Introduction
Isolated fallopian tube anomalies belong to a group of rare disorders. Some authors mention several cases of isolated segmental absence of one of the fallopian tubes [1], reporting an incidence of 1/11,240 for unilateral abnormalities of the oviducts [2], or simply describing it as uncommon [3]. Abnormalities of Mullerian development are often found on evaluation for infertility or incidentally on intraabdominal examination. The mechanism of this malformation is usually not well elucidated [4]. Fallopian tube anomalies can manifest with infertility or unspecified abdominal pains, or they might present as completely asymptomatic. Isolated segmental absence of the fallopian tube is an even more uncommon anomaly, with only a few cases described in the literature [1, 5]. In this article we present a case of isolated bilateral distal segmental absence of fallopian tubes.
Case report
A 22-year-old woman was admitted to the Department of Surgical, Endoscopic, and Oncological Gynaecology of the Polish Mothers’ Memorial Hospital Research Institute due to a suspicion of large bilateral hydrosalpinx, revelaed on a routine transvaginal ultrasound examination. On admission the patient complained of irregular, mild abdominal pains. Her clinical history was unremarkable, and her menstrual cycles were regular and painless. The patient reported never having had intercourse or any sort of sexual relations. Cultures for chlamydia and other common sexually transmitted pathogens were negative. There was an unsuccessful attempt of conservative treatment with antibiotics, implemented due to the patient’s initial complaints. Due to a strong suspicion of bilateral hydrosalpinx of unclear aetiology, a decision to perform a diagnostic laparoscopy with possible concomitant chromopertubation was made. In the event of occlusion of both fallopian tubes and no technical possibility to restore the fallopian continuity, the patient was informed that bilateral salpingectomy was an option.
After a typical introduction of the trocars a normal uterus and 2 ovaries were observed. Both oviducts, on the other hand, were massively distended and distorted, confirming the initial diagnosis of bilateral hydrosalpinx. A precise inspection of the fallopian tubes proved no continuity between proximal segments of the oviducts and hypoplastic infundibular portions with almost non-existent fimbriae with the distance between each oviduct and its respective atretic infundibulum being about 2 cm. Bilaterally, the fimbriae exhibited signs of severe atrophy/atresia. Additionally, endometriotic implants were found in the vicinity of the left ovarian fossa and the rectouterine pouch peritoneum. No evidence of other post-inflammatory damage was noted within the pelvis. Using the smallest speculum, a narrow catheter was inserted to the uterine cavity to introduce a dye and assess the fallopian tubes’ patency. In view of the fact that the fallopian tubes proved to be bilaterally obstructed and severely distorted, as well as the fact that there was no technical possibility of recreating the tubal patency (completely destroyed, almost non-existent fimbriae), we decided to perform a bilateral salpingectomy. Histopathologic examination revealed locally enlarged fallopian tubes with only residual lumen in the parts with seemingly normal diameter (Fig. 1–4).
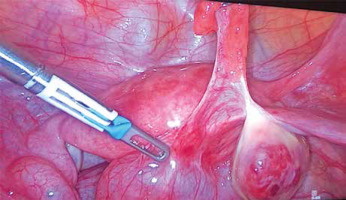
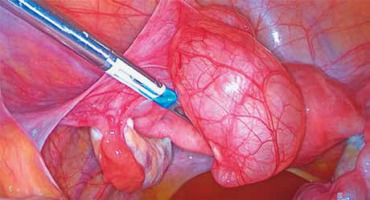
Fig. 2
Intraoperative views of the left fallopian tube
There is a visible lack of connection between the fallopian tube, entirely enlarged by hydrosalpinx, and its fimbriae. The ovary remains unchanged
Discussion
The fallopian tubes are paired structures that extend from the ovaries to the uterus. Their main function is to conduct an ovum from the ovary to the uterus, transport sperm cells in the opposite direction, and finally to transport a fertilized ovum to the uterine cavity. Usually about 10–12 cm long and 1–4 mm wide, the oviducts consist of 4 parts: the intrauterine part, the isthmus, the ampulla, and the infundibulum with fimbriae, which are slender, irregular processes arising from folded mucosa of the fallopian tube. Histologically, the oviduct is comprised of several layers. The innermost layer is the mucosa. Its epithelium includes column-shaped cells, peg cells, and cilia that respectively produce tubal fluid and facilitate the transport within the oviduct. The muscular layer is comprised of outer longitudinal and inner circular smooth muscle fibres that allow peristalsis of the fallopian tubes. The most external layer, the serosa, is derived from the visceral perineum, whereas the subserosa consists of loose adventitious tissue, blood vessels, lymphatics, and nerves [6].
The patient presented above represents a rare group of isolated, bilateral fallopian tube pathologies with no concomitant abnormalities of the remaining genitourinary system. It is known that during embryological development of the female reproductive system, around the 6th week of pregnancy, the Mullerian (paramesonephric) ducts fuse partially, forming uterovaginal primordium from their caudal tips and fallopian tubes from their cranial portions. Different malformations might appear if there is failure on any stage of the fusion of the paramesonephric ducts [6]. Diagnosis is very challenging because in most cases those abnormalities are not easily seen on ultrasound, computed tomography, or even magnetic resonance imaging. Hysterosalpingography allows us to visualise the course and partially the anatomy (or, more likely, patency) of the oviducts, which makes it a very good diagnostic tool. The most objective and certain diagnosis, however, can be obtained through laparoscopy, with a histopathological examination performed if necessary. Usually, the diagnosis is made accidentally during the diagnostic process for infertility.
The literature mentions various cases of subtle oviduct pathologies, such as tubal diverticula, hydatid of Morgagni, accessory fallopian tube, accessory ostium, phimosis, fimbrial agglutination, or tubal sacculation, which may play an important role in female infertility and occasionally might be accompanied by endometrial implants. Out of the anomalies mentioned above, a tubal diverticulum might be mistaken for hydrosalpinx; however, they are easily distinguishable by a contrast medium trial – in the case of tubal diverticulum the contrast would eventually drain into the peritoneal cavity, whereas in hydrosalpinx no contrast would be visible. Another possible diagnosis would be phimosis, which is a concentric stricture of the fallopian tube at its distal end; however, it presumes tubal patency, which in turn allows easy differentiation with hydrosalpinx [6].
Hydrosalpinx develops due to a blocked, dilated, fluid-filled fallopian tube. It is a very rare finding in sexually inactive women without inflammatory disease and especially rare in children and adolescents. Sporadic cases of unilateral noninflammatory hydrosalpinx were reported as isolated postsurgical complications, complications of peritoneal drains [7], or – in one case – endometriosis in an adolescent patient [8]; however, none of those seems to be applicable in our case. It is well-known that hydrosalpinx may develop as a result of an infection – the most common pathogen being Chlamydia trachomatis. In a study carried out by Raoofi et al. [9] Chlamydia trachomatis IgG antibodies were significantly higher in women with bilateral tubal disease, whereas 5 out of 30 seronegative examined women had unilateral tubal abnormality. None of the seronegative subjects suffered from bilateral tubal obstruction as seen in our patient.
Other authors mention several cases of isolated segmental absence of one of the fallopian tubes [1], reporting an incidence of 1/11,240 for unilateral abnormalities of the oviducts [2], or simply describing it as uncommon [3]. Three theories have been proposed to explain this phenomenon: the first suggesting an asymptomatic torsion with subsequent necrosis of the tube [10] (such torsion can appear even during the foetal life), the second proposing a vascular accident with secondary ischaemia, and the third concentrating on developmental disorders of paramesonephric and mesonephric ducts [10–12]. Although it is known that hydrosalpinx might be a risk factor for a fallopian tube torsion (along with tubal malformations, paratubal cysts, venous congestion, physiological abnormalities, trauma, previous surgery, pregnancy) [1], it seems highly unlikely for that to happen in both oviducts simultaneously. Furthermore, in our patient the tubal segment lost to the torsion would be longer, there were no nearby adhesions observed (which might have been present in case of inflammation sometimes associated with torsion), both ovaries were normal, and the patient presented no history of potentially torsion-related acute abdominal pain [1, 12].
Uckuyu et al. described a series of 4 cases similar to the one we present [5]; however, all of the patients manifested a unilateral tubal and/or ovarian absence, and therefore an underlying vascular event had been suggested, unlike in our case, where we were inclined to assume a congenital malformation as the reason for the pathology observed, similarly to a case of congenital absence of distal fallopian tubes with traces of endometriosis in rectovaginal pouch and right pelvic side wall, presented by McBean et al. [13] – in this case, however, the oviducts did not develop hydrosalpinx. Kozlowski et al. describe a case of bilateral atresia of the proximal ampulla of both tubes with a normal proximal segment consistent with a torsion event [10]. A similar observation was made by Tulusan [14], who described a case of complete bilateral absence of the muscular layer of the ampullary part of the fallopian tube with distorted fimbriae; however, in this patient the fimbriae were pathologically elongated. Paterson et al. [3] reported a case in which the left proximal tube was absent, and the distal end separated into 3 portions.
An interesting classification of tubal pathologies was proposed by Nishiyama et al. [4]. The author suggests a division of all cases of bilateral tubal atresia into 4 categories: absence of both the ovaries and fallopian tubes, anomalies of both the ovaries and fallopian tubes, anomalies of fallopian tubes only, and anomalies of fallopian tubes and uterus with normal ovaries. According to this proposition, our case falls into the third category, along with 3 cases reported by Kozlowski et al. [10], McBean et al. [13], and Tulusan [14], all of which are described above in more detail. Another classification was proposed by Paterson et al. [3] – the authors divided congenital tubal anomalies into 3 groups: a) complete absence, b) partial or segmental absence, and c) duplication, accessory ostia and tubes, multiple lumina and diverticula. According to this classification, our patient would be found in the second category.
Management of this rare group of disorders remains unclear. Because the number of cases is relatively small, there is no consensus on treatment [1]. If the oviduct pathology does not cause its obstruction, usually no further action is necessary, because it does not interfere with the fallopian tube primary function, which is to enable transport of germ cells and fertilisation. If, however, a patient suffers from bilateral tubal obstruction, then we could consider excising the absent segments and performing tubal reanastomosis. Unfortunately, in our case that was not possible because of complete destruction of fimbriae and symmetrically distorted, distended oviducts, which was why the decision to perform bilateral salpingectomy was made. Patients with unilateral fallopian tube pathology constitute another challenge – both conservative and invasive treatment might be an option depending on the pathogenesis of the condition, individual characteristics of the patient, presented symptoms, and procreative plans.
In summary, our case belongs to a group of pathologies that is not yet well understood. Given the common asymptomatic presentation of the condition, a large group of patients will never be diagnosed with fallopian tube disorders, and we will not know their exact occurrence rate. Even though structural anomalies of the oviduct require a detailed examination of the patient in search of potential associated anomalies, it is possible to confirm a diagnosis of isolated structural anomaly of the fallopian tube. Whether the reason for the pathology is a vascular incident, a torsion episode, or a congenital defect, the treatment must be carefully planned with respect to the patient’s wishes and procreative plans.
Conclusions
Isolated structural anomalies of the fallopian tube are rare and infrequently reported in the literature. Although usually asymptomatic, they might also manifest as acute abdominal pain or infertility. Various aetiologies have been proposed to explain this phenomenon, ranging from congenital to vascular events. We present a patient with an isolated, bilateral, distal absence of fallopian tubes, which resulted in bilateral hydrosalpinx and occlusion of fallopian tubes. To our knowledge, this is the only case described in the literature, but several similar cases have been reported over the years.