Introduction
Psoriasis is one of the most common immune-mediated inflammatory disorder characterized by chronic course. It affects approximately 2–3% of the world’s population [1]. Psoriasis may be provoked by environmental factors in the patients with genetic predispositions [2]. Psoriasis is phenotypically characterized by thickened, red, scaly plaques and systemic inflammation, it is also associated with multiple comorbidities, such as cardiovascular disease, stroke, hypertension, metabolic diseases, chronic kidney disease and joint destruction. Psoriatic arthritis (PsA) is diagnosed in about one-third of patients with psoriasis [3, 4].
In 1964, PsA was recognised as a separate disease by the American Rheumatism Association (now the American College of Rheumatology), and is included in a group of the seronegative spondyloarthropathies. Generally, PsA is associated with psoriasis, but 10–15% of patients develop arthritis prior to psoriasis, the potential presence of PsA sine psoriasis is also possible. PsA affects people heterogeneously with a range of clinical manifestations, like inflammatory arthritis, dactylitis, enthesitis, spondylitis, skin psoriasis and nail disease. The disease has a significant impact on patients’ physical function, social participation, and quality of life [5, 6].
The severity of psoriasis vulgaris (PV) is graded into mild and moderate to severe disease. Quantitative scoring of skin severity includes calculation of the Psoriasis Area and Severity Index (PASI), body surface area (BSA) as well as the Dermatology Life Quality Index (DLQI). Mild disease is defined as body surface area (BSA) ≤ 10%, psoriasis area and severity index (PASI) ≤ 10 points and dermatology life quality index (DLQI) ≤ 10 points, moderate to severe psoriasis as BSA > 10% and/or PASI > 10 points and DLQI > 10 points [6, 7]. Patients with psoriatic arthritis meet the Classification Criteria for Psoriatic Arthritis (CASPAR). Active disease is defined as ≥ 3 tender and ≥ 3 swollen joints, moreover patients complete 5-point Likert scale (score 1: not at all severe; 2: mild; 3: moderate; 4: severe; 5: very severe). The assessment of psoriasis disease activity and its effect on patients’ quality of life are used to assess the severity of patients’ disease and their response to treatment [8, 9].
Psoriasis is pathogenically driven by proinflammatory cytokines and mediated by T cells and dendritic cells. Inflammatory myeloid dendritic cells release interleukin (IL) 23 and IL-12 to activate IL-17-producing T cells, Th1 cells, and Th22 cells to produce psoriatic cytokines like, IL-17, interferon (IFN) γ, TNF, and IL-22. These cytokines mediate effects on keratinocytes. Under the regulation of IL-23, T cells produce high levels of IL-17, which is the major effector cytokine in the pathogenesis of psoriatic disease, along with the IL-17 cytokine family (IL-17A, IL-17F, and IL-17 receptor A). That creates a self-amplifying, inflammatory response in keratinocytes, which drives the development of thickened skin lesions infiltrated with inflammatory cell populations. Major sources of IL-17A in patients with psoriatic disease are mast cells, γδ T cells, αβ T cells, and innate lymphoid cells in lesional skin and synovial fluid. Within the skin and joints, IL-17A acts on cellular targets, including keratinocytes, neutrophils, endothelial cells, fibroblasts, osteoclasts, chondrocytes, and osteoblasts, to stimulate production of various antimicrobial peptides, chemokines, and proinflammatory and proliferative cytokines, which promote tissue inflammation and bone remodelling. The importance of the IL-23/IL-17A axis in the pathogenesis of psoriatic disease resulted in development of many new biologic treatments targeting these cytokines. Clinical studies with antibodies against IL-17 have proven the importance of this cytokine in the pathogenesis of psoriasis and their high therapeutic efficacy in the patients with moderate and severe psoriasis and psoriatic arthritis [10–13].
Secukinumab is a recombinant human monoclonal antibody that specifically binds to a proinflammatory cytokine released by T-helper-17 (Th17) cells, IL-17A. It blocks its binding with IL-17R and expression of cytokines. This blockade normalizes the inflammatory processes and combats epidermal hyperproliferation, T-cell infiltration, and excessive expression of pathogenic genes [14].
In January 2015, US FDA and European Commission approved secukinumab for the treatment of moderate-to-severe psoriasis, psoriatic arthritis and ankylosing spondylitis [15, 16]. According to many clinical trials, secukinumab has shown significant efficacy in the treatment of moderate-to-severe psoriasis and psoriatic arthritis, demonstrating a rapid onset of action, sustained response, a favourable safety profile, and an improvement of patients’ quality of life [17–20].
Aim
The aim of the study was to analyse the influence of secukinumab on skin lesions, symptoms of arthritis, quality of life as well as to assess its safety during the treatment of patients with psoriasis and psoriatic arthritis.
Material and methods
The study included 38 patients (21 men, 17 women) treated with secukinumab in the Department of Dermatology, Paediatric Dermatology and Oncology, Medical University of Lodz (from March 2019 to April 2020). Twenty-one patients (11 men, 10 women) were diagnosed with moderate-to-severe psoriasis vulgaris, 17 psoriatic arthritis with accompanying psoriatic skin lesions (10 men, 7 women). The median age of patients with PV and PsA was 43.95 y.o. and 43.95 y.o., respectively. Duration of psoriasis vulgaris ranged from 4 years to 46 years, with median 17.9 years; the median psoriatic arthritis’s duration was 11.53 years with range from 4 years to 35 years. Period of treatment with secukinumab ranged from 1 month to 12 months. The median treatment’s duration in the group of patients with PV and PsA was 5.76 months and 4.94 months, respectively (Table 1).
Table 1
Characteristics of psoriatic patients
All patients presented with prior failure to systemic therapies, contraindications, or intolerability to systemic agents (methotrexate, cyclosporine, acitretin, sulfasalazine). Patients with psoriasis vulgaris were previously treated with methotrexate (MTX), cyclosporine and/or acitretin. In the group of patients with psoriatic arthritis, MTX and sulfasalazine were most commonly used (Table 1). In all psoriatic patients, PASI, BSA and DLQI were calculated before therapy. Patients with active psoriatic arthritis met the Classification Criteria for Psoriatic Arthritis (CASPAR), and they marked on Likert scale as 4–5. Our patients were screened according to secukinumab baseline monitoring guidance and had no contraindications for the use of biologics. Patients were treated with secukinumab, which is formulated as lyophilized powder of 150 mg in a prefilled syringe. Patients were treated according to recommended dosage of secukinumab in psoriasis vulgaris – 300 mg subcutaneous injection (at sites such as upper arm, thigh and abdomen) at weeks 0, 1, 2, 3, 4, and continued treatment with injections every 4 weeks. In psoriatic arthritis with accompanying psoriatic skin lesions they were treated with 300 mg given subcutaneously at weeks 0, 1, 2, 3, and 4, followed by a dose of 300 mg every 4 weeks. Our analyses included all patients who received ≥ 1 dose of secukinumab. We assessed the response to secukinumab treatment by assessment of PASI, BSA and DLQI after 1 month, in the third month of therapy and subsequently every 3 months in patients with psoriasis vulgaris. In the patients with psoriatic arthritis, 5-point Likert scale was assessed by the patients and we assessed the number of tender and swollen joints every 6 months. In both groups we analysed complete blood count and hemogram, liver function tests and renal function tests, repeated 1 month after the first injection, in the third month of therapy and subsequently every 3 months. Safety was evaluated by monitoring adverse events, including the severity of the event and the relationship of the event to the study drug, and by obtaining clinical laboratory measurements, assessing vital signs, and performing physical examinations at each visit.
Statistical analysis
Statistical analysis was performed using Statistica software. The obtained results were analysed statistically by the student's t-test, analysis of variance (ANOVA) post hoc (Scheffe’s test) comparisons and χ2 test with Yates correction if needed. P-values less than 0.05 were considered as statistically significant.
Results
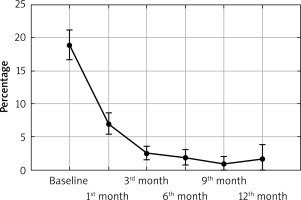
The performed study showed that there was a statistically significant decrease in PASI (from 17.86 points to 0.72 point), BSA (from 18.89% to 0.88%) as well as the DLQI (from 19.32 points to 0.44 point) in all PV and PsA patients during secukinumab treatment (p < 0.0001; Figures 1–3). In patients with PV we observed a statistically significant decrease in PASI (from 21.46 points to 0.84 point), BSA (from 22.38% to 0.8% ) and DLQI (from 20.57 points to 0.33 point) (p < 0.0001; Table 2). In patients with PsA there was a statistically significant decrease in PASI (from 13.41 points to 0.0 point), BSA (from 14.59% to 1.0%) and DLQI (from 17.76 points to 0.67 point) (p < 0.0001; Table 3). 57.89% of all patients with PV and PsA achieved completely normalized DLQI (0–1 point), 66.67% and 47.06% respectively of patients. 76.32% of all patients with PV and PsA reached PASI75, 68.42% PASI90 and 47.37% PASI100. In patients with PV 90.48% achieved PASI75, 76.19% PASI90 and 52.38% PASI100. In PsA patients, 58.82% reached PASI75, 52.94% PASI90 and 41.18% PASI100. In both groups there were no statistically significant differences in PASI, BSA, DLQI between women and men. We found no statistically significant changes in any laboratory parameters during the secukinumab treatment (Tables 2, 3). The effectiveness of secukinumab therapy was similar in our patients, in both groups, demonstrating a rapid onset of action and sustained response (Figures 1–3). Generally, we observed resolution of skin psoriatic lesions, improvement in arthritis and significant improvement in the quality of life in our patients. Furthermore, we observed reduction in the number of tender and swollen joints in our patients after 6 months of therapy. The adverse effects recorded by our patients included gastrointestinal disturbances (1), urticaria (1) and urinary tract infection (1). Side effects were reported in 3 cases, all in patients with psoriasis vulgaris. One episode of acute urticaria, one case of abdominal pain accompanied by increased liver transaminases and one patient with recurrent urinary tract infections were also noted.
Figure 1
Reduction in Psoriasis Area and Severity Index (PASI) in psoriatic patients during secukinumab treatment
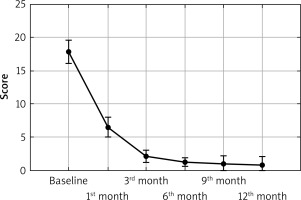
Figure 3
Reduction in Dermatology Life Quality Index (DLQI) in psoriatic patients during secukinumab treatment
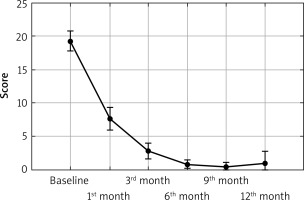
Table 2
Changes in quantitative scoring of skin severity and laboratory parameters in patients with psoriasis vulgaris during secukinumab treatment
Table 3
Changes in quantitative scoring of skin severity and laboratory parameters in patients with psoriatic arthritis during secukinumab treatment
Discussion
Psoriasis is a chronic systemic inflammatory, immune-mediated disease associated with profound impact on patients’ quality of life [21, 22]. That autoimmune disease, involving skin and small joints is driven by proinflammatory cytokines, among which IL-17 is the major effector cytokine [23]. That findings led to the discovery of new antipsoriatic therapies which have been developed to block this key cytokine and its downstream effects. Clinical studies have labelled secukinumab, which is a humanized, monoclonal antibody anti-IL-17A, suitable as therapy for moderate to severe psoriasis, hypertrophic palmoplantaris psoriasis, and generalized pustular psoriasis in adult patients, in cases of prior failure to systemic therapies, contraindications, or intolerability to systemic agents. Also psoriatic arthritis and ankylosing spondylitis not responding to systemic agents or moderate-to-severe disease in adult patients are indications for secukinumab [15, 16, 24–26]. Its clinical efficacy in psoriasis and safety have been well demonstrated in many clinical trials. In correlation with resolution of psoriatic skin changes, and improved signs and symptoms of psoriatic arthritis, secukinumab is also associated with significant improvements in health-related quality of life measures [17–20]. The results of our studies confirm clinical efficacy and safety of secukinumab in treatment of PV and PsA in real life conditions.
In our study secukinumab was associated with a reduction in psoriasis symptoms, like resolution of psoriatic skin lesions, pain and swelling in the joints and tendons, accompanied by reduction in the index used to express the severity of psoriasis, i.e. PASI, BSA. Moreover an improvement in the health-related quality of life on the DLQI and 5-point Likert scale was shown. In our study all patients achieved minimal clinically important difference (MCID) for DLQI.
Generally, secukinumab has a high safety profile; among adverse effects reported in clinical trials the most common were nasopharyngitis, diarrhoea, upper respiratory tract infection, inflammatory bowel disease and exacerbation of Crohn disease. Other incidences like urticaria and anaphylaxis, headache, pruritus, hypertension, arthralgia and back pain, cough, rhinorrhoea, injection site reaction, pyoderma, candidiasis, malignancies, nonmelanoma skin cancer (basal cell carcinoma, squamous cell carcinoma), melanoma, bladder cancer, thyroid cancer, neutropenia, were mentioned as well; moreover secukinumab interferes with the immune system and it enhances the risk of infections [27–29]. In our study, we observed three incidences of adverse events in psoriatic patients. One episode of acute urticaria in a female patient, observed after the first dose of secukinumab, one female patient with recurrent urinary tract infections, after 6 months of secukinumab therapy and one case of abdominal pain accompanied by increased liver transaminases in a male patient, after 9 months of secukinumab therapy. In that case, we suspect that the inhibition of IL-17a initiated an inflammatory cascade that might lead to the development of Crohn's disease. In all cases the secukinumab therapy was discontinued. All adverse events were resolved with treatment interruption. Our patient with abdominal pain accompanied by increased liver transaminases did not develop inflammatory bowel disease. In the patient with acute urticaria we observed a decrease in PASI (from 30 points to 0 point), BSA (from 35% to 0%) and DLQI (from 28 points to 1 point) after one dose of secukinumab. All patients present with long-term remission, experienced stabilization of psoriatic disease, without progression for 4 to 6 months after completion of treatment.
A limitation of our study was the trial population, although it was sufficient for assessing efficacy and safety. Longer time is required to detect rare adverse events. Moreover, our study was a single-centre study. National multicentre studies in the future might add greater value to the assessment of biological treatment strategies for psoriasis. Furthermore, we did not assess the follow-up period in our study. Significant clinical improvement was confirmed in our patients treated with secukinumab. Secukinumab therapy showed high efficacy in the treatment of moderate-to-severe psoriasis and psoriatic arthritis, demonstrating a rapid onset of action, sustained response, a relatively safety profile, and an improvement of patients’ quality of life. Generally, significant clinical improvement and known drug side effects were confirmed in our patients. These observations were made in real-life conditions and in all the analysed aspects proved good efficacy and safety profile of secukinumab.
Conclusions
Although there is no cure for psoriasis and psoriatic arthritis, however various treatment strategies allow sustained control of the diseases. Secukinumab offers a good therapeutic opportunity and may be a preferred treatment option for patients with moderate and severe psoriasis and psoriatic arthritis. Secukinumab is a valuable addition to our current antipsoriatic drugs.