Introduction
Limb trauma (LT) refers to injuries and tissue damage occurring in the limbs (upper and lower extremities) due to external forces. Such trauma can result from various causes, including traffic accidents, accidental injuries, work-related incidents, and more. LT is among the major causes of significant disability and mortality worldwide, presenting a substantial challenge in the field of medicine [1, 2]. Encompassing a range of diverse diseases and injuries, LT includes but is not limited to the following categories. Fractures: Limb fractures are among the most common forms of LT, leading to bone fractures and dislocations, and joint dislocations, with the severity depending on the location and type of fracture [3, 4]. Soft tissue damage: LT can result in damage to soft tissues, including muscles, tendons, ligaments, and blood vessels. These injuries can give rise to complications such as bleeding, tissue ischemia, and necrosis. Nerve injury: LT may also involve nerve damage, encompassing nerve rupture, compression, or stretching, which can lead to sensory loss, impaired motor function, and neural deficits [5–7]. Currently, the clinical management of LT faces several challenges and dilemmas. Traditional treatment methods mainly include surgical repair, wound suturing, and conventional wet dressings. However, these methods exhibit limitations in certain cases. Firstly, significant bleeding and soft tissue swelling resulting from trauma can lead to surgical difficulties, increasing surgical risks. Secondly, wound infections are prone to occur during the wound healing process, prolonging recovery time and increasing patient discomfort. Moreover, the outcomes of treatment for certain severe LT cases are not always satisfactory, including joint stiffness, malformation healing, and functional impairments [8, 9].
Therefore, the quest for an innovative treatment approach to enhance the rehabilitation outcomes of LT patients is urgently needed. Vacuum sealing drainage (VSD) technique is an innovative technology widely applied in the field of trauma nursing. This technique is based on the principle of negative pressure, achieving wound edge closure and drainage fluid evacuation by applying negative pressure on the wound surface. VSD technique offers several key advantages: firstly, it effectively controls wound bleeding, reducing tissue oedema and exudate accumulation [10, 11]. Secondly, negative pressure promotes blood circulation, enhances oxygen supply within the wound, and stimulates tissue repair and regeneration. Furthermore, negative pressure can encourage wound contraction, facilitating wound healing [12]. However, despite achieving some success in trauma nursing, traditional VSD dressings exhibit certain limitations. VSD dressings consist of sponge material and a dressing covering the wound, with negative pressure applied to the wound surface through the dressing. Nevertheless, VSD dressings have the following limitations. Firstly, their sealability may not be optimal, leading to negative pressure leakage and contamination of the wound’s surrounding environment. Secondly, frequent changes of VSD dressings are required during application, adding complexity to nursing and patient discomfort. Additionally, the adsorption capacity and biocompatibility of VSD dressings also have certain limitations [13–15].
To overcome the limitations of VSD dressings and further enhance the effectiveness of trauma nursing, carbon nanomaterial (CNM) dressings have been introduced as a novel dressing material. CNM dressings possess a porous structure and a high specific surface area, which contribute to their excellent adsorption and release properties [16]. Moreover, carbon nanomaterials also exhibit advantages such as antibacterial properties, promotion of wound healing, and biocompatibility. In comparison to traditional dressing material, CNM dressings offer better sealability, effectively reducing negative pressure leakage and external contamination. Additionally, CNM dressings have a relatively longer application duration, which reduces the frequency of dressing changes and alleviates patient discomfort. Consequently, CNM dressings are regarded as a promising dressing option capable of enhancing the effectiveness of VSD technique in the nursing treatment of LT patients [17, 18].
This work employed a randomized controlled trial methodology to recruit 86 LT patients, aiming to assess the application effectiveness of VSD technique combined with CNM dressings in the nursing treatment of LT patients.
Aim
It aimed to provide the clinical community with more efficient and safer treatment options, contributing to the enhancement of treatment outcomes and rehabilitation processes for LT patients. Moreover, the results would offer a more reliable foundation for clinical practice, driving improvements in medical quality and advancements in patient care.
Material and methods
Research objects
A total of 86 LT patients admitted to the Dushu Lake Hospital Affiliated to Soochow University between March 2020 and February 2023 were selected and randomly enrolled into two groups: the Control (Ctrl) group and the Experimental (Exp) group, with 43 patients in each. Patients in the Ctrl group underwent conventional wound cleansing and drainage methods combined with regular dressing, while those in the Exp group received VSD combined with CNM dressings. Both groups received identical clinical nursing procedures.
Patients enrolled had to satisfy all the following conditions: patients aged between 18 and 65 years; and patients who were hospitalized due to LT and diagnosed with fractures, soft tissue injuries, tendon injuries, etc.
The patients had to be excluded if they experienced any of following conditions: pregnant or lactating women; patients with severe underlying conditions such as severe heart disease, liver or kidney failure; patients with immune system disorders, infectious diseases, tumours, and other serious complications; patients who have received treatment or surgical interventions related to the study; patients allergic or intolerant to carbon nanomaterials or VSD technique; and patients participating in other clinical trials; patients with cognitive impairment, language barriers, or communication difficulties who cannot effectively comply with study requirements.
In this work, the research objectives, procedures, precautions, and the legality of the study were all explained explicitly to the patients. Furthermore, the study objects agreed to sign an informed consent form with the consent of their family members when necessary. The implementation of this work had received approval from the Hospital Ethics Committee. Throughout the study period, assurance was given that no harm will be caused to the patients. Additionally, any obtained subject and private data were treated as confidential information, solely intended for research purposes and strictly prohibited from any other use.
Conventional wound cleansing and drainage methods
In the Ctrl group, prior to the commencement of surgery, patients receive appropriate anaesthesia based on clinical requirements. Patients were positioned on the operating table and underwent disinfection while being draped with sterile surgical drapes. The surgical process began with wound debridement, wherein blood, necrotic tissue, and contaminants around the wound were removed. This procedure involved irrigating the wound with sterile saline solution and employing surgical instruments to clear foreign objects and necrotic tissue from the wound area. Depending on the situation, the medical team may opt for fracture reduction, joint realignment, or nerve repair. Surgical interventions, such as fracture fixation or other procedures, may be conducted when deemed necessary. Following wound cleansing, a drainage tube was placed around the wound by the medical team. Typically made of soft plastic with a porous structure, the drainage tube guided exudate and blood from the wound area into a drainage bag. Subsequently, the medical team covered the area with sterile gauze. The dressing should cover the entire wound, secured with sterile bandages to ensure proper sealing. After the drainage tube placement and dressing application were complete, the surgical area underwent final cleansing, ensuring cleanliness and sterility around the wound. Sterile drapes and other items on the operating table were removed, and the surgical area was dressed with bandages.
VSD
In the Exp group, following wound cleansing, the medical team precisely applied CNM dressings (Manufacturer: Anxin Biotechnology Co., Ltd.) over the entire wound area, ensuring broad and continuous coverage. The unique structure and properties of CNM dressings provided enhanced wound vacuum sealing, along with additional biological activity to facilitate tissue repair and regeneration. Upon completion of CNM dressing application, a drainage tube was placed around the wound by the medical team and connected to a negative pressure device. Unlike conventional methods, the placement and connection of the drainage tube were carried out to ensure close contact with CNM dressings, maximizing the synergistic effects of the negative pressure drainage technique and CNM dressings. The negative pressure drainage device was tailored to the patient’s condition, with appropriate negative pressure levels adjusted. The negative pressure drainage device maintained a constant negative pressure on the wound, drainage tube, and CNM dressings, promoting wound healing and effectively collecting exudate and blood.
Nursing intervention
(1) Wound care: the nursing team should regularly inspect the wound, observe the progress of wound healing, and remain vigilant for any abnormalities such as signs of infection or increased exudate. Meanwhile, the nursing team could maintain the dryness and cleanliness of the wound to prevent the accumulation of debris and bacterial infection. Meanwhile, medical instructions for changing dressings should be strictly followed, ensuring proper adhesion and sterility, including the principles of aseptic technique to prevent cross-infection.
(2) Pain control: a multimodal pain management approach was applied based on the pain assessment results of the patients. This strategy encompassed medication therapy (analgesics), physical modalities (hot/cold packs, massage), and psychological support. Besides, the pain intensity and responses should be monitored, and the analgesic dosages and regimens were adjusted accordingly.
(3) Infection prevention and control: cross-infection should be prevented carefully by adhering rigorously to hand hygiene and aseptic techniques. Meanwhile, the medical/nursing team should regularly change dressings, promptly address and report any signs of wound infection, such as redness, swelling, and increased discharge. In addition, antibiotic treatment based on bacterial culture and sensitivity results was implemented, selecting appropriate antibiotics.
(4) Circulatory management: the circulatory status of patients was monitored, including peripheral pulses, skin temperature, and skin colour. Suitable measures should be ensured to promote blood circulation, such as elevating the affected limb, massage, or warm compresses. Furthermore, the medical/nursing team should monitor and correct the fluid balance of patients, ensuring adequate fluid circulation and tissue perfusion.
(5) Activity and functional recovery: the patients were encouraged to engage in active bedside activities, including joint movements, muscle contractions, and relaxations. The patients were provided with rehabilitation guidance and education, covering safety techniques and activity restrictions in daily life. Additionally, they were arranged with physical therapists to conduct rehabilitation training and functional recovery.
(6) Psychological support: emotional support and psychological assistance should be provided to help patients cope with psychological issues such as anxiety, fear, and depression. The patients were encouraged to participate in rehabilitation plans and activities to boost confidence and self-efficacy. Furthermore, support and education should be offered for family members, helping them understand the patient’s situation and offering assistance.
Observation indicators
(1) Wound healing assessment: evaluation criteria were based on clinical presentation and tissue healing status.
Satisfactory: ① absence or reduced amount of exudate around the wound, no continuous exudate or blood oozing; ② no redness, swelling, local warmth, pus discharge, or increased secretion around the wound; ③ intact skin adhesion at the wound edges, formation of granulation tissue within the wound, relatively flat and smooth healing; and ④ minimal or no apparent pain during rest or activity, or only slight discomfort.
Suboptimal: Ŕ continuous exudate, pus discharge, or increased secretion around the wound; ② redness, swelling, local warmth around the wound, possibly with pus discharge or increased secretion; ③ incomplete adhesion or separation at the wound edges, potential exposure of deep tissues; and ④ noticeable pain during rest or activity, possibly aggravated pain or tenderness.
(2) Pain intensity: the visual analogue scale (VAS) was employed as a pain assessment tool to evaluate the pain intensity of patients. The VAS score involved patients marking their perceived pain intensity on a straight line, which was a 10-centimeter line, with 0 representing no pain and 10 indicating the most severe pain. Assessment criteria were as follows: 0: no pain; 1–3: mild pain, tolerable; 4–6: moderate pain, affecting activity but still bearable; 7–9: severe pain, significantly affecting activity and difficult to bear; and 10: most severe pain, unbearable.
(3) IOC: haemorrhage: postoperative bleeding situations were documented; wound infection: occurrence of wound infection following treatment was assessed, skin damage: instances of skin damage that arose during treatment were recorded, encompassing conditions like skin ulcers, rashes, etc.
(4) Functional recovery: LFR of the two groups of patients was compared using a self-developed LFR scale, assessed as excellent, good, or poor.
Excellent: Ŕ no or slight pain, capable of performing daily activities without restriction; ② joint mobility considerably restored, approaching a normal range, enabling completion of daily activities and light exercises; ③ noticeable increase in muscle strength, capable of withstanding higher loads and resistance, performing higher-intensity activities; and ④ successful restoration of functionality, capable of executing complex movements and activities, such as climbing stairs, jumping, and running.
Good: Ŕ pain ranging from mild to moderate, bearable but discomforting, slight limitations in daily activities; ② joint mobility relatively normal, albeit potentially slightly restricted, capable of completing daily activities and light exercises; ③ partial recovery of muscle strength, though still somewhat deficient, capable of performing general daily activities; and ④ moderate functional recovery, able to undertake most daily activities, yet possibly encountering some difficulties in certain complex movements and exercises.
Poor: Ŕ pain ranging from moderate to severe, limited mobility, adversely affecting daily activities; ② markedly restricted joint mobility, unable to reach a normal range, severely impacting daily activities and exercises; ③subpar muscle strength recovery, diminished muscle control, unable to perform certain daily activities; ④ inferior functional recovery, incapable of executing most daily activities, losing a certain level of work and life capabilities.
(5) Patient satisfaction assessment: patient satisfaction with treatment outcomes and nursing services was evaluated using a department-developed questionnaire and was calculated with (Number of Very Satisfied + Number of Somewhat Satisfied)/Total Survey Participants × 100%.
Statistical analysis
SPSS 20.0 was employed to analyse the data. Continuous variables were presented as mean ± standard deviation, and intergroup comparisons were conducted using paired-sample t-tests. Categorical data were represented as cases (%) and intergroup comparisons were performed using the χ2 test. P < 0.05 indicated a statistical significance.
Results
General characteristics of patients
The general characteristics of patients were presented in Table 1. No great differences were observed between patients in Ctrl and Exp groups in terms of age, gender, affected side, and type of injury (p > 0.05), indicating a comparability.
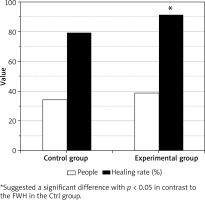
Comparison of FWH rates of patients in different groups
As illustrated in Figure 1, there were 34 (79.06%) cases of FWH in the Ctrl group, and 39 (90.69%) cases in the Exp group. It indicated that the FWH rate in the Exp group was sharply higher and exhibited a significant difference compared to that in the Ctrl group (p < 0.05).
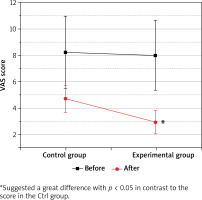
Comparison on preoperative and postoperative pain of patients
As depicted in Figure 2, prior to surgery, no considerable differences in VAS scores were observed between patients in the Ctrl and Exp groups. After the operation, VAS scores in the Ctrl group decreased to 4.72 ±1.03 points, whereas they decreased to 2.95 ±0.88 points in the Exp group. The data revealed that the VAS scores of patients in the Exp group were much lower than those in the Ctrl group, presenting a statistically significant difference (p < 0.05).
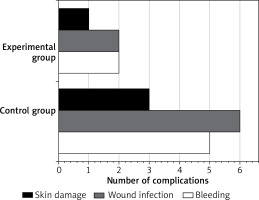
Comparison on IOC of patients after different nursing interventions
As illustrated in Figure 3, in the Ctrl group, there were 5 cases of bleeding, 6 cases of wound infection, and 3 cases of skin damage. In contrast, there were 2 cases of bleeding, 2 cases of wound infection, and 1 case of skin damage in the Exp group. As a result, the IOC in the Exp group (11.62%) was much lower and presented a significant difference compared to 32.55% in the Ctrl group (p < 0.05).
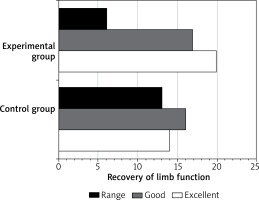
Comparison on LFR of patients
As explicated in Figure 4, in the Ctrl group, there were 14 cases of good LFR, 16 cases of fair LFR, and 13 cases of poor LFR. In the Exp group, there were 20 cases of good LFR, 17 cases of fair LFR, and 6 cases of poor LFR. The overall LFR rate in the Exp group was greatly different (higher) than that in the Ctrl group, with a value of 86.04% vs 69.76%, holding a statistical significance (p < 0.05).
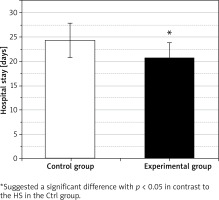
Comparison on HS of patients receiving different nursing interventions
As depicted in Figure 5, the average HS for patients in the Ctrl group was 24.32 ±3.56 days, while it was 20.71 ±3.23 days in the Exp group. It showed that patients in the Exp group stayed for a short period in hospital in contrast to those in the Ctrl group, and this difference was significant (p < 0.05).
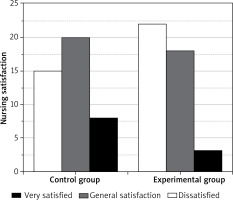
Nursing satisfaction of patients
As illustrated in Figure 6, in terms of clinical nursing, 15 patients in the Ctrl group were very satisfied, 20 were moderately satisfied, and 8 were dissatisfied. In the Exp group, 22 patients were very satisfied, 18 were moderately satisfied, and 3 were dissatisfied. The above data suggested that nursing satisfaction rate in the Exp group (93.02%, 40/43) was higher, which was significantly different from that in the Ctrl group (81.39%, 35/43) (p < 0.05).
Discussion
Currently, LT stands as one of the prevalent clinical conditions, exerting a vital impact on quality of life and functional recovery of patients. Traditional treatment approaches encompass routine wound debridement and the application of regular dressing. However, these methods have exhibited limitations and challenges in certain scenarios. In pursuit of more effective therapeutic strategies and elevated treatment outcomes for enhanced patient rehabilitation, this study was conducted with the aim to assess the application effects of VSD technique combined with CNM dressings in the nursing treatment of LT patients. By comparing with conventional methods, the study seeks to determine whether the combination of VSD technique and CNM dressings can enhance the FWH rate, reduce the incidence of complications, alleviate postoperative pain, promote faster LFR, and shorten HS of patients. Additionally, this work placed attention on the nursing satisfaction of patients in the Exp group to evaluate the overall impact of this technique on the nursing experience of patients. Through these experiments, this work aspired to provide the clinical community with more effective and secure treatment options, contributing to the improvement of treatment outcomes and rehabilitation progress for LT patients. Results in this work were expected to offer more dependable evidence for clinical practice, thereby advancing the quality of healthcare and enhancing the nursing experience for patients.
Based on the experimental results, the FWH rate of patients in the Exp group (90.69%) was higher than that of the Ctrl group (79.06%), showing a significant difference with p < 0.05. The adoption of VSD technique combined with CNM dressings in the Exp group potentially provided superior wound vacuum sealing and biological activity, thereby promoting wound healing and repair. The unique structure and properties of CNM dressings could facilitate tissue regeneration and repair, potentially accelerating the wound healing process. Moreover, the patients in the Exp group received meticulous and professional nursing care, including wound cleansing and dressing changes, demonstrating the high quality of the nursing team’s expertise. The experimental results revealed that postoperative VAS scores in the Ctrl group (4.72 ±1.03) were higher than those in the Exp group (2.95 ±0.88), presenting a significant difference with p < 0.05. The combination of VSD technique and CNM dressings may contribute to reducing the severity of postoperative pain and promoting its alleviation. The bioactive components within CNM dressings could exert anti-inflammatory and analgesic effects on the surrounding tissues, thus mitigating postoperative pain. Negative pressure drainage technique effectively removed wound exudate and blood, reducing the accumulation of wound irritants and subsequently alleviating postoperative pain. Zhang et al. [19], in a retrospective analysis, explored the role of VSD in improving treatment outcomes, reducing postoperative infections, and preventing lower limb deep vein thrombosis in orthopaedic trauma patients. They divided patients into the Ctrl group (conventional dressing changes) and the Exp group (VSD treatment). The results demonstrated that the occurrence of postoperative infections and lower limb vein thrombosis was lower in the Exp group compared to the Ctrl group. Additionally, the Exp group had shortened operative and hospitalization times, accelerated wound healing, and reduced postoperative infections and deep vein thrombosis. These findings align with the results of the current study.
Furthermore, Shi et al. [20] investigated the application value of VSD combined with antimicrobial biofilm hydraulic fibre dressings in wound healing after severe acute pancreatitis surgery. Patients in the Ctrl group received VSD treatment, while those in the Exp group received VSD combined with antimicrobial biofilm hydraulic fibre dressings. The postoperative recovery efficiency, preoperative and postoperative wound area reduction rates, and incidence of wound-related adverse reactions were compared between the two groups. The results demonstrated significant application effectiveness of VSD combined with antimicrobial biofilm hydraulic fibre dressings in postoperative wound healing. This approach improved wound healing efficiency, reduced inflammatory markers, and lowered the incidence of adverse reactions. While further research is needed to determine its impact on infection and inflammation prevention, this treatment method exhibits promising prospects for clinical application. The findings of this study are consistent with these results. Based on the experimental results, the IOC (32.55%) of the Ctrl group was higher, which was significantly different from that in the Exp group (11.62%). VSD technique may reduce the accumulation of wound exudate and blood, thus reducing the risk of bleeding and infection. CNM dressings possess antimicrobial properties that can inhibit wound infection. The overall LFR rate (86.04%) of the Exp group was much higher compared to that of the Ctrl group (69.76%), and p < 0.05 was marked. VSD technique may contribute to promoting wound healing and tissue repair, thereby accelerating limb function recovery. CNM dressings may play a role in promoting tissue repair and regeneration through their bioactive components, aiding in limb function recovery. Additionally, the nursing care in the Exp group included rehabilitation guidance and functional recovery training, thereby enhancing the effectiveness of LFR. Moreover, the average HS of the Exp group (20.71 ±3.23 days) was significantly shorter than that of the Ctrl group (24.32 ±3.56 days) (p < 0.05). The faster wound healing and lower IOC in the Exp group resulted in reduced hospitalization time. The use of advanced treatment techniques and dressings in the Exp group provided better wound management and nursing care, thus contributing to higher nursing satisfaction among patients. The experimental results disclosed that nursing satisfaction (93.02%) in the Exp group was significantly higher which was 81.39% in the Ctrl group. This might be attributed to the positive experience and feedback on treatment effectiveness from Exp group patients, contributing to increased nursing satisfaction.
Yuan et al. [21] also conducted a relevant study, involving continuous treatment of 83 LT patients. Based on the treatment methods, patients were divided into the VSD group and the traditional compression dressing group. After surgical reduction, the skin was sutured using either VSD or traditional dressings, and the outcome was evaluated based on the percentage of skin grafting. The results indicated that the efficacy of VSD and traditional dressing treatments for LT was comparable. However, with an increase in hospitalization costs, VSD technique might carry a higher risk of adverse outcomes. This aligns with the results of the Exp group in this study, where the advantages of VSD technique combined with CNM dressings were more pronounced, further supporting the application of this approach in LT patients’ nursing treatment. Nevertheless, they also mentioned the potential risks of adverse outcomes and higher hospitalization costs associated with VSD technique. This highlights the need to acknowledge the higher implementation and equipment costs of VSD technique, which could add to the economic burden of patients. Therefore, in resource-limited settings, especially in rural hospitals, traditional dressing methods still possess certain advantages and feasibility. In summary, the results of this study support the application of VSD technique combined with CNM dressings in the nursing treatment of LT patients, demonstrating favourable clinical outcomes and patient satisfaction. However, we should also take into consideration the cost and feasibility limitations of this technique. Future research could further explore ways to reduce the cost of VSD technique and compare the effects of different treatment methods in various medical settings to provide more comprehensive and accurate clinical guidance. When selecting an appropriate treatment method, a comprehensive consideration of patients’ individual conditions, resource limitations, and medical environment is necessary to achieve optimal treatment outcomes and cost-effectiveness.
Conclusions
Results of this work indicated that in the nursing treatment of LT patients, the combination of VSD technique and CNM dressings had significant advantages over the conventional wound debridement method combined with regular dressing. It demonstrated favourable outcomes in terms of FWH rate, IOC, postoperative pain scores, LFR, HS, and nursing satisfaction. However, this work also was subjected to certain limitations. Firstly, the sample size was relatively small, which may introduce sample selection bias, and further expansion of the sample size was needed to enhance the study reliability. Secondly, this work only observed short-term treatment effects, while long-term efficacy and prognosis require further investigation. Additionally, this work did not conduct a detailed analysis of factors such as patients’ underlying diseases and surgical technique proficiency, which could potentially influence the results. Future research could further explore the application of VSD technique combined with CNM dressings in the nursing treatment of LT patients, considering additional evaluation indicators including pain management and quality of life to comprehensively assess the technique’s effects. In summary, the combination of VSD technique and CNM dressings shows potential advantages in the nursing treatment of LT patients. However, larger-scale, long-term follow-up, and multi-centre studies would be needed to validate its efficacy. Further research can delve into the mechanism of this technique, optimize treatment protocols, and compare it with other treatment methods to provide more reliable evidence for clinical practice, thereby promoting the treatment outcomes and rehabilitation process of LT patients.