Purpose
After breast cancer, colorectal cancer, and lung cancer, cervical cancer is the fourth most common cancer in women in the world. Approximately 604,127 new cases of cervical cancer and 341,831 deaths from this disease occurred in 2020 worldwide [1]. Low- and middle-income countries accounted for 90% of the incidence and mortality [2]. India accounts for nearly one-fifth of the global cervical cancer cases, with 2.01% cumulative risk of incidence and 1.3% cumulative risk of death from this disease [3].
Current standard of treatment for locally advanced carcinoma cervix is external beam radiotherapy (EBRT) with concurrent chemotherapy followed by brachytherapy (BT) [4], the latter contributing to excellent local control to a total EQD2 of 85-90 Gy equally divided between EBRT and brachytherapy [5].
Intra-cavitary brachytherapy (ICBT) and interstitial brachytherapy (ISBT) are two most common types of BT following EBRT. A comparatively lesser implemented third type of brachytherapy, free-hand technique (intra-cavitary + interstitial, IC + IS) is a combination of intra-cavitary brachytherapy and placement of needles, without the use of a template in a selected group of patients. In view of an increased patient load to up to 6-8 cervix brachytherapy patients per week, and more than 2/3rd of patients with locally advanced stages, with limited number of ISBT templates, we implemented IC + IS technique in selected sub-set of patients in order to reduce waiting period.
There are few studies describing this technique in the literature. Therefore, in the current study, we dosimetrically compared ICBT with free-hand technique (IC + IS).
Material and methods
After obtaining ethical clearance and informed consent from patients, this prospective dosimetric study was conducted among 27 histologically proven locally advanced carcinoma cervix patients. All of them received EBRT to a dose of 45 Gy in 25 fractions, over 5 weeks using three dimensional conformal radiotherapy (3D-CRT), along with 4-6 cycles of concurrent weekly cisplatin/carboplatin chemotherapy [6].
Brachytherapy was applied under combined spinal epidural anesthesia within 10 days following completion of EBRT. Apart from the central disease, patients with more than medial 1/3rd parametrial residual disease but not extending up to lateral pelvic wall at brachytherapy were considered for free-hand technique. Based on findings from examination under anesthesia (EUA), the number of needles to be placed was decided. IC + IS technique was done following catheterization of the bladder.
Free-hand (IC + IS) technique
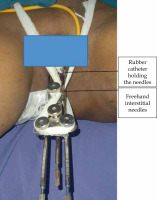
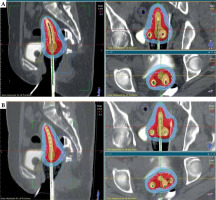
Figure 1 shows free-hand brachytherapy technique with the position of needles and intra-cavitary applicators. A sterile plastic suction catheter was cut appropriately to obtain two small pieces of ~4 cm in length each, to accommodate 2-3 needles, 1 cm apart. Using a sterile marker pen, 3 points were marked on these suction tubes 1 centimeter apart. Based on the decision, needles were inserted at the marked points on the suction catheter. One piece of this catheter was fixed at 4 cm behind the tip of needles, and the other piece at the distal end of needles to stabilize the applicators. Based on pre-EBRT MRI and EUA (evaluation under anesthesia) findings, the length of needles inserted during brachytherapy was decided. Since all our patients had combined spinal-epidural anesthesia, during CT simulation, the position of needles was verified and corrected if required. The distance between the needles was kept at minimum of 1 cm and less than 2 cm. If anatomy was favorable, 3 needles were inserted, whereas in narrow or conical vagina, 2 needles were inserted. Figure 2 demonstrates the alignment and position of needles with respect to ICBT applicator. Tandem of appropriate length was inserted into the uterine cavity. Following insertion of the central tandem, the needles were inserted at the respective side of the fornix and two ovoids on either side of the tandem medially to the needles. After securing the applicators in place, careful vaginal packing was done using betadine-soaked gauze to displace the bladder and rectum, and also to augment the applicator’s stability. Rectal tube was placed for instilling diluted contrast in the rectum during simulation. Computerized tomography (CT) simulation was performed with 2.5 mm slice thickness. For the bladder and rectum delineation, contrast mixed with normal saline (NS) was instilled. CT images were transferred to HDR Plus treatment planning system (TPS), version 3.0.8.
Brachytherapy planning
High-risk clinical target volume (CTVHR) was delineated based on EUA findings at brachytherapy and pre-EBRT MRI that defined CTVIR, or a 1 cm margin around HR-CTVCT according to Viswanathan et al. guidelines [7]. Therefore, one centimeter margin to CTVHR formed intermediate-risk clinical target volume (CTVIR). According to our department protocol, the bladder, rectum, and sigmoid were contoured, and constraints were assigned.
Multiplanar reconstruction view was utilized for applicator digitization. Surface control points were created on CTVHR and OARs. Forward treatment plan was generated in HDR Plus v. 3.0.8 TPS using Task Group 43 (TG-43) algorithm [8, 9]. Dose constraints were 6.5 Gy to CTVHR, 5 Gy to 2 cc bladder, and 4 Gy to 2 cc rectum and sigmoid colon. Re-shaper tool was applied for optimization to achieve better CTVHR coverage and minimize dose to OARs.
Needle dwell positions were activated inside the CTVHR volume. Two unique plans were created for each patient. The ICBT plan was devised by deactivating free-hand needles and planning with the central tandem and two ovoids only, whereas the free-hand plan was generated by including free-hand needles with the central tandem and ovoids. The target volume coverage of high-risk clinical target volume (HR-CTV) and OARs (organs at risk) dose of the bladder, rectum, and sigmoid were compared between these two plans. A dose of 6.5 Gy per fraction to a total of four fractions was prescribed to HR-CTV. Dosimetric comparison between these two plans was done by analyzing dose volume histograms (DVH) and documenting dose to HR-CTV using V90 (%), V100 (%), V150 (%), V200 (%), D90 (Gy), D98 (Gy), D100 (Gy), and D2cc for OARs.
All fractions were delivered over two days, with minimum of six hours gap between two fractions, in a single session [10]. All patients were treated using BEBIG Multisource cobalt-60 (60Co) HDR afterloader (model A.1.86). EQD2 for 2 cm3 of the bladder, rectum, sigmoid, D90, and D98 were calculated for both the plans using the following formula:
BED = nd (1 + d/α/β) and EQD2 = BED/[1 + (2/α/β)],
where n is the number of fractions and d is the dose per fraction. The α/β ratio was considered as 3 for the normal tissue and 10 for the tumor.
Statistical analysis
Sample size was calculated based on a previous study conducted by Oike et al. [11], where considering D90% coverage in IC/IS plan, it was found to be 118 ±22%. In the present study, considering the power of 80%, relative precision of 7%, and confidence level of 95%, minimum sample size was calculated to be 27. Statistical software, SPSS Inc., version 18.0 was used for data analysis, with p-value of < 0.05 considered statistically significant. Qualitative variables were presented as frequency and percentage. All quantitative variables were analyzed using mean and standard deviation parameters. With paired t-test, different doses were compared and statistical significance was determined.
Results
Patient characteristics are summarized in Table 1. Our study included a total of 27 patients, with a mean age of 55 years, ranging between 43 and 74 years. All the patients received EBRT to a dose of 45 Gy in 25 fractions using 3D-CRT technique. All brachytherapy plans were optimized to 6.5 Gy per fraction to a total of 4 fractions in this dosimetric study. The number of needles inserted was influenced by the extent of residual parametrial disease and vaginal anatomy. A total of 79 needles were used in the study, ranging from a minimum of 2 needles to maximum of 6 needles for a patient.
Table 1
Patient characteristics and frequency
DVH parameters
The HR-CTV of V90 and V100 showed statistical significance with p-value of < 0.0001, favoring the free-hand technique; however, it did not show significant difference for V150 and V200. Upon comparison of D90, D98, and D100, the mean values in the ICBT plan were 5.26 Gy, 3.72 Gy, and 2.61 Gy, while in the free-hand plan, the mean values were 6.28 Gy, 4.91 Gy, and 3.62 Gy, respectively, with statistically significant p-value of < 0.0001 (Table 2). The calculation of EQD2 values led to the following results. In the free-hand plan, EQD2 values of D90, D98, and D100 were 78.47 Gy, 68.85 Gy, and 60.81 Gy, respectively. However, the corresponding parameters in the ICBT plan were 71.07 Gy, 61.50 Gy, and 55.35 Gy, respectively, with all free-hand values being statistically significant (p ≤ 0.0001).
Table 2
Comparison of mean dose of high-risk clinical target volume (HR-CTV) between intra-cavitary brachytherapy (ICBT) and free-hand plans
OARs dose
Table 3 demonstrates comparison of OARs doses with ICBT and free-hand techniques, with no statistical difference between these two methods. The mean EQD2 for the bladder D2cc was 70.08 Gy and 71.28 Gy for the ICBT and free-hand plans, respectively, with no statistical significance (p = 0.92).
Table 3
Mean dose of organs at risk in intra- cavitary brachytherapy (ICBT) and free-hand technique
| D2cc | Mean dose (Gy) | p-value | |
|---|---|---|---|
| ICBT | Free-hand | ||
| Bladder | 4.46 ±0.64 | 4.59 ±0.57 | 0.08 |
| Rectum | 3.90 ±0.53 | 3.98 ±0.51 | 0.15 |
| Sigmoid colon | 2.67 ±0.92 | 2.77 ±0.96 | 0.22 |
The EQD2 for the rectum was 64.94 Gy in the ICBT technique vs. 65.57 Gy in the free-hand technique, and was statistically non-significant (p = 0.18). Similarly, EQD2 for the sigmoid was 55.95 Gy in the ICBT plan and 56.59 Gy in the free-hand plan, with a p-value of 0.16.
Discussion
It has been well-established that there is a significant correlation between dose to target volume and local control in carcinoma cervix [12]. The need for ISBT arises when there is more than medial 1/3rd parametrium involvement. However, ISBT is invasive, tedious, resource-intensive, time-consuming procedure, causing discomfort for the patient. In order to overcome these, a combination of intra-cavitary and interstitial brachytherapy was implemented. The current prospective dosimetric study compared intra-cavitary and free-hand brachytherapy techniques in patients with locally advanced carcinoma cervix. Similar dosimetric studies comparing ICBT with combined IC + IS brachytherapy technique by generating 2 separate plans for each patient have been conducted, including Akbarov et al. [13], Qu et al. [14], Tambaş [15], and Nomden et al. [16], using IC/IS applicators. However, among the combined IC/IS approaches, only a few authors, such as Yoshio et al. [17], Liu et al. [18], Wang et al. [19], and Bajwa et al. [20] have correlated DVH parameters between ICBT and free-hand IC + IS techniques.
Assessment of parametria
In the present study, the decision about the number of needles and their positions was done according to EUA findings during brachytherapy, whereas Bajwa et al. [20] and Liu et al. [18] used pre-brachytherapy MR images. This is probably due to the limited availability of MRI facility in Indian setting. Moreover, a thorough pelvic examination under anesthesia is sufficient to decide about the applicators and needle placement [21].
Free-hand technique
Number of needles
A total of 79 needles were used in our study. It ranged from a minimum of 2 needles to maximum of 6 needles per patient. The number of needles were decided based on the parametrial disease – whether unilateral or bilateral, similar to Yoshio et al. study [17]. However, the numbers of needles used for each patient in Wang et al. [19] and Liu et al. [18] studies were ranging from 4 to 7 and 6.9 ±1.4, respectively, which were slightly higher compared with those in our study. This is attributable to the use of image guidance during the procedures.
Free-hand needle approach
The free-hand needle insertion can be performed either trans-vaginally, entering through the fornices into the involved parametrium, or through transperineal approach without a template. However, in Liu et al. [18] study, the needles were inserted at 2, 4, 8, and 10 o’clock positions, without using ovoids, while Bajwa et al. [20] reported using transperineal approach. In our study, we inserted the needles through the vaginal fornices based on the involved side before the insertion of vaginal ovoids.
Image guidance
Most of the studies used image guidance in the form of ultrasound, CT scan, and C-arm CT for the free-hand interstitial needle insertion (Table 4). CT image guidance was applied by Liu et al. [18], whereas Wang et al. [19] along with CT image guidance, used rectal contrast to delineate better while inserting the needles. Trans-rectal ultrasound and fluoroscopy were applied in Yoshio et al. [17] study. However, Bajwa et al. [20] started their study with the use of C-arm guidance, which did not result in desired implant geometry in the first two cases, as it was a learning curve for them. But subsequently, with C-arm itself, implant geometry was achieved. Image guidance facilitated the usage of a greater number of needles inserted into the involved parametrium with desired implant geometry, achieving adequate depth and minimizing the implant complications.
Table 4
Comparison of D90 (Gy) EQD2 values among various studies
In our study, the free-hand needle insertion took place without any image guidance due to the lack of resources. The position of needles were sufficient and satisfactory, and there were no needle-related complications, such as bowel injury, confirmed by brachytherapy CT simulation scans (Figure 3).
Depth of insertion
The depth of insertion of the needles in our study was uniformly kept at 4 cm from the vaginal fornix, as we did not use image guidance for the needle insertion. There was no procedure-related complications, such as bladder or bowel perforations, due to uniform depth of insertion. However, in a study by Qu et al. [14], the mean depth of insertion of the distal parametrial needle was 6.52 ±2.8 cm, as it was done under ultrasound guidance. Moreover, Liu et al. [18] demonstrated that 5 of 52 patients (9.6%) suffered intestinal injury; therefore, these needles were not loaded.
Fixation of free-hand needles
In our study, the free-hand needles were fixed using suction catheters, which did not require suturing (Figures 1 and 2). The applicators were stabilized with the help of the gauze tied to the abdomen. In a study by Wang et al. [19], the needles were fixed using a button stopper that was sutured to the perineum. Bajwa et al. [20] employed sterile pieces of thermoplastic cast and standard interstitial needle screws to stabilize the needles through the holes in aquaplast, which were sutured to the perineum.
DVH parameters
The free-hand and ICBT plans had a mean V100 values of 89.06% and 81.51% (p ≤ 0.0001), respectively. Interestingly, no other known free-hand study had compared V90% values. The V100 (%) values in Yoshio et al. [17] study were slightly higher than that of the current study (96 ±3.7%). This may be due to the transperineal approach of the needle insertion to cover the entire residual parametrial disease.
However, V150% and V200% values of both the plans were not significant in our study, with p-values of 0.06 and 0.62, respectively, which is in line with Yoshio et al. [17] research. The EQD2 values of D90, D98, and D100 showed statistical significance in the ICBT plan with 71.07 Gy, 61.50 Gy, and 55.35 Gy, respectively, while that of the free-hand plan were 78.47 Gy, 68.85 Gy, and 60.81 Gy, respectively (p ≤ 0.0001).
Liu et al. [18] achieved a mean D90 of 88.1 ±3.3 Gy as a result of placement of oblique needles, i.e., free-hand needle inserted from the left side of the introitus to the right parametrium and vice versa under image guidance. In a study by Bajwa et al. [20], the mean D90 was 82 Gy, slightly higher than in our study (Table 4). This may be due to the fact that Bajwa et al. inserted transperineal needles under image guidance, which helped to achieve a bit higher D90 value than that achieved in the present study.
As a department protocol, we tried to accomplish a maximum EQD2 of 80 Gy to HR-CTV keeping OARs doses well within 75 Gy EQD2 for the bladder and 65 Gy EQD2 for the rectum. This is based on Viswanathan et al. [22] study reporting that with CT-based planning, there is an over-estimation of the width of HR-CTV as compared with MRI-based planning [23, 24]. This leads to an increased volume receiving prescription dose. Hence, the D90 value in our study is relatively smaller compared with other studies. This is supported by our department data, [23, 25], showing a local control rate of 87.14% at 2 years in locally advanced carcinoma cervix patients.
In our study, in the free-hand and ICBT plans, the D2cc values of the bladder, rectum, and sigmoid were 4.59 Gy, 3.98 Gy, and 2.77 Gy, and 4.46 Gy, 3.90 Gy, and 2.67 Gy, respectively, with no statistical significance (p = 0.08, 0.15, 0.2, respectively) as the needles were placed in the parametrium laterally. In terms of EQD2, the D2cc values of the bladder, rectum, and sigmoid were 70.08 Gy, 64.94 Gy, and 55.95 Gy in the ICBT plan, respectively. Similarly, the D2cc EQD2 values of the bladder, rectum, and sigmoid were 71.28 Gy, 65.57 Gy, and 56.59 Gy in the free-hand plan, respectively.
Advantages of free-hand technique
Patient’s comfort was one of the major advantages of the free-hand brachytherapy; this procedure was well-tolerated compared with interstitial brachytherapy. This is probably due to the fact that the free-hand technique involves insertion of needles through vaginal fornices, whereas in interstitial brachytherapy, needles are inserted transperineally using a template, causing significant discomfort in ISBT patients. Therefore, regarding patient’s comfort, the free-hand technique is better than interstitial brachytherapy in suitably selected patients. Patients tolerated this procedure well with combined spinal-epidural anesthesia, with top-up at regular intervals.
Applicator removal
Free-hand needles were removed following the removal of ovoids and central tandem, so that we could assess and appropriately manage any possible bleeding occurring due to the removal of needles. As compared with template-based interstitial brachytherapy associated with a significant amount of bleeding on removal of the applicators, especially from the needle entry points over the perineal skin, minimal or no bleeding were noticed on removal of needles in the free-hand brachytherapy technique, as the needles were inserted through the fornices and not through the perineum. In our study, in a very few patients, the bleeding points were easily managed with application of appropriate pressure using a gauze pad.
Another notable advantage is that the free-hand brachytherapy technique can be used in clinical setting where multiple applications are practiced, as in Yoshio et al. [17] and Liu et al. [18]studies, instead of treating all fractions in a single-application setting. Added advantages in an outpatient setting include lower risk of hospital-acquired infection, lower financial cost to patient, and better workflow protocol within the department [26].
In this study, we observed that there was a better CTVHR coverage and OARs doses equivalent to that of intra-cavitary brachytherapy technique, showing a trend towards usage of the free-hand technique in suitable locally advanced carcinoma cervix patients [27].
Lack of image guidance during application is the only limitation of our study. MR imagining was not considered as part of our study.
Conclusions
The free-hand technique (IC + IS) is a relatively simple procedure, and provides a greater degree of freedom for needle insertion resulting in greater patient’s comfort when compared with ISBT and other template-based techniques. The target volume coverage was statistically significant when compared with ICBT, with no difference in OARs doses. It emerges as a reliable and feasible option for patients with more than medial 1/3rd parametrial residual disease following EBRT, but not extending up to lateral pelvic wall. However, a clinical comparison of the same is needed in a future study. Therefore, the free-hand technique (IC + IS) is a reliable and practical alternative that can be employed even in resource-limited settings.