Introduction
Single-photon emission computed tomography/computed tomography (SPECT/CT) plays an important role in assessing oral and maxillofacial lesions [1-4]. SPECT/CT is useful not only for detecting jaw bone invasion of oral cancer but also for surgical planning [5]. Furthermore, radiologic-pathologic correlation of medication-related osteonecrosis of the jaw (MRONJ) could be achieved using SPECT/CT [6].
SPECT/CT can provide the quantitative parameter standardized uptake value (SUV) [7,8]. Quantitative SPECT/CT offers the possibility to continue and expand the potential of quantitative nuclear medicine applications [9,10]. Quantitative salivary gland SPECT/CT holds promise as an objective imaging modality for assessment of salivary dysfunction [11-13]. Furthermore, SUV using Q.Metrix [14,15] and GI-BONE [16-19] software could be useful for the evaluation of jaw lesions. In recent years, Q.Volumetrix MI and GEniE-Xeleris 4 DR were developed. However, to the best of our knowledge, no reports have been published on SPECT/CT SUV of jaw lesions using Q.Volumetrix MI and GEniE-Xeleris 4 DR. The aim of this study was to investigate mandibular lesions with SPECT/CT using Q.Volumetrix MI and GEniE-Xeleris 4 DR.
Material and methods
Subjects
This prospective study was approved by the ethics committee of our university (ECNG-R-318). After providing written informed consent, 8 patients (2 men and 6 women; mean age 71.1 years [range 52-91 years]) with mandibular lesions (4 MRONJ, 3 chronic osteomyelitis, and 1 squamous cell carcinoma) underwent SPECT/CT at our university hospital from January 2020 to March 2021.
SPECT/CT imaging
SPECT/CT scans were obtained using a SPECT/CT scanner (Optima NM/CT 640, GE Healthcare, Tokyo, Japan), following our institutional protocol [14]. Patients were administered an intravenous injection of 740 MBq of technetium 99m hydroxymethylene diphosphonate (99mTc-HMDP, Clear Bone Injectable, Nihon MediPhysics, Tokyo, Japan) prior to the SPECT acquisition.
Data analysis
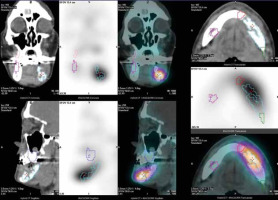
The maximum SUV was obtained by using software and a workstation (Q.Volumetrix MI and GEniE-Xeleris 4 DR, respectively, GE Healthcare, Tokyo, Japan). The localization and size of volume of interest (VOI) can be drawn over the lesion, mesial, distal, and opposite side as normal using the CT, SPECT, and SPECT/CT transaxials, coronals, and sagittals as the anatomical reference (Figure 1). Q.Volumetrix MI can analyse SUV of lesions by organ segmentation using optional pan and zoom imaging. Then, the dosimetry software provided multiple quantitative data for a given VOI. The maximum SUV in a given VOI was calculated as follows: maximum SUV = (maximum radioactivity/voxel volume)/(injected radioactivity/body weight).
Figure 1
Q.Volumetrix MI and GEniE-Xeleris 4 DR. Using the computed tomography (CT), single-photon emission computed tomography (SPECT), SPECT/CT transaxials, coronals, and sagittals as the anatomical reference, the localization and size of volume of interest (VOI) was automatically drawn over the lesion (sky blue), mesial (red), distal (green), and opposite side as normal (pink)
Results
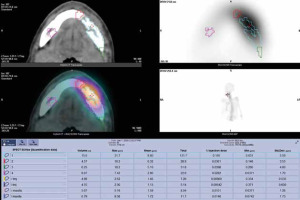
Table 1 shows 8 cases of SPECT/CT maximum SUV for mandibular lesions. Maximum SUVs for MRONJ (n = 4, 25.4 ± 4.9), chronic osteomyelitis (n = 3, 14.6 ± 3.1), and squamous cell carcinoma (n = 1, 31.7) were significantly higher than those of the opposite side as normal mandible (3.8 ± 0.7, 4.6 ± 1.8 and 7.4, p = 0.000), respectively. Figures 2 and 3 indicate cases of chronic osteomyelitis (case 5) and squamous cell carcinoma (case 8), respectively.
Table 1
Cases of single-photon emission computed tomography (SPECT)/computed tomography (CT) maximum standardized uptake value for mandibular lesions
Figure 2
Chronic osteomyelitis of the right side of the mandible in a 69-year-old man (case 5). Computed tomography (CT), single-photon emission computed tomography (SPECT), SPECT/CT, and maximum intensity projection (MIP) show a hot spot in the mandible. Maximum standardized uptake values (SUVs) of lesion (sky blue), mesial (red), distal (green), and normal (pink) were 18.20, 6.19, 5.24, and 5.51, respectively
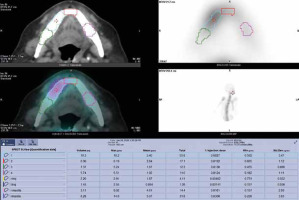
Figure 3
Squamous cell carcinoma of the left side of the mandible in a 59-year-old man (case 8). Computed tomography (CT), single-photon emission computed tomography (SPECT), SPECT/CT, and maximum intensity projection (MIP) show a hot spot in the mandible. Maximum standardized uptake values (SUVs) of lesion (sky blue), mesial (red), distal (green), and normal (pink) were 31.70, 18.20, 18.20, and 7.42, respectively
Discussion
Despite SPECT/CT playing an important role in assessing oral and maxillofacial lesions [1-4], few reports have been published on SPECT/CT SUV of jaw lesions. In our study, SPECT/CT SUV using Q.Volumetrix MI showed potential as a useful parameter for the evaluation of mandibular lesions, such as detection and surgical planning.
Regarding comparison of utility with other molecular imaging applications, Q.Volumetrix MI is better than Q.Metrix [14,15] at operability, because SUV analysis using Q.Volumetrix MI involves 1 step; however, Q.Metrix involves 2 steps (preparation for Q.Metrix and Q.Metrix). Furthermore, Q.Volumetrix MI is better than Q.Metrix regarding resolution, because Q.Volumetrix MI is a 512 matrix; however, Q.Metrix is a 256 matrix. Therefore, the localization and size of VOI can be drawn over the lesion, mesial, distal, and opposite side as normal using the CT, SPECT, and SPECT/CT transaxials, coronals, and sagittals as the anatomical reference by optional pan and zoom imaging. We consider that SUV using Q.Volumetrix MI software could be useful for the evaluation of jaw lesions.
Modabber et al. [3] concluded that SPECT/CT can safely detect different kinds of inflammatory jaw pathologies compared to other conventional imaging modalities; additionally, SPECT/CT assists the surgeon in determining the expansion of the process preoperatively, thereby optimizing surgery planning. Miyashita et al. [6] showed that the presence of regenerative vascularity with necrosis or inflammation seems to determine bone metabolism in MRONJ using 3-dimensional (3D) SPECT/CT. In this study, maximum SUVs for MRONJ (n = 4, 25.4 ± 4.9) and chronic osteomyelitis (n = 3, 14.6 ± 3.1) in mandible were higher than those of the opposite side as normal mandible (3.8 ± 0.7 and 4.6 ± 1.8, respectively). Furthermore, Ogura et al. [20] showed that surgical specimens from segmental mandibulectomy of MRONJ were analysed using cone-beam computed tomography (CBCT), and CBCT could be useful for the post-surgical evaluation of MRONJ. Miyashita et al. [5] indicated that 3D SPECT/CT is useful not only for detecting jaw bone invasion of oral cancer but also for surgical planning. In this study, the maximum SUV for squamous cell carcinoma in mandible (n = 1, 31.7) was higher than that of the opposite side as normal mandible (7.4). Furthermore, Q.Volumetrix MI can analyse SUV of lesions by organ segmentation, such as the lesion, mesial, distal, and opposite side as normal, using optional pan and zoom imaging. We consider that SPECT/CT SUV using volumetric analysis showed potential as a useful parameter for evaluation of MRONJ and malignant tumour of the jaw, such as detecting, surgical planning, and post-surgical evaluation.
There were several limitations of this study. The sample was relatively small. Power calculation because of small sample sizes would strengthen the study, otherwise this is a significant limitation. Furthermore, we showed only maximum SUVs in this study, but there are other parameters concerning volumes and activities that should be utilized. Therefore, further research is necessary to validate these results.


