.
Outcomes
The primary outcome was the need for intubation and IMV within the first 7 days of life in preterm infants after birth. The criteria for intubation and mechanical ventilation were as follows [16, 17]: (1) severe respiratory acidosis (PaCO2 > 65 mm Hg with pH < 7.20); (2) severe apnea and bradycardia (defined as recurrent apnea with > 3 episodes/h associated with heart rate < 100/min, a single episode of apnea that requires mask ventilation); (3) hypoxia (FiO2 > 0.5 with PaO2 < 50 mm Hg) for at least 2 h; (4) other specific circumstances based on the medical team’s discretion at each site.
Secondary outcomes included days of hospitalization, predischarge mortality, rate of retinopathy of prematurity (ROP) > stage II, bronchopulmonary dysplasia (BPD) [18], air leaks, intraventricular hemorrhage (IVH) ≥ grade 3, and necrotizing enterocolitis (NEC) ≥ stage II. IVH classification was according to Papile et al. [19] and for NEC, Bell staging was used [20].
Sample size calculation
According to a retrospective study [21], the risk of failure while receiving initial NCPAP without INSURE in infants born between 25 and 32 weeks was 25%. We assumed a reduction of 15% in in the primary outcome with NHFOV/NIPPV as compared with NCPAP. Considering an α error of 0.05 and a power of 80%, 96 neonates would be needed at least in each group.
Statistical analysis
Logistic regression was used for propensity score calculation from baseline patient characteristics including gestational age, gender, birth weight, multiple pregnancy, cesarean delivery, Apgar score at 5 min, corticosteroid, premature rupture of membrane, caffeine treatment, surfactant treatment and diabetes. Propensity score analysis with 1 : 1 matching was performed with the nearest neighbor matching method using calipers of width equal to 0.1 of the standard deviation of the logit of the propensity score. Multiple imputations were performed because the exclusion of patients with at least 1 missing variable may cause bias. If continuous data were normally distributed, differences among groups defined by exposure to different ventilations were examined using Student’s t test. If not, the nonparametric H test was used for comparison of the three groups. The χ2 test and Fisher’s exact test were used to analyze categorical variables. Statistical significance was considered if the p-value was < 0.05. All statistical data analyses were performed using SPSS statistical software (version 22.0).
Results
Five hundred and twelve preterm infants with RDS who received NIV treatment were included. They were divided into three groups based on the initial NIV mode (197 in NCPAP group, 163 in NIPPV group and 152 in NHFOV group). Baseline patient characteristics before propensity score matching are described in Table I. Several differences were found. In order to avoid differences and deviations between retrospective study groups, we used propensity score matching. Propensity score matching identified 126 infants in each cohort (NHFOV vs NIPPV), 96 infants in each cohort (NHFOV vs. NCPAP), and 134 infants in each cohort (NIPPV vs. NCPAP) respectively. The perinatal characteristics of the studied groups are reported in Table II and no significant differences (p > 0.05 respectively) were found between the three studied groups. The baseline patient characteristics after propensity score matching are listed in Table II.
Table I
Baseline patient characteristics before propensity score matching
[i] NHFOV – noninvasive high-frequency oscillatory ventilation, NIPPV – nasal intermittent positive-pressure ventilation, NCPAP – nasal continuous positive airway pressure, PS – pulmonary surfactant, GA – gestational age week, BW – birth weight. P1 – p-value of NHFOV vs. NIPPV, P2 – p-value of NHFOV vs. NCPAP, P3 – p-value of NIPPV vs. NCPAP.
Table II
Baseline patient characteristics after propensity score matching
[i] NHFOV – noninvasive high-frequency oscillatory ventilation, NIPPV – nasal intermittent positive-pressure ventilation, NCPAP – nasal continuous positive airway pressure, PS – pulmonary surfactant, GA – gestational age week, BW – birth weight. P1 – p-value of NHFOV vs. NIPPV, P2 – p-value of NHFOV vs. NCPAP, P3 – p-value of NIPPV vs. NCPAP.
The need for IMV was significantly lower in the NHFOV than NCPAP and NIPPV groups (13/126 vs. 27/126, p = 0.027; 9/96 vs. 20/96, p = 0.016), while no difference was observed between NIPPV and NCPAP groups (25/134 vs. 25/134, p = 1.00) (Table III). However, the number of days of hospitalization in NIPPV was significantly lower than that in the NCPAP group (24.8 ±14.6 vs. 33.2 ±20.2 days, p = 0.002) (Table III). There was no significant difference among the three groups in any secondary outcomes (p > 0.05 respectively) (Table III).
Table III
Primary outcome and secondary outcome of 3 cohorts
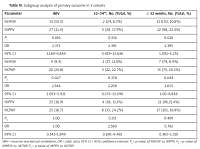
In subgroup analyses, the need for IMV did not show significant differences between the NHFOV versus NCPAP cohort and NHFOV versus NIPPV cohort at 32 to 34 + 6 weeks’ gestational age (2 : 17 vs. 5 : 22; 95% CI: 0.372–13.090; p = 0.376 and 2 : 24 vs. 5:28; 95% CI: 0.419–13.636; p = 0.316). However, in the preterm infants at ≤ 32 weeks’ gestational age, the need for IMV was significantly lower in the NHFOV group than in the NCPAP and NIPPV groups (7 : 79 vs. 15 : 74; 95% CI: 1.00–6.836; p = 0.044 and 11 : 102 vs. 22 : 98; 95% CI: 1.092–5.251; p = 0.026), and there was no difference between NIPPV and NCPAP in the subgroup (Table IV).
Table IV
Subgroup analysis of primary outcome in 3 cohorts
Discussion
In this retrospective study, we performed propensity score matching to balance baseline patient characteristics, and demonstrated that NHFOV, applied as the initial NIV for RDS treatment of preterm infants, had a significantly lower failure rate than NIPPV and NCPAP after matching. However, we found no significant difference between NIPPV and NCPAP in the risk of failure. In addition, there was no difference between the three groups in any of the secondary outcomes.
We have previously reported that NHFOV significantly decreased the need for IMV compared with NCPAP in preterm infants with moderate-severe RDS (n = 81, GA 28–34 weeks) [12]. Recently, Iranpour et al. also found that NHFOV significantly reduced the duration of non-invasive respiratory support and decreased the need for intubation compared with NCPAP in infants with RDS (n = 68, GA 30–36 weeks) [13]. Moreover, a recent meta-analysis of randomized controlled trials concluded that NHFOV significantly removes carbon dioxide and reduces the risk of intubation compared with NCPAP [22]. The results of this retrospective study are consistent and offer additional evidence to support previous observations that showed the benefit of NHFOV over NCPAP in preterm infants with RDS, with a significant reduction in the need for IMV. Conversely, the trial of Mukerji included 39 infants with a birth weight of less than 1250 γ and randomly assigned to NHFOV or biphasic positive airway pressure if they failed on NCPAP and demonstrated that failure of NHFOV was lower with biphasic positive airway pressure (37.5% vs. 65.2%, p = 0.09), although not statistically significant [14]. Considering the small sample size of the study, their results seemed inconclusive. The study by Malakian et al. [15] randomized preterm infants (GA 28–34 weeks; n = 124) to NHFOV versus NCPAP and reported that NHFOV did not reduce the need for invasive mechanical ventilation during the first 72 h, but the duration of noninvasive ventilation in the NHFOV group was significantly shorter. The difference between their outcomes and our findings may be due to the discrepancy in the different time-points of evaluation and analyses.
Contrary to our hypothesis, this study did not demonstrate a significant decrease in the primary outcome of the need for intubation and IMV in preterm infants receiving NIPPV for NIV support compared to those receiving NCPAP. Several randomized trials have compared NIPPV with NCPAP for the initial management of infants with RDS, showed discrepancies in obtained results [23–27]. Kugelman et al., Sai Sunil Kishore et al., and Shi et al. reported that early initiation of NIPPV may lead to a reduction in the need for intubation and IMV compared with NCPAP [23–25], while Chen et al. and Meneses et al. found that NIPPV had no advantage in reducing intubation compared with NCPAP [26, 27]. Recently, Bourque et al. performed a retrospective cohort study using NIPPV randomized control trial data of Kirpalani et al. They identified that failure rates were similar for NIPPV vs. NCPAP [28]. Our study also demonstrated no significant differences between NIPPV and NCPAP; however, the number of days of hospitalization in NIPPV was significantly lower than that in the NCPAP group. We speculated that the main reason for the inconsistency among the aforementioned studies might be a wide range of set peak pressures (10–25 cm H2O pressure), ventilator rates (10–60/min), variable inflation times (0.3–0.5 s), and synchronized or no synchronized breaths for use in NIPPV [29].
In subgroup analyses, we found that NHFOV significantly decreased the need for IMV compared with NCPAP and NIPPV in very preterm infants (gestational age < 32 weeks). Rüegger et al. [30] evaluated the effectiveness of NHFOV versus NCPAP for oxygen desaturation and bradycardia in very preterm infants. They also reported that NHFOV compared with NCPAP significantly reduced the frequency of desaturation and bradycardia. With a collapsing chest wall and poor diaphragmatic strength, smaller infants are more vulnerable to fail NCPAP due to closure of the glottis during the inspiratory phase. NHFOV does not induce glottal constrictor muscle activity, in contrast to NCPAP, obtaining a sufficient gas exchange and reducing the risk of apneas [30]. This may be an additional advantage of NHFOV relative to NCPAP in smaller preterm infants.
In the present study, we found no difference in any of the respiratory secondary outcomes among different NIV strategies, especially in the rate of BPD. Nevertheless, the following key points should be acknowledged: (1) The sample size was calculated based on the need for intubation rather than the rate of BPD, so it is possible that the sample size is too small to detect the difference of BPD among the different NIV. (2) The etiology of BPD is complex. Avoiding invasive ventilation does not mean reducing the incidence of BPD. Furthermore, the absence of differences in any other adverse events (i.e. IVH, NEC, pneumothorax, etc.) among different NIV strategies can offer additional evidence to support the similar safety of different NIV modes. According to the study of Handoka et al. [31], the failure of synchronous noninvasive intermittent positive pressure ventilation (SNIPPV) is related to the mean airway pressure (MAP). We did not compare the precise parameter of each group. This is the limitation of our study.
The limitations of the study are: 1) it was retrospective, and the retrospective nature of the study might inherently lead to the risk of missing data; 2) it was not randomized, and propensity score analysis could only balance known and selected variables; 3) there might remain a risk of bias in the choice of the mode of NIV. Actually, it was in some sense based on local practices and provided devices.
In conclusion, despite some limitations, this retrospective study demonstrates that NHFOV can reduce intubation and the need for IMV compared with NIPPV and NCPAP as an initial NIV for RDS treatment of preterm infants. To recommend the use of NHFOV as the primary mode of respiratory support for RDS in preterm infants, further multicenter randomized controlled trials are warranted.