Introduction
The role of laparoscopy in the resection of Wilms’ tumor (WT) in children has remained debatable. Although an open approach to renal tumors in children is the gold standard, laparoscopic nephrectomy (LN) is acceptable and can be applied in carefully selected patients. In the latest SIOP-RTSG 2016 UMBRELLA Protocol criteria for LN were incorporated [1]. These criteria are as follows: (1) resection in accordance with oncological principles, (2) adequate lymph node sampling, (3) small, centrally located tumors, (4) tumor removal in a retrieval bag (without morcellation). Laparoscopic nephron-sparing surgery (NSS) is even more controversial but may be acceptable in selected cases of unilateral non-syndromic WT. This technique can be applied in single, small (volume < 300 ml) tumors restricted to one pole of the kidney or located peripherally at the mid-kidney. No less than 66% of renal tissue should be saved after the tumor resection with an adequate margin. It should be noted that oncological safety is of primary importance. The risk of recurrence should be precisely evaluated with regard to the potential nephrologic advantages. What is more interesting, according to the UMBRELLA Protocol rules, if NSS is feasible, it should be preferred. The authors report 8 cases of laparoscopic (hemi)nephrectomy for Wilms’ tumor.
Aim
We report 7 cases of laparoscopic nephrectomy and 1 case of laparoscopic heminephrectomy for Wilms’ tumor. Clinical data, technical feasibility and outcome were analyzed.
Material and methods
Between December 2013 and November 2020, 42 consecutive children with primary renal tumor underwent nephrectomy. From these patients, 11 had an LN. Three patients with other renal malignancies were excluded from the analysis. There were 8 children with Wilms’ tumor (2 boys and 6 girls), aged between 13 months and 7 years. All patients received neoadjuvant chemotherapy according to the current SIOP protocol.
The tumor volume was calculated using the formula proposed by SIOP-2001: V = a × b × c × 0.523 cm3, a = length (cm), b = width (cm), c = thickness (cm). The selection criteria for LN were: unilateral tumor, not crossing the midline, no venous tumor thrombus, significant tumor reduction after preoperative chemotherapy.
The patients’ demographics and clinical data are shown in Table I.
Table I
Demographic and clinical data of patients
Results
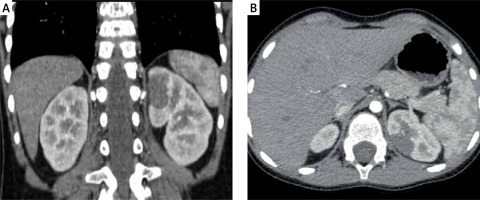
The mean tumor volume before and after chemotherapy was 174.4 ml (range: 14.7–501 ml) and 32.8 ml (range: 4.3–68 ml) respectively. Seven nephrectomies and one left heminephrectomy (NSS) (tumor volume 14.7 ml before chemotherapy (Photos 1 A, B) and 4.3 ml after chemotherapy (Photos 2 A, B)) were performed. LN was performed via the transperitoneal approach in all cases. No patients had an intraoperative tumor rupture. Median operative time for LN was 120 min (range: 100–195 min). The operative time for laparoscopic NSS was 210 min. No conversions to open surgery were needed. The specimen was extracted in a bag without morcellation in all cases. The umbilical trocar was removed. An endobag was inserted through the incision. The specimen was placed into it, and the abdominal cavity was deflated. For the extraction, the umbilical incision was extended 1–2 cm up and down according to the size of the specimen. All children had an attempt of lymph node sampling. Their number per pathology assessment ranged from 0 to 5 (median 2). In only one patient the number of harvested lymph nodes was zero. In this case no lymph nodes were observed visually and adipose tissue in the station which should contain small lymph nodes was removed. In the remaining patients the number of sampled lymph nodes was 2 in 5 cases, 3 in 1 case and 5 also in 1 case. All analyzed lymph nodes were negative for malignancy. The mean time of hospitalization was 3.5 days (range: 2–17).
Photo 1
A, B – Computed tomography scan of tumor at diagnosis showing an upper pole renal mass (tumor volume 14.7 ml)
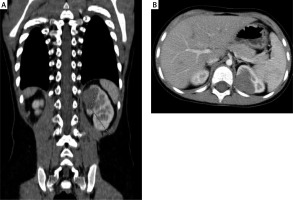
There were no intraoperative events. One complication after heminephrectomy occurred. A 5-year-old girl (patient no. 1) with a peripheral tumor of the left kidney was qualified for nephron-sparing surgery after a multidisciplinary tumor board meeting. NSS seemed possible because of the polar location and the small size of the tumor. The tumor size was 37 × 23 × 33 mm before and 18 × 20 × 23 mm after chemotherapy. An EinsteinVision 2.0 3D Camera System was used. The patient was placed in the decubitus position and 4 ports were placed (umbilicus – 12 mm, scope; middle epigastrium – 5 mm; left midabdomen – 5 mm; middle hypogastrium – 10 mm). A vessel loop was placed to secure control of the main renal artery and vein. The renal vein and artery to the upper pole of the kidney were controlled using Hem-O-Lock clips. The boundaries of the tumor were marked on the renal capsule under intraoperative US guidance. The upper pole of the kidney was resected using scissors (without arterial clamping – “zero-ischemia” resection). An extra rim of renal parenchyma was removed circumferentially to improve the radicality of the resection. The renal calyx and parenchyma were sutured using Vicryl 3-0 continuous suture and secured with TachoSil. The urinary leakage was observed postoperatively. Drainage of fluid (biochemically confirmed urine) was about 200 ml/day. Six days after laparoscopic NSS a cystoscopy with ureteral catheterization was done and urinary leakage was confirmed. The child required an open reoperation 8 days after LN. Partial ureteropelvic junction disruption (iatrogenic event during the first cystoscopy?) and leakage from the renal calyx were found. Ureteropelvic junction obstruction was diagnosed, although there was no renal pelvis dilatation on the initial imaging. The pyeloplasty was performed with double J stent placement to protect the anastomosis. An opened calyx was sutured using interrupted Vicryl 4-0 sutures. The further postoperative course was uneventful. The urinary leakage had resolved and the double J stent was removed after 2 months.
Five patients had a stage I and 3 had a stage II tumor. Seven patients had intermediate-risk and one had high-risk (blastemal) Wilms’ tumor histology. There were no local or distant relapses. All patients remained disease-free at a median follow-up of 71 months (range: 16–94 months). The pathological data and oncological outcomes are presented in Table II.
Table II
Pathological data and oncological outcome
Discussion
Although laparoscopic techniques are widely used in pediatric oncological surgery for various diseases, they are relatively rarely applied for renal tumors [2, 3].
One of the reasons is that not all renal tumors can be easily removed via laparoscopy. Usually the first symptom seen in patients with Wilms’ tumors is a large mass in the abdomen. In sizeable tumors the open approach remains the gold standard [1]. Even if laparoscopic resection for larger lesions have been reported, it should be avoided because of difficult tumor mobilization and the risk of its rupture and neoplastic cell spillage with the subsequent need for radiation therapy [4]. Moreover, large tumors require a formal laparotomy to remove the specimen [5]. The question arises whether it should still be considered minimally invasive surgery. On the other hand, it is difficult for surgeons to accumulate experience both in renal surgery (nephrectomy) and minimally invasive techniques. Thanks to the fact that neoadjuvant chemotherapy causes tumor shrinkage and encapsulation, rendering them more resistant to tumor spillage, laparoscopic nephrectomy has become a feasible option [1, 6, 7]. In accordance with the SIOP-RTSG 2016 UMBRELLA Protocol the acceptable indication for LN is a small, centrally located tumor without infiltration of extra-renal structures and thrombus in the renal vein or vena cava. Unilateral cases may also benefit from nephron-sparing surgery (NSS). NSS is acceptable in cases of: (1) a single, unilateral tumor restricted to one pole of the kidney or peripheral at mid-kidney, (2) tumor volume < 300 ml at diagnosis, (3) no preoperative rupture, (4) no intraluminal tumor in the renal pelvis, (5) no invasion of surrounding organs, (6) no tumor thrombus in the renal vein or vena cava, (7) excision can be performed with a safe oncological margin, (8) adequate kidney remnant (at least 66% of renal tissue should be spared after the resection) [1].
Duarte et al. first reported the use of laparoscopy for Wilms’ tumor. The authors described 2 cases of laparoscopic nephrectomy for unilateral WT [8]. Since then, several larger case series have been published [9–12]. Selected publications on laparoscopic nephrectomy and laparoscopic NSS for Wilms’ tumor are presented in Table III. One of the biggest series of LN for Wilms’ tumor came from Burnand et al. [9]. In this retrospective review 20 laparoscopic nephrectomies for WT were presented. Nine of 20 patients did not meet SIOP criteria for LN. No patients had an intraoperative tumor rupture, however. There were 2 conversions: one caused by problems with renal hilum visualization and the other caused by patients’ desaturation after partial resection of the diaphragm. There was one local recurrence. The number of sampled lymph nodes ranged from 0 to 10. No positive lymph nodes were identified.
Table III
Laparoscopic nephrectomy for Wilms’ tumor – selected publications
Adequate lymph node sampling (more than 6) is one of the most important aspects of LN sampling. It is necessary for accurate tumor staging and subsequent correct treatment. Data from SIOP 2001 presented by Warmann et al. raised the issue of poor lymph node sampling [6]. Lymph nodes were sampled in 15 of the 24 patients (63%). The number of harvested lymph nodes ranged from 0 to 11. Five patients had positive lymph nodes. Flores et al. reported 14 patients who underwent LN [7]. An estimate of 3 or 4 lymph nodes were sampled in each case. In the presented cohort, all children had an attempt of lymph node sampling and their number per pathology assessment ranged from 0 to 5. In other publications presented in Table III the lymph node sampling was also inadequate. Because most of the published reports come from individual clinical centers and are based on a relatively small number of patients, a negative prognostic impact of the inadequate sampling could not be calculated statistically [6]. Perhaps after confirmation of the relationship between lymph node sampling and oncological outcomes, it will be possible to extend the SIOP criteria.
Traditionally, the indications for NSS are: (1) bilateral WT, (2) unilateral WT with high risk of bilaterality (predisposing conditions such as Beckwith-Wiedemann syndrome), (3) WT in solitary kidney. In recent years, however, open NSS has been reported for children with unilateral WT without the above-mentioned indications [13]. Many publications indicate that NSS allows for kidney function preservation, which can positively affect the overall health status and quality of later life [14].
Moreover, both methods (radical nephrectomy and NSS) are comparable with regard to tumor rupture rates, recurrence rates and survival rates [13]. For these reasons, open nephrectomy is no longer considered the gold standard for unilateral, small WT (in selected cases, of course). On the other hand, laparoscopic NSS for malignant renal tumors remains controversial. The main difficulties are: (1) obtaining a negative resection margin, (2) avoidance of tumor spillage, (3) leaving the residual tumor, and (4) potentially increased chance of recurrence. Therefore, there are few publications on this method [15–17]. Laparoscopic NSS is technically very demanding and seems to be feasible and effective only when performed by a very experienced team. The patient presented in our series is a good illustration of complications that can occur after laparoscopic NSS. Fortunately, the final surgical and oncological outcome was very good.
Conclusions
This report demonstrates the feasibility of laparoscopic nephrectomy in children with Wilms’ tumors. But the feasibility of the operation is not the most important factor. Adherence to oncological principles is the key factor. Oncological safety should be the primary consideration. Therefore, patients should be very carefully selected for LN. Further publications on laparoscopic nephrectomy (and laparoscopic NSS) are needed to determine an optimal surgical approach to children with Wilms’ tumor and to define the role of lymph node sampling.