Introduction
Percutaneous nephrolithotomy (PCNL) is one of the standard surgical procedures for treatment of large renal and upper ureteral tract stones [1]. It has replaced the traditional open surgery due to its advantages of small trauma, high stone clearance rate, fewer complications and rapid postoperative recovery. However, it could lead to serious complications [2], such as intraoperative and postoperative bleeding, postoperative urinary tract infection, perirenal abscess and urine leakage. Misalignment of puncture location could also cause damage to surrounding organs or tissues such as colon and pleura.
The prone position (PP) is the classic position for PCNL, which provides a large puncture surface area and a wide space for instrument manipulation. However, PP would cause hemodynamic changes, ventilation dysfunction, and spinal cord and peripheral nerve injury [3]. Patients should first take the lithotomy position for placement of the ureteral catheter, and then change to PP for lithotripsy. In this way, the surgeons have to reposition and disinfect the operation area, which increases the workload and operation time. More importantly, a retrograde endoscopic procedure cannot be performed at the same time. If a double J stent needs to be placed from the lower urinary tract, the patient will need to be placed back in the lithotomy position again, which might lead to iatrogenic injury and longer operation time [4]. Furthermore, severe spine disease and ankylosing spondylitis are relative contraindications for prone PCNL. In addition, this position is not suitable for patients with severe cardiopulmonary disease and morbid obesity [5].
Valdivia et al. first reported their experience with PCNL in the supine position and described the advantages of this technique in 1987 [6]. The risk of cardiovascular and respiratory complications is lower in the supine position [7]. In addition, because the operation time is shorter, the anesthesia procedure is safer and requires less anesthetic. However, the supine position has its own disadvantages. First, it has a limited puncture surface area. Second, the depth between the skin and the kidney is deeper. Third, it is difficult to approach the upper renal calyx [8]. These factors motivated surgeons to improve PCNL positions, such as the Valdivia position and oblique supine position (OSP) [9]. The OSP could provide a wider puncture area, more space for nephroscopic manipulation like the PP, and no need to change position during the operation [10].
However, whether OSP is superior to PP remains controversial. Therefore, we performed this meta-analysis to systematically evaluate the current data comparing the efficacy and safety of PP and OSP during PCNL.
Aim
The objective of this meta-analysis was to investigate the efficacy and safety of OSP and PP in PCNL.
Material and methods
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses statement (PRISMA).
Search strategy
This systematic literature review was performed up to November 2022 using PubMed, Ovid and Web of Science databases to identify relevant studies comparing OSP versus PP during PCNL. The search strategy was: “(Percutaneous nephrolithotomy OR PCNL) AND (oblique supine position OR supine position OR modified Valdivia position) AND (prone position)”. We also manually screened the list of references from the related literature to identify other eligible studies.
Inclusion and exclusion criteria
The inclusion criteria were the comparative study of the OSP and PP during PCNL for adults aged 18 and above. The language of included studies was restricted to English. Exclusion criteria were non-comparative studies, studies on children, and studies without primary data (i.e. reviews, commentaries, conference abstracts).
Data extraction
Extraction of data was performed independently by two authors with a predefined data extraction form. Any discrepancy was resolved in consultation with the third author. They determined the relevance of the article by reading titles and abstracts. We compared preoperative demographic characteristics as well as perioperative and postoperative outcomes between the two procedures. The following information was extracted: baseline demographic characteristics (age, gender, BMI, and stone size), surgical outcomes (operation time, hemoglobin drop, hospitalization, stone-free rate) and complications (major complications are defined as Clavien-Dindo score ≥ 3).
Quality assessment
Two researchers independently evaluated the evidence level of included studies according to the Oxford Centre for Evidence-based Medicine. The risk of bias for the 5 RCTs was assessed. Only 1 study [11] was regarded as high risk because of using the unblind clinical trial (Figure 1). Any disagreements were settled by consensus with the third researcher.
Statistical analysis
A meta-analysis was performed using Cochrane Collaboration’s Review Manager (RevMan) 5.4 software (Cochrane Collaboration, Oxford, UK). For continuous outcomes, the weighted mean difference (WMD) with 95% confidence interval (CI) was used. For dichotomous outcomes, the odds ratio (OR) with a 95% confidence interval (CI) was calculated. According to the heterogeneity levels, the random effect or fixed effect model was used to calculate the summary risk estimates. Statistical heterogeneity was defined based on the Cochrane Q p value or I2 statistic. If p ≥ 0.1 or I2 < 50%, a fixed-effects model was used, while if p < 0.1 or I2 ≥ 50%, a random-effects model was used. When the p-value was less than 0.05, it was considered statistically significant. To assess publication bias, funnel plots were examined.
Results
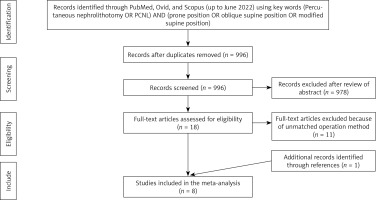
Overall, 8 articles [11–18] (5 randomized controlled trials [11, 13, 16–18] and 3 retrospective studies [12, 14, 15]) were included for further study, including 1185 patients (OSP = 634, PP = 551), as shown in Figure 2. The basic characteristics and quality assessment of included studies are summarized in Table I.
Table I
Basic characteristics of included studies
Figure 2
PRISMA flow diagram of the search strategy and identification of studies included in this study
All the eight studies including 1185 patients (OSP = 634, PP = 551) reported age, gender, BMI, and stone size. The results showed no statistically significant difference between OSP and PP for age (WMD = –0.95 years; 95% CI: –2.12 to 0.21; p = 0.11) and proportion of male patients (OR = 0.02; 95% CI: –0.03 to 0.08; p = 0.43), while OSP was associated with higher BMI (WMD = 0.66 kg/m2; 95% CI: 0.29 to 1.03; p = 0.0005) and smaller stone size (WMD = –0.01 cm, 95% CI: –0.18 to 0.02; p = 0.01) compared with PP (Figure 3).
Figure 3
Forest plots of demographic characteristics of oblique supine position (OSP) vs. prone position (PP) for percutaneous nephrolithotomy (PCNL)
SD – standard deviation, CI – confidence interval.

Seven studies including 985 patients (OSP = 534, PP = 451) reported the stone-free rate. Meta-analysis of these studies showed that there was no significant difference in stone-free rate between OSP and PP (OR = 1.32; 95% CI: 0.98 to 1.78; p = 0.07). All the eight studies including 1185 patients (OSP = 634, PP = 551) reported the operation time. The meta-analysis of our study showed that OSP was associated with shorter operation time compared with PP (WMD = –14 min; 95% CI: –27.00 to –1.00; p = 0.03). All the eight studies including 1185 patients (OSP = 634, PP = 551) reported the hospitalization. The meta-analysis of our study showed no significant difference between the OSP and PP (WMD = –5.99 h; 95% CI: –17.15 to 5.16; p = 0.00001). Six studies including 886 patients (OSP = 443, PP = 443) reported the hemoglobin drop. The results showed that OSP was associated with significantly less hemoglobin drop (WMD = –0.36 g/dl; 95% CI: –0.60 to –0.13; p = 0.003) (Figure 4).
Figure 4
Forest plots of surgical outcomes of oblique supine position (OSP) vs. prone position (PP) for percutaneous nephrolithotomy (PCNL)
SD – standard deviation, CI – confidence interval.

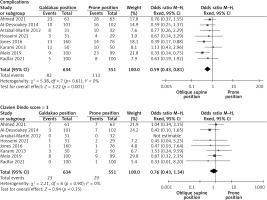
All the eight studies including 1185 patients (OSP = 634, PP = 551) reported complications. The results of this meta-analysis showed that OSP was associated with fewer overall complications (OR = 0.59; 95% CI: 0.43 to 0.81; p = 0.001). while there was no significant difference between OSP and PP with regard to Clavien-Dindo score ≥ 3 complications (OR = 0.76; 95% CI: 0.43 to 1.34; p = 0.35) (Figure 5) (Supplementary Figures S1 and S2).
Discussion
Renal stones are very common in urinary tract stones, and are more difficult to manage than stones in other locations. Currently, PCNL is the standard surgical procedure for the treatment of large renal stones, which has higher safety and efficacy than other procedures [19, 20].
PP is the classic position during PCNL, which provides a fixed renal anatomy. It is easier for surgeons to identify the renal anatomy and select the appropriate puncture point. However, PP requires repositioning from the lithotripsy to the prone position during surgery. In addition, a retrograde endoscopic procedure cannot be performed at the same time. Importantly, PP would cause hemodynamic changes and ventilation dysfunction. Compared with the PP, the risk of cardiovascular and respiratory complications is lower in the supine position. Some studies reported that the supine position was more suitable for obese patients [4, 5]. However, the puncture surface area and nephroscopic manipulation space are limited in the supine position, while the OSP could provide a wider puncture area, more space for manipulation of instruments, and no need to change position during the operation. More importantly, the OSP would reduce cardiovascular and respiratory risks and facilitate patient management for the anesthesiologist [7].
Many studies have reported that the PP was associated with a higher stone-free rate compared with the supine position [21–23]. This might be related to the following reasons. First, the PP could provide a larger surface area for renal puncture and a wider space for instrument manipulation [24]. Second, it is easier to approach the upper renal calyx in PP [25]. However, our study found that OSP was associated with a comparable stone-free rate with the PP. The reasons could be multifaceted. First, the OSP provided a larger flank exposure area for puncture, and a wider space between the last rib and the iliac crest during PCNL [26]. Second, the instruments could approach the upper renal calyx easily in OSP [8]. Third, the OSP could provide the possibility of simultaneous PCNL and ureteroscopic procedures, which would significantly improve the stone-free rate [27]. Fourth, the sheath angle of the OSP was horizontal or downward, which accelerated the evacuation of the stone fragment. Fifth, due to the lower angle of OSP, the lower renal perfusion pressure could prevent debris from migrating to the ureter and other calyces [28]. However, the smaller stone size in OSP might be the reason for a higher stone-free rate. Therefore, more randomized controlled studies are needed to confirm this result.
One of the most important advantages of OSP is that there is no need to change position during PCNL. Our meta-analysis showed significant shorter operation time in OSP, which was consistent with previous studies [29, 30]. This might be mainly due to the absence of repositioning and re-sterilization. In addition, the simultaneous PCNL ureteroscopic procedure was also associated with shorter operative time [4]. The smaller stone size in OSP could be associated with shorter operation time. However, BMI was larger in OSP, which would increase the surgical difficulty and prolong operation time. Therefore, the result of shorter operation time in OSP is reliable.
The hemoglobin drop reflects intraoperative blood loss. Although we found less blood loss in OSP, the difference of 0.36 g/dl was clinically meaningless. Kamphuis et al. demonstrated that blood loss was directly related to the dilatation size [31]. On the other hand, the shorter operation time might also be the reason for less intraoperative blood loss [32].
Complications are a very important indicator to evaluate the safety of a surgical procedure. We graded complications using the modified Clavien-Dindo score classification system [33–35]. Our results showed that OSP was associated with a superior overall complication rate and noninferior major complication rate. The reasons for these results might be as follows. First, PP might be associated with increased cardiovascular and respiratory risks, especially in morbidly obese patients [5]. Second, computed tomography (CT) showed that the colon was closer to the kidney in PP compared with OSP [36, 37], which resulted in a lower risk of colon injury in OSP [38]. Third, lower renal calyceal pressure seemed to reduce urinary tract infections and urine leakage.
There are several limitations in this study. First, the small sample size of included studies resulted in high heterogeneity. Second, three studies were retrospective, and the retrospective nature limited the reliability of the results. Third, the stone size and BMI were not consistent, which might have led to biased results. Fourth, the definition of stone-free rate was not consistent, which might have led to heterogeneity. Finally, the short follow-up time limited the assessment of long-term complications.
Conclusions
Compared with the PP, the OSP may be associated with non-inferior stone-free rate, blood loss, and hospitalization. Furthermore, the OSP might be superior in operative time and complications than PP during PCNL, especially for patients with severe cardiopulmonary disease, anesthesia risk and morbid obesity. More well-designed randomized controlled trials are required to validate these results.