Introduction
Globally 11–15% of pregnancies lead to spontaneous miscarriage during their first trimester. Diagnosis of miscarriage is preceded by surgical evacuation to reduce the subsequent risk of haemorrhage and gynaecological infection, which increase due to the retained products of conception (RPOC) [1, 2]. However, surgical management is associated with complications which, although rare, can cause serious morbidity such as infection, heavy bleeding, or uterine perforation may arise from surgical mode of intervention [3–6].
Expectant and pharmacological management are substitute treatment routes shown to be safer and more effective than the surgical method [7–9]. Pharmacological treatment of miscarriage has been proven to be beneficial in women with a missed miscarriage or empty sac [10–12]. However, misoprostol treatment can have adverse effects such as nausea, vomiting, and vaginal bleeding [13–17].
Expectant management is the natural strategy of passing out the retained tissues of gestation outside the hospital, which is an alternative option to the conventional treatment with medication or surgery. Expectant management is a suitable choice of treatment when the remaining product of conception is between 15–50 mm in the anterior-posterior diameter. Randomized control trial (RCT) studies have shown expectant care to report with success chances between 75 and 80%, especially in cases of incomplete miscarriage (79%) [1, 3].
However, vaginal bleeding and expulsion of pregnancy tissue is unpredictable in expectant care, thus resulting in many women still undergoing surgical management such as D and E. Expectant management also results in unplanned emergency surgery due to increased pain or bleeding with risk of infection, and abdominal pain [18].
Hence, the aim of the present research is to generate evidence regarding on the clinical safety and effectiveness of expectant care in the management of spontaneous miscarriage, compared to medical or surgical intervention during the 1st to 13th week of gestation.
Material and methods
Overview
This systematic review was conducted according to PRISMA [19] and was registered in Prospero (CRD42020154395). Based on the PICO strategy used to build the research question, the population involved women undergoing early spontaneous miscarriage/abortion in the first trimester; the intervention was the expectant management to induce abortion, and complete miscarriage success, haemorrhage, blood transfusion, fever, incomplete uterine evacuation, repeat uterine evacuation procedure, re-infection, post-operative complications, and re-hospitalization was the outcome of interest.
Thus, this systematic review sought to clarify the safety, efficacy, and side effects of expectant care on spontaneous miscarriage during the 1st to 13th weeks.
Eligibility
The review included original, free, full-text articles in English that estimated the safety and side effects of expectant management during first-trimester spontaneous miscarriage. Studies that did not include expectant management, as well as thesis papers, conference summaries, review articles, laboratory studies, and case series or reports were omitted from this systematic review.
Search strategy
The searches were performed in the following electronic databases: PubMed, Medline, Embase, and Cochrane including publications from January 2000 to December 2022. The terms used in the search are mentioned in Supplementary Table 1. The articles selected through these databases were de-duplicated, and the abstracts were read individually by 2 reviewers using Rayyan software [20]. Eligible articles underwent qualitative and quantitative analyses, according to data availability. Secondary articles were selected by cross-referencing the included articles.
Table 1
Demographic details of all the studies
Data extraction
Two researchers extracted data from the articles independently with the primary interest being the success of expectant management. A standardized MS Excel sheet was created to collect characteristics data from the studies such as year of publication, author, country, sample of participants, age, confounding factors, type of intervention, pre-outcomes, and outcomes including success rate, surgical treatment, Hb level, bleeding, abdominal pain, gestational sac or decidual tissue, fever, nausea, blood transfusion, readmission, and antibiotic requirement.
Assessment of risk of bias in the included studies
The bias assessment for the chosen studies was appraised with Joanna Briggs Institute (JBI) criteria [21, 22]. Two reviewers independently decided whether there was “high risk”, “low risk”, or “unclear risk” of bias. The risk of bias was ranked high when the study reached up to 49% of yes, moderate with 50–69% and low when it is above or equal to 70%.
Statistical analysis
The meta-analyses were accomplished with Review manager [23]. The odds ratio (OR) was considered as the measure of effect size to determine the complete abortion success rate for various interventions. When the tau square was zero. the fixed effects model was used, or else a random effects model was used to calculate the OR. The dependent variable was success rate, need for secondary evacuation, vaginal bleeding, and abdominal pain. The independent variables were medical vs. surgical intervention or medical vs. expectant management. If heterogeneity existed (I2 > 50%), a meta-regression was performed by relating study characteristics using SPSS [24].
Results
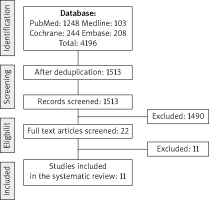
A total of 4196 indexed, peer-reviewed articles with the key search terms were identified and retrieved from the literature database, i.e. 1248 in PubMed, 103 in Medline, 208 in Embase, and 244 in Cochrane. 2683 studies were excluded because there were duplicate studies in the databases. After a complete evaluation, 11 articles [1–3, 17, 18, 25 –30] were included in this systematic review, as shown in Figure 1, comprising 2889 patients undergoing first-trimester miscarriage with 1709 undergoing expectant care for miscarriage in the first trimester. Seven studies [1–3, 17, 18, 25, 29] were considered for the meta-analysis.
Study characteristic
Five studies compared the expectant intervention with surgical management, and 3 studies compared the expectant intervention with medical management. The primary features of the studies are presented in Table 1. Interventions in the control arm varied in terms of medical or surgical intervention and the duration of the study. Complete abortion in most studies was well defined as expulsion of complete RPOC without surgical involvement. A complete abortion rate within 14 days was mostly mentioned. The systematic review revealed that the highest success through expectant management at 14 days was reported to vary between 99 and 47% [2, 29].
Risk of bias
Out of the 11 articles included, 6 had a randomized controlled trial design, while 5 had a quasi-controlled design. Only one RCT [17] study showed high bias, while 2 studies [25, 27] in the quasi-controlled study showed moderate bias. The results of the quality assessment using JBI criteria are mentioned in Supplementary Table S2.
Meta-analysis
Seven studies were included in the meta-analysis, and the details are shown in Table 2.
Table 2
Outcome variables of articles undergoing meta-analysis
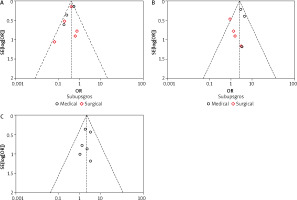
The results of meta-analysis for the outcomes are presented as forest plots in Figure 2. The present study compared the success rate of the intervention, and for the reported side effects, we could only compare the incidence of surgical evacuation required, abdominal pain, and vaginal bleeding in the meta-analysis. The forest plot indicated that the odds of success in expectant intervention was low when compared with surgical intervention (n = 1339, OR: 0.37 [0.28, 0.48], heterogeneity: χ2 = 5.71, df = 4 [p = 0.22]; I2 = 30%) and with medical management (n = 1025, OR: 0.47 [0.36, 0.61], heterogeneity: χ2 = 6.33, df = 2 [p = 0.04]; I2 = 68%). The main outcome of expectant management was need for surgical evacuation after follow-up visit (n = 1577, OR: 2.59 [1.88, 3.59], Heterogeneity: χ2 = 8.10, df = 6 (p = 0.23); I2 = 26%). The secondary outcomes evaluated were abdominal pain (OR: 1.44 [0.88, 2.36]), vaginal bleeding (OR: 2.19 [1.37, 3.49]), and infection (OR: 0.90 [0.53, 1.55]). The success rate and surgical evacuation showed moderate heterogenicity (I2 < 50) whereas the other the showed no heterogenicity.
Publication Bias
The funnel plot was symmetrical, as shown in Figure 3, indicating no publication bias, which was confirmed using Egger’s regression method (Egger test, p = 0.621).
Discussion
Miscarriage in the first trimester is a common factor, which could be due to advanced maternal age, stress, medical conditions such as T-shaped uterus, aneuploidies, and chronic endometritis. Studies have shown that these factors can lead to recurrent miscarriage and failure in procedures such as IVF treatment to conceive [31, 32]. Spontaneous miscarriage in women can affect them physically, mentally, and socially; hence, awareness regarding treatment options for miscarriage and their impact on general health is important [33]. This systematic review and meta-analysis represents the most comprehensive synthesis of data for expectant management for first trimester miscarriage when compared with medical or surgical interventions. Most of the literature is focused on the success rate of ultrasound findings at 2-week follow-up. It was found that expectant management is a better alternative in spontaneous miscarriage in the first 3 months of gestation, with a success rate as high as 99% after 2 weeks [29]. However, it was found that the achievement of complete evacuation of products of gestation was lower in patients undergoing expectant management when compared with surgical or medical interventions. This study supports the selection of expectant management as a potential substitute for surgery or pharmacological intervention because the probability of infection and abdominal pain were reported to be lower in expectant management.
Women electing this approach should be counselled factually about the chances of requiring additional surgical action, potential difficulties such as vaginal bleeding, and the availability of other management choices. Excessive vaginal bleeding and repeated requirement for blood transfusion due to it contribute towards hospital readmission and prolonged stay, which was assessed in the systematic review.
We assessed the risk of bias using the JBI criteria, which demonstrated low to moderate risk of bias in the majority of included studies. Most of the studies did not consider the confounding factors and did not conduct any statistical test to compare them. The majority of the studies were unable to give the sample size calculation. It was not possible to blind the participants or clinician in the studies, and the blinding of the outcome evaluator was unclear in some studies.
Conclusions
However, the findings of the present study have some limitations because most studies did not consider the dimension of retained tissues of gestation, the presence or absence of any clinical signs such as pain, bleeding, or infection before the treatment, and variations in treatment location and study duration. There were disparities in the ultrasound standards used to classify miscarriage (missed vs. incomplete) and the size of products of conception. Current evidence suggests that the side effects of expectant management is lower when compared to surgical or medical intervention. Future trials should consider women’s opinions and quality of life measures in conjunction with the clinical results to provide a wider dimension in the assessment of the efficiency and side effects of the intervention.