Summary
Mitral regurgitation (MR) is a frequent coincidence in patients with severe aortic stenosis (AS). The major cause of MR in this setting is MR secondary to the AS (functional/secondary), while the primary pathology of the mitral valve apparatus (organic/primary MR) is less common. Echocardiographic assessment of MR was performed at baseline, at 30 days and at 6 months after balloon aortic valvuloplasty (BAV), when indicated. Balloon aortic valvuloplasty may reduce MR in mid-term follow-up. Predictors of persistent MR at 6 months after BAV included an increase of left ventricle end-systolic diameter and MR jet area and decrease of left ventricle ejection fraction at 30 days, as well as the presence of primary MR.
Introduction
Mitral regurgitation (MR) is a frequent complication in patients with severe aortic stenosis (AS), occurring in up to 65% of cases [1, 2]. The major cause of MR in this setting is MR secondary to the AS (functional/secondary), while the primary pathology of the mitral valve apparatus (organic/primary MR) is less common [1, 3]. The coexistence of significant MR has been associated with adverse outcomes in patients with severe AS [4–8]. Balloon aortic valvuloplasty (BAV) is offered as a bridge therapy in hemodynamically unstable patients to conventional surgical aortic valve replacement (AVR) or transcatheter aortic valve implantation (TAVI) for elderly and frail patients with severe AS [9]. Data on the effects of BAV on MR and TR are scarce.
Material and methods
Study population
The data of all consecutive patients with severe symptomatic AS with an aortic valve area (AVA) < 0.7 cm2 (indexed AVA < 0.5 cm2/m2 body surface area) and/or mean transaortic gradient ≥ 40 mm Hg who underwent BAV between December 2008 and May 2021 at two tertiary university centers were included.
Methods
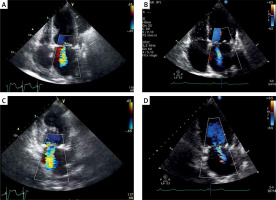
Detailed material and methods were described previously [10, 11]. Transthoracic echocardiography (TTE) served as a tool for MR assessment at baseline, after 30 days and at 6 months. Echocardiography was performed using the commercially available ultrasound systems VIVID 7 (GE, Boston, USA) and iE33 (Philips Ultrasound, Bothell, Washington, United States). Echocardiographic evaluation was performed by three experienced echocardiographers, blinded to clinical data and further data of post-BAV outcomes. MR was quantified in the apical long-axis view by measuring the MR jet area at mid-systole [12]. The severity of MR was graded by the MR jet area relative to the left atrial area, as follows: none or trace; mild (MR jet area < 20%); moderate (MR jet area 20–40%); or severe (MR jet area ≥ 40%). At least moderate MR grade was considered clinically significant and patients with confirmed at least moderate MR were included in the MR group.
Ethical issues
Ethical review and approval were waived for this study, due to the retrospective character of the study, yet the institutional board was informed and acknowledged the study. This study, which involves human participants, complies with the 1964 Helsinki Declaration and its later amendments.
Statistical analysis
Continuous variables were expressed as a median (interquartile range) and categorical variables were expressed as a number (percentage). Continuous variables were compared by the t-test for dependent samples when normally distributed or by Wilcoxon’s signed-rank test when not normally distributed. Categorical variables were compared by Pearson’s χ2 test and Fisher’s exact test. The Pearson rank correlation coefficient for normally distributed variables or Spearman’s rank correlation coefficient for non-normally distributed variables was calculated to test the association between two variables. Univariate logistic regression analysis was initially used to identify parameters associated with persisting significant MR at 6 months after BAV. Significant parameters were entered in a multivariate analysis, using stepwise selection, to identify independent predictors of significant MR after BAV at 6 months. The entry criterion for an individual item into the multivariable logistic regression model was p < 0.05. The significance level was set at p < 0.05. Statistical analysis was performed using IBM SPSS Statistics for Windows, Version 25.0 (IBM Corporation, Armonk, NY, USA).
Results
Clinical data
A total of 382 BAVs in 374 patients were performed. The procedural success rate was 94.6%. Detailed baseline characteristics, procedural data, complication rate and outcomes were reported previously [11]. Of 374 patients, 26.2% (n = 98) had concomitant at least moderate MR (the MR group). Of the initial group of 374 patients, 103 (27.5%) were not available for the 6-month follow-up due to death (n = 81), requiring subsequent AVR (n = 8) or TAVI (n = 14) in the meantime.
Echocardiographic data
The echocardiography data at baseline and at 1 and 6 months after BAV for the remaining 271 patients are included in our final analysis. Of these, 21.2% (n = 85) had at least moderate MR at baseline (in 19 subjects (22.3%) MR was diagnosed as primary). The baseline characteristics of the patients with or without baseline MR are summarized in Table I.
Table I
Baseline characteristics of patients treated with balloon aortic valvuloplasty according to baseline mitral regurgitation
The two groups were similar in terms of baseline clinical data, except for history of neoplasm and syncope, which were more frequent in the non-MR group than in the MR group (10.7 vs. 3.5%; p = 0.04 and 12.4 vs. 5.9%; p = 0.04, respectively). Echocardiographic data are presented in Table II. Regarding baseline echocardiography parameters, the two groups showed similar severity of AS, but patients in the MR group had a greater left ventricle (LV) size (LV end-diastolic diameter (LVEDD), 47.8 (41.3–52.4) mm vs. 43.2 (35.2–46.8) mm; p = 0.002; LV end-systolic diameter (LVESD), 36.2 (34.9–43.2) mm vs. 26.9 (25.2–38.7) mm; p = 0.003) and slightly lower LV ejection fraction (40.1 (31.5–50.5)% vs. 45.3 (35.3–55.4)%; p = 0.04). The LV size was significantly reduced at 30 days and 6 months after BAV in the MR group (p < 0.001 for LVEDD and LVESD, Table II), but not in the non-MR group (p = 0.45 for LVEDD and p = 0.65 for LVESD). Mitral regurgitation parameters significantly improved both at 30 days and 6 months after BAV in the MR group (Table II, Figure 1), but only in 5 out of 19 patients with organic MR. At 6 months after BAV, significant MR persisted in 18 (21.2%) patients in the MR group. In 65 patients of the MR group, 54 (63.5%) patients had an improvement of MR jet area < 4.0 cm2 and 11 (12.9%) patients improved but significant MR still remained. In 2 (2.3%) patients MR worsened compared with baseline. The odds ratio (OR) and 95% confidence interval (CI) for univariate and multivariate logistic regression analysis of the variables associated with persisting significant MR are presented in Table III. In multivariate logistic regression analysis, the change at 30 days, from baseline, in the LVESD (OR = 1.87; 95% CI: 1.23–2.87; p < 0.001) and LVEF (OR = 0.95; 95% CI: 0.87–1.01; p < 0.001), MR jet area (OR = 2.2, 95% CI: 1.5–4.6; p < 0.001) and the presence of primary MR (OR = 3.2, 95% CI: 1.04–5.98; p < 0.001) were retained as independent predictors of significant persisting MR at 6 months after BAV.
Table II
Echocardiographic data of the MR group
| Parameter | Baseline (n = 85) | 30 days after BAV | P-value | 6 months after BAV | P-value* |
|---|---|---|---|---|---|
| Peak systolic velocity, median (IQR) [m/s] | 4.9 (4.3–5.4) | 3.8 (3.4–4.1) | < 0.001 | 4.2 (3.5–4.5) | < 0.001 |
| Mean transaortic gradient, median (IQR) [mm Hg] | 42.2 (40.5–56.3) | 28.4 (20.1–34.3) | < 0.001 | 36.7 (30.5–43.6) | < 0.001 |
| Aortic valve area, median (IQR) [cm2] | 0.48 (0.41–0.60) | 0.81 (0.66–0.94) | < 0.001 | 0.70 (0.62–0.82) | < 0.001 |
| Left ventricle ejection fraction, median (IQR) (%) | 40.1 (31.5–50.5) | 45.2 (37.3–52.2) | <0.001 | 44.1 (39.2–53.4) | 0.04 |
| Left ventricle end-diastolic diameter [mm] | 47.8 (41.3–52.4) | 45.5 (39.2–51.1) | < 0.001 | 44.2 (39.4–52.2) | < 0.001 |
| Left ventricle end-systolic diameter [mm] | 36.2 (34.9–43.2) | 33.4 (33.1–42.6) | < 0.001 | 32.9 (33.3–41.9 | < 0.001 |
| Mitral regurgitation: | |||||
| MR jet area [cm2] | 7.2 (4.5–9.9) | 3.6 (2.3–7.2) | < 0.001 | 3.2 (2.1–6.7) | < 0.001 |
| %MR/LAA, % | 34.5 (23.4–42.7) | 17.5 (9.3–29.5) | < 0.001 | 14.5 (8.3–24.5) | < 0.001 |
Table III
Univariate and multivariate analysis for prediction of persistent severe MR after 6 months
| Parameter | Univariate analysis OR (95% CI) | P-value | Multivariate analysis OR (95% CI) | P-value |
|---|---|---|---|---|
| Age | 0.99 (0.92–1.12) | 0.87 | ||
| Sex (female) | 1.45 (0.59–2.98) | 0.76 | ||
| LVESD | 0.97 (0.79–1.46) | 0.54 | ||
| LVEDD | 0.96 (0.82–1.78) | 0.65 | ||
| LVEF | 1.01 (0.98–1.07) | 0.59 | ||
| AVA | 2.57 (0.54–6.33) | 0.12 | ||
| MR jet area | 1.54 (0.99–1.99) | 0.26 | ||
| ΔLVESD* | 1.6 (1.21–2.51) | 0.002 | 1.87 (1.23–2.87) | < 0.001 |
| ΔLVEF* | 0.98 (0.96–1.03) | 0.003 | 0.95 (0.87–1.01) | < 0.001 |
| ΔMR jet area* | 1.7 (1.44–3.51) | 0.001 | 2.2 (1.53–4.69) | < 0.001 |
| Organic MR | 2.1 (0.99–4.87) | 0.001 | 3.2 (1.04–5.98) | < 0.001 |
Discussion
In our two-center study, concomitant at least moderate MR was noted in 26.2% of patients with severe AS undergoing BAV. The reduction of MR following BAV was observed in the majority of patients. In addition, the increase of LVESD and MR jet area and decrease of LVEF at 30 days, as well as the presence of primary MR, were identified as independent predictors of persistent MR at 6 months. Our findings seem to be relatively important due to the paucity of data on MR reduction after BAV in patients with AS.
Mitral regurgitation is present in up to 65% of patients with severe AS [1, 2]. The cause of MR in patients with severe AS in most cases is functional [3]. However, with the increasing age of AS patients, mitral apparatus may present calcifications and other degenerative processes resulting in organic MR. The coexistence of significant MR, independent of its etiology, has been associated with adverse outcomes in patients with severe AS [4–8]. Balloon aortic valvuloplasty is a recognized and recommended treatment in patients with severe AS who are hemodynamically unstable or require urgent non-cardiac high-risk surgery as a bridge to definite treatment [9, 13]. Immediate results of BAV include an increase in AVA and a decrease in maximal and median transaortic gradient [14–20]. Moreover, in most patients, improvement of LVEF was crucial for better outcomes [10, 13]. The data on MR reduction after BAV are limited. In a study by Masaki et al. a significant reduction of MR was observed at 1 month and 3 months after the procedure, with the change at 1 month in the LVESD and MR jet area being predictive of persisting significant MR at 3 months after BAV [21]. Maluenda et al. found that nearly half of the patients with severe AS and coexistent MR showed improvement in the magnitude of MR after BAV [22]. Larger left atrial and LVEDD and higher transaortic valve gradients were associated with a lack of MR improvement [22]. On the other hand, worsening of MR directly after BAV was also reported and was related to LV wire interaction with the mitral apparatus [23, 24]. In a study by Come et al., one of the first studies assessing MR after BAV, mitral regurgitant score decreased significantly compared to baseline and immediately after the procedure [25]. Transcatheter aortic valve replacement (TAVR) is a definite treatment for patients with severe AS who are too old or too sick to undergo AVR. There is no doubt that TAVR is a valuable treatment option reflected in current ESC guidelines on valvular heart disease [9]. There are numerous data on the beneficial role of TAVR and many papers have shown a significant MR reduction immediately after or during follow-up after TAVR [26–31]. Similar results were reported for patients with low-flow and low gradient AS [32]. The majority of available data assessed post-TAVR MR only up to 12 months after the index procedure and showed persistent MR reduction compared to baseline. Also, many studies have assessed the impact of MR on long-term mortality (up to 3 or 5 years). However, none of them evaluated MR grade at that time. In a study by Voisine et al., data of patients with pure severe AS and significant MR undergoing AVR or aortomitral surgery were analyzed and MR reduction was present in only 60% of subjects but persistent up to 2 years [33]. In our study, post-BAV MR was assessed only up to 6 months after the index procedure. There is a lack of data showing at least 1-year beneficial results of MR reduction after BAV. The reason for that may be that 6 months is the maximal time window to schedule the patient for final treatment (TAVR or AVR). The majority of patients still treated conservatively beyond 6 months have an extremely poor prognosis with mortality at 12 months up to 69% [10].
The study findings were derived from observational analyses, which are subject to well-known limitations. However, our data present everyday clinical practice with consecutive patients enrolled. Another limitation was the lack of data on patients (27.5%) who dropped out from the analysis due to death or definitive treatment. Referring to methodology, it is known that MR parameters used in our study are inferior to indices such as vena contracta and effective regurgitant orifice area; however, only these parameters could be calculated, considering the enrollment period and available acquisition.