Introduction
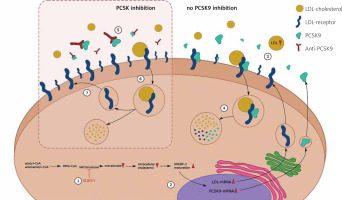
Proprotein convertase subtilisin/kexin 9 (PCSK9) is a key regulator of low-density lipoprotein (LDL) metabolism. PCSK9 binds to the LDL receptors (LDL-R) on the surface of hepatocytes, leading to degradation in lysosomes and to higher plasma levels of LDL cholesterol (LDL-C) [1]. The main sources of PCSK9 are the liver, intestines, and kidneys [2]. An animal study on PCSK9-knockout mice has shown that the absence of hepatic PCSK9 results in a two-thirds reduction in circulating LDL-C, which suggests that intestinal and renal PCSK9 expression has a minor effect on circulating LDL-C phenotype [3]. Human monoclonal antibodies, such as alirocumab or evolocumab, bind plasma PCSK9 and prevent LDL-R from degradation, leading to lower LDL-C plasma levels [4–6]. PCSK9 inhibitors (PCSK9i) are successfully used in patients with familial hypercholesterolaemia [7]. The mechanism of action of PCSK9i is presented in Figure 1. PCSK9 was first considered as a potential target for lipid-lowering therapies when its pathogenic role in familial hypercholesterolaemia was discovered (FH) [8, 9]. However, PCSK9 mutations only account for a small percentage of FH cases, while LDL-R loss-of-function mutations account for about 90% of cases [10]. After initial observation of PCSK9i in FH patients, these drugs showed great efficiency in lowering cholesterol levels and cardiovascular risk in patients who were simultaneously treated with maximum statin doses in various trials. This led to FDA approval of the treatment [11, 12].
Figure 1
Mechanism of action of statins and PCSK9 inhibitors. The figure supports the combined targeted cholesterol-lowering therapy with a statin and a PCSK9 inhibitor. (1) Statins decrease cholesterol production by blocking HMG-CoA reductase, preventing the conversion of HMG-CoA to mevalonic acid. (2) The lowered concentration of intracellular cholesterol promotes the maturation of SREBP-2 and increases the expression of genes encoding LDL and PCSK9. (3) The increased number of receptors on the cell surface enables increased LDL uptake and a reduction in extracellular cholesterol levels. (4) Once bound to LDL and PCSK9, the LDL receptor is internalized and degraded in the lysosomes. (5) Anti-PCSK9 antibodies, known as PCSK9 inhibitors, bind to PCSK9, preventing them from binding to the LDL receptor. (6) The LDL receptor is internalized after binding to LDL, but in the absence of PCSK9, only the cholesterol molecule is degraded in the lysosome. (7) LDL receptors return to the cell surface and their increased concentration results in increased LDL uptake
The term metabolic-associated fatty liver disease (MAFLD), known also as non-alcoholic fatty liver disease (NAFLD), covers a range of liver diseases caused by the accumulation of fat in more than 5% of hepatocytes. The continuum begins with benign metabolic (or non-alcoholic) fatty liver, which may cause steatohepatitis with steatosis, hepatocellular ballooning, inflammation, and cirrhosis, possibly resulting in end-stage liver disease or neoplastic transformation to hepatocellular carcinoma (HCC) [13, 14]. MAFLD is currently the most common liver disease, affecting more than 25% of the adult population worldwide, with incident rates expected to rise [14, 15]. MAFLD is a risk factor for cardiovascular disease, type II diabetes, and chronic kidney disease [16–19]. The proposal to rename NAFLD to MAFLD of Eslam et al. (2019) produced a consensus and subsequently changed the approach to diagnosis. Rather than being a diagnosis of exclusion, MAFLD is now diagnosed on the basis of detecting liver fat accumulation (with imaging, liver biopsy, or blood biomarkers) with the coexistence of one of 3 major criteria: obesity or overweight, type-2 diabetes mellitus, and the presence of 2 or more metabolic abnormalities [20, 21]. The current main approach to MAFLD therapy is to implement diet and lifestyle interventions. Due to patients’ inconsistency or advanced stage of disease, traditional approaches can help only to a certain extent. In an increasing number of cases, there is an ongoing need for novel pharmacological treatments, if patient outcomes are to be improved. A vast variety of strategies are being investigated, with the main focus on insulin resistance (metformin, thiazolidinediones), decreasing the effects of oxidative stress (vitamin E, pentoxifylline), targeting proinflammatory cytokines (anti-TNF-α, TGF-β, IL-11), and others [14]. Finally, one of the key approaches is to lower cholesterol levels using statins, ezetimibe, and the novel treatments using proprotein convertase subtilisin/kexin 9 inhibitors, which we focus on in this review.
The role of PCSK9 in MAFLD pathogenesis
Recent studies have pointed out the role of PCSK9 in the pathogenesis of MAFLD. This section highlights advances in understanding the effects of PCSK9 gene variants on MAFLD development, the effect of PCSK9 on MAFLD progression, and the mechanisms underlying inflammation and cirrhosis.
PCSK9 variants associated with MAFLD pathogenesis
PCSK9 plays an essential role in cholesterol homeostasis. Gain-of-function (GOF) mutations and loss-of-function (LOF) mutations in the PCSK9 gene result in different outcomes. GOF mutations, as previously discussed, are responsible for a fraction of FH cases. However, some LOF variants may have a beneficial effect on lipid metabolism. Grimaudo et al. conducted a study on 1874 patients at histological risk of NASH and reported that some loss-of-function PCSK9 variants were protective against liver damage, including liver steatosis, NASH, and fibrosis in individuals at risk. Patients with the LOF variant of PCSK had lower LDL-C levels, and PCSK9 hepatic expression was directly correlated with severity of liver steatosis. In animal models of male mice, inducing an overexpression of PCSK9 led to liver fibrosis and NASH [22]. In another study, hepatic PCSK9 mRNA showed a positive correlation with the expression of genes involved in lipid metabolism, such as FASN and PPARΥ [23]. Welty et al. described loss-of-function PCSK9 variants in patients with hypobetalipoproteinaemia, which are associated with a lower risk of liver damage [24]. In addition, Lee et al. found that gene expression levels that contribute to hepatocellular carcinoma development were significantly lower in PCSK9 knock-out mice [25]. However, different LOF PCSK9 variant carriers were found to have increased hepatic uptake of free fatty acids, greater liver fat accumulation, and a higher risk of hepatic steatosis. Knock-out PCSK9 mice in this study had an increased hepatic uptake of lipids. The authors suggested that, although PCSK9i reduces LDL-C plasma levels, it may also contribute to higher lipid accumulation and development and to the progression of MAFLD [26, 27].
The effects of PCSK9 on lipid accumulation and inflammation
Hepatic steatosis is the main clinical feature characterizing nonalcoholic fatty liver. It is defined by the presence of intrahepatic fat without inflammation or fibrosis indicators. An analysis of 71 patients showed that hepatic expression of PCSK9 mRNA [22], as well as circulating PCSK9 levels [28–30], increased with severity of hepatic steatosis. PCSK9 knock-in mice fed a NASH diet had more pronounced hepatic steatosis than wild-type mice, suggesting the promoting role of PCSK9 in fat infiltration of liver tissue [22]. Grimaudo et al. found that hepatic overexpression of human PCSK9 in male mice accelerated the development of MAFLD and liver fibrosis upon dietary challenge [22]. Diet-induced hepatic steatosis causes downregulation of surface LDLR through de novo PCSK9 synthesis, which may contribute to an increased risk of cardiovascular disease in patients with liver disease [29]. Fatty liver index (FLI), an algorithm based on body mass index (BMI), waist circumference, gamma-glutamyl transpherase (GGT), and triglycerides, has been positively correlated with serum PCSK9 levels in patients with type-2 diabetes [31].
MAFLD, characterized by fat accumulation and steatosis, may progress into more severe entities. Steatohepatitis is defined as the infiltration of inflammatory cells into the lipid-enriched liver, which may later progress to HCC. The PCSK9 loss-of-function variant was reported by Grimaudo et al. to be protective against lobular inflammation, but no association with hepatocellular ballooning was found [22]. Human-PCSK9 knock-in mice fed a NASH diet exhibited more expressed liver fibrosis and macrophage infiltration than wild-type mice [22]. According to these authors, PCSK9 may promote fibrosis development through oxidative stress generation. Ruscica et al. conducted a study on 201 individuals with MAFLD and measured circulating PCSK9 levels that were positively correlated with hepatic necroinflammation, hepatocellular ballooning, and fibrosis stage [30].
Although neutrophil infiltration indicates NASH, and may itself play a role in fibrosis development, He et al. identified the mechanism underlying the opposite process. PCSK9i treatment in mice leads to higher presentation of LDL-R on hepatocyte cell surfaces, which leads to higher uptake of miRNA-223 extracellular vesicles from neutrophils to hepatocytes. Once internalized, miRNA-223 inhibits inflammatory and fibrogenic gene expression, which leads to amelioration of NASH progression [32]. As reported by Zou et al., hepatic PCSK9 levels increased along with the development of hepatic fibrosis [33]. Liver inflammation and fibrosis were ameliorated by CRISPR/Cas9 inhibition of PCSK9 by increasing lipopolysaccharide uptake. It is noteworthy that this effect was limited by end-stage cirrhosis.
While normal alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels do not exclude nonalcoholic fatty liver disease, patients with MAFLD may have moderate elevations of aminotransferases [34, 35]. Circulating PCSK9 levels correlate positively with liver biomarkers, such as alkaline phosphatase (ALP), ALT, AST, and GGT [28]. Furthermore, AST and ALT decreased after PCSK9 was inhibited [33]. Although caution is advised when administering evolocumab to patients with elevated transaminases (because safety studies did not include patients with hepatic impairment), the above data suggest that these patients may also benefit from such therapy [36].
Although most data suggest that PCSK9 contributes to the development of NAFLD, some studies have drawn different conclusions. Wargny et al. did not find any association between circulating PCSK9 and severity of hepatic steatosis or NASH in the at-risk population [37]. There was no correlation between circulating PCSK9 and liver fat content, steatosis severity, NASH activity score, lobular or portal inflammation, ballooning, or fibrosis. There was no association between circulating PCSK9 and transaminases, although a positive correlation with GGT and ALP was reported. Moreover, there was no relation between PCSK9 mRNA expression and NAFLD score or NASH histological severity. The authors nevertheless did not exclude the possibility of the involvement of PCSK9 in the early stages of MAFLD. In a study conducted by Demers et al., PCSK9-mediated CD36 degradation was found to limit triglyceride accumulation in the liver and to prevent liver steatosis [38, 39]. PCSK9 inhibition might thus lead to increased CD36-mediated liver fat uptake and an increased risk of MAFLD. The authors emphasized that this hypothesis requires verification in long-term studies.
Clinical trials evaluating the effects of PCSK9 inhibitors in patients with MAFLD
A randomized study of 40 patients with heterozygous familial hyperlipidaemia showed complete amelioration of previously diagnosed MAFLD and NASH after one year of treatment with a PCSK9 inhibitor (evolocumab or alirocumab) [40]. There were no signs of steatosis, inflammation, or fibrosis. No patient presented with cirrhosis. Furthermore, improvements in liver structure and function were observed, as was a reduction in cardiovascular risk.
Scicali et al. evaluated the effect of PCSK9 inhibitors in patients with MAFLD and genetically confirmed familial hyperlipidaemia [41]. Subjects were divided into a low-TG/HDL group and high-TG/HDL group. Steatosis biomarkers such as triglyceride-glucose index (TyG) and hepatic steatosis index (HIS) were evaluated before and after treatment with PCSK9 inhibitors. After treatment with PCSK9i, the low-TG/HDL group showed lower TyG and HIS than the high-TG/HDL group. After 6 months of PCSK9i therapy, the low-TG/HDL group was found to have higher plasma levels of endogenously secreted receptors for advanced glycation end products (esRAGE) than the high-TG/HDL group; this may have a protective effect in MAFLD pathogenesis [42, 43]. This may thus suggest that patients with MAFLD and low TG/HDL ratio at baseline may benefit more from treatment with PCSK9 inhibitors.
Shafiq et al. explored the effects of PCSK9 inhibitor therapy in a retrospective study of 29 patients. Eight of 11 patients with confirmed MAFLD diagnosis achieved complete radiologic resolution after PCSK9i treatment. Additionally, ALT and AST levels decreased after treatment, with the ALT reduction being statistically significant. Approximately 1.5 years of treatment were needed for radiological improvement to be observed; 2 years were necessary to produce a downward trend in aminotransferase levels [44].
The details of the clinical trials using PCSK9i in patients with MAFLD are presented in Table I.
Table I
Clinical trials evaluating PCSK9i efficacy in MAFLD
| Study, reference | Number of patients; disease type | Study type, regimen (R) | Duration of treatment | Results, Efficacy |
|---|---|---|---|---|
| Dimakopoulou et al. [40] | 40; FH (including 7 NAFLD, 6 NASH) | Randomized, 2 arms; R: evolocumab (140 mg/14 d s.c.); alirocumab (150 mg/14 d s.c.) | 1 year | NAFLD/NASH were ameliorated, no signs of steatosis, inflammation, fibrosis, cirrhosis; CVD risk was reduced with improvements in liver structure and function |
| Scicali et al. [41] | 26; FH with NAFLD with elevated LDL-C despite treatment with statins and ezetimibe | Observational, 1 arm; R: 3 patients started alirocumab 75 mg, 10 patients started alirocumab 150 mg and 13 patients started evolocumab 140 mg | 6 months | After 6 months, patients were divided into 2 subgroups: L-TG/HDL and H-TG/HDL. TyH and HSI (steatosis biomarkers) were significantly reduced in the L-TG/HDL group (p < 0.05) and were lower than H-TG/HDL group |
| Shafiq et al. [44] | 29; treated with PCSK9i for different reasons including 11 with hepatic steatosis diagnosis | Retrospective, chart review-based | Mean duration of PCSK9i treatment: 23.69 ±11.18 months | Out of 11 patients with radiologic diagnosis of liver steatosis, 8 (72.73%) had complete radiological resolution. ALT (p = 0.042) and AST (p = 0.201) levels decreased |
[i] FH – familial hypercholesterolaemia, NAFLD – non-alcoholic fatty liver disease, NASH – non-alcoholic steatohepatitis, s.c. – subcutaneously, CVD – cardio- vascular disease, L-TG/HDL – low triglyceride to high-density lipoprotein ratio, H-TG/HDL – high triglyceride to high-density lipoprotein ratio, LDL-C – low-density lipoprotein C, TyH – triglyceride glucose index, HSI – hepatic steatosis index, ALT – alanine aminotransferase, AST – aspartate aminotransferase.
Discussion
PCSK9 inhibitors seem to be a promising agent for the treatment of metabolic fatty liver disease. Although the number of clinical trials using PCSK9i in the clinical setting is insufficient, their results indicate its high efficacy and safety. PCSK9 inhibitors, as shown in the results of clinical trials reviewed in this article, may reduce liver steatosis, inflammation, and fibrosis. They may also ameliorate cardiovascular risk. Although caution is suggested when prescribing PCSK9i to patients with impaired liver function [36], the study of Shafiq et al. suggests that this treatment can simultaneously decrease AST and ALT levels. The meta-analysis of Zhang et al. showed that there is no significantly increased risk of adverse events in the group treated with PCSK9 inhibitors, in comparison to placebo or ezetimibe; PCSK9 inhibitors are safe and well-tolerated by patients [45].
The increasing number of cases of MAFLD and the lack of effective pharmacological treatment is driving an ongoing need for new therapies. To this end, the pathogenesis of MAFLD needs to be better understood. Despite the evidence of effective use of PCSK9i as a lipid lowering therapy in MAFLD, the role of PCSK9 in this context remains unclear.
Our recommendations for future studies include better evaluation of the efficacy of PCSK9i therapy in individuals with MAFLD, including a larger number of patients and longer observation time. Tools such as TG/HDL ratio and FLI need to be standardized and implemented in order to assess liver function. Further studies are needed to assess the relationship between lipid concentrations, liver biomarkers, and radiological images with the disease progression.
However limited the data, PCSK9 inhibitors appear to have a beneficial effect in patients with MAFLD and represent a possible treatment option in the future.










