Summary
Interventional treatment of carotid dissection is related, according to available literature, with a complication rate of up to 13%, and the incidence of occlusion in the C2-C5 segment of the carotid artery, after the use of stents dedicated to the treatment of intracranial aneurysms, can reach 10–18% (during 6–12 months of follow-up). In order to reduce the incidence of periprocedural complications, there were used protection systems (distal and proximal) and a new generation of flexible, double-mesh stents, allowing them to be introduced into the C4-C4 segment of the carotid artery or distal part of the vertebral artery. This study shows that the use of protection systems and the new double-mesh stents is a safe method with good early and midterm results (up to 40 months), with the effect of a flow-diverter stent.
Introduction
Carotid dissection is a relatively rare disorder and occurs in 3 individuals out of 100,000 people per year [1–3]. It can be asymptomatic, but in 20% of patients, primarily those younger than 45 years, it results in cerebral events including strokes [4]. Most often dissection affects the internal carotid artery and is asymptomatic or associated with minor neurologic sequelae, such as cervical pain, headache or Horner’s syndrome. Cerebral ischemic events are less common. In most cases the clinical course of carotid dissection is benign and symptoms resolve after pharmacological treatment. There is, however, a group of patients presenting with the signs of cerebral ischemia, which is usually due to embolization or significant stenosis of the dissected artery. These patients, regardless of the cause of dissection (associated with atherosclerosis, post-traumatic or iatrogenic), constitute a large therapeutic challenge, especially if the dissection is localized in the cavernous (C4) or more distal segments of the internal carotid artery. Prior to introduction of endovascular management of such lesions, a full neurological recovery was only seen in a small percentage of patients [5]. Currently endovascular angioplasty and stenting is becoming a preferred method of treatments of carotid dissections [1–4, 6]. In a large meta-analysis published in 2016, endovascular management was found to be more effective than open surgical repair, with an acceptable frequency of serious adverse events [7, 8]. We analyzed our experience in the management of carotid and vertebral dissections to assess the effectiveness of stenting with use of new-generation stents and protection systems [9].
Aim
In this retrospective study we analyzed the efficacy and safety of treatment of symptomatic dissections of the internal carotid or vertebral arteries that coexisted with hemodynamically significant stenosis or aneurysmatic dilatation of the dissected artery with use of the new-generation double-mesh stents (which can be used as a flow-diverting device excluding aneurysmatic dilatation) with protection systems.
Material and methods
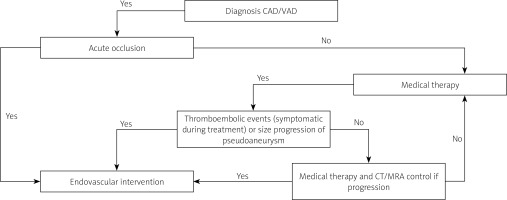
From May 2015 to February 2018 a total of 19 patients (15 men, age range: 25–83, median: 55 years) were scheduled for endovascular treatment according to the algorithm in our hospital (Figure 1) with symptomatic dissection of the internal carotid or vertebral arteries with coexisting stenosis and/or aneurysmatic dilatation of the artery. The detailed inclusion and exclusion criteria are outlined in Table I.
Table I
Inclusion and exclusion criteria for patients with dissection
Figure 1
Algorithm management of patients with dissection of carotid and vertebral arteries in our hospital
CAD – carotid artery dissection, VAD – vertebral artery dissection.
Spontaneous dissection occurred in 16 patients (including one with vertebral artery occlusion), traumatic disease in 2 patients and 1 in the iatrogenic mechanism.
In the analyzed patients, 12 (63%) patients suffered a stroke (in 2 patients in the course of the dissection there was acute occlusion of the internal carotid artery (ICA), 6 (32%) patients had transient cerebral ischemia and in 3 (16%) there was head or neck pain with Horner syndrome symptoms).
As a preliminary imaging examination, an ultrasound examination was used, then the presence of lesions in all patients was confirmed by angiotomographic (CT) examination. The study was aimed at assessing the aorta and cervical arteries, including segments not available for the ultrasound examination.
The aortic arch was of type I in 12 cases, type II in 7, and type III in 2 patients. Bilateral stenosis of the carotid artery was found in 3 (16%), and occlusion was confirmed in 2 patients. Clinical characteristics of patients are given in Table II.
Table II
Demographic, clinical and diagnostic data, and endovascular interventions (n = 19)
The primary endpoint was the proportion of patients who had new a stroke (different from the preprocedural event or exacerbation of preprocedural stroke) or a stroke-related death. We included all types of strokes, both ipsi- and contralateral, as well as minor, major and fatal strokes. The secondary endpoint was the proportion of patients who had reocclusion or death that was not caused by the stroke. In addition, we assessed technical feasibility of endovascular repair of carotid and vertebral dissections, and also safety and feasibility of stent implantation in the intracranial portion of the internal carotid artery.
Standard preprocedural management of patients comprised multidisciplinary assessment, including neurological, neuroradiological and vascular consultations. Potential risks and benefits associated with the planned procedure were discussed with patients, and all of them gave their written informed consent. Details of the endovascular procedure are described in the next part of this paper. Neurological assessment was performed at least once before the procedure and on postprocedural day 1–2. Follow-ups were performed on the day of the procedure, and then after 1, 3, 6 and every 6 months (on an outpatient basis). Control CT angiographies or arteriography were performed 3 or 6, 12 and 24 months after endovascular repair. In all patients dual antiplatelet therapy was initiated 3–1 days before the day of the procedure. Periprocedurally, patients received unfractionated heparin at a dose of 100 U/kg. Patients were discharged home 3-5 days (except for patients with acute stroke) after the procedure, with the recommendation of dual antiplatelet therapy (aspirin + clopidogrel or ticagrelor) for at least 30 days, optimally for 3-6 months, or, in patients presenting with dissections which were longer than 60 mm, up to 12 months (Table III).
Table III
Location of dissections
[i] Loc. of DIS – location of dissection, ICA – internal carotid artery, VA – vertebral artery, C1 – cervical segment of ICA, C2 – petrous segment of ICA, C3 – lacerum segment of ICA, C5 – clinoid segment of ICA, V1 – preforaminal segment of vertebral artery, V3 – suboccipital part of vertebral artery, DIS – dissection, PA – pseudoaneurysm, DAPT – dual antiplatelet therapy. (A) – acute occlusion with neurologic symptoms, device – protection system, type of stents (S – SpiderFX Embolic Protection Device, E – Emboshield NAV6 Embolic Protection System, M – Mo.Ma 8F, C – Cello, P – Precise stent, CW – Carotid Wallstent stent, RS – RoadSaver stent, LB – Leo-Baby), A – acetylsalicylic acid, C – clopidogrel, T – ticagrelor, type of control (U – ultrasound, C – CT angio, D – angiography).
Endovascular techniques
The femoral artery was the preferred access site and it was used in 17 (89%) patients, while radial access was used in 2 patients. Stents and protection systems were tailored according to the specific patient and angioarchitecture of the dissection, particularly to its location, length and coexisting stenotic or aneurysmatic lesions (Table III).
Usually, for the management of carotid dissections, we used the Precise (Cordis, Fremont, CA, USA), the RoadSaver (Terumo, Tokyo, Japan) or the Carotid Wallstent (Boston Scientific, Natick, MA, USA) stents. As a protection system we used either the Mo.Ma Ultra 8F (Medtronic, Minneapolis, MN, USA) proximal device and Cello catheter (Covidien, ev3 Endovascular, Inc., Plymouth, MN, USA), or distal protection filters, such as the SpiderFX Embolic Protection Device (Covidien, ev3 Endovascular, Inc., Plymouth, MN, USA) and the Emboshield NAV6 Embolic Protection System (Abbott Vascular, Abbott Park, IL, USA). In the case of distal lesions or large aneurysms of a cervical portion of the carotid artery we used the following stents: the RoadSaver and the Leo-Baby (Balt Extrusion, France) self-expanding stents. Since a stenosis associated with dissection is simply the result of a false lumen and intimal flap, self-expanding closed-cell stents (RoadSaver or Leo-Baby stents) are usually sufficient to address lesions located in the upper part of the neck. We used protection systems in all patients.
Results
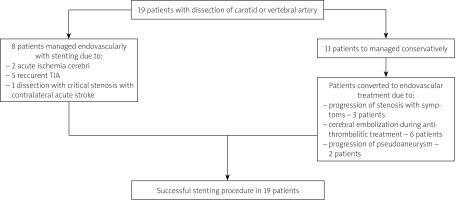
Eighteen patients presented with dissections of the internal carotid artery and 1 patient with a dissected vertebral artery. Length of lesions varied from 22 to 156 mm (mean: 60.1 ±38.7 mm). In 16 patients dissections coexisted with aneurysmatic dilatation of the artery, with maximal diameter of such an aneurysm 3–18 mm (mean: 6.6 ±2.6 mm). Details are presented in Table III. Out of these 19 patients, in 8 (42%) patients, considering morphology of the lesion and overall clinical picture, we performed endovascular interventions without an attempt to treat them conservatively (this included 2 patients in whom we performed urgent endovascular procedures due to acute occlusion of the internal carotid artery, other patients were managed as quick as possible, usually within 7–30 days from the first symptoms). The remaining 11 (58%) patients were initially managed conservatively and the decision to address the dissection endovascularly resulted from clinical worsening due to: recurrent cerebral embolism in 6 patients, progression of stenosis in 3 patients and progression of pseudoaneurysm in 2 of them (Figure 2).
Figure 2
Treatment plan and qualification for interventional treatment of patients with carotid or vertebral arteries dissection
In 8 patients it was possible to repair the dissection using only one stent, in 10 patients we used two stents and in 1 patients three stents (Table III).
In 8 patients, proximal protection was used, in 6 patients Mo.Ma (Medtronic, Minneapolis, MN, USA), in 2 the Cello system (Covidien, ev3 Endovascular, Inc., Plymouth, MN, USA), in 9 patients the SpiderFX distal protection system Embolic Protection Device (Covidien, ev3 Endovascular, Inc., Plymouth, MN, USA), and in 2 the Emboshield NAV6 Embolic Protection System (System (Abbott Vascular, Abbott Park, IL, USA). Out of 19 patients in whom a protection system was used, in 7 of them filters captured embolic debris (in 3 patients a lot of debris).
When the proximal protection system was used, mean duration of the proximal protection was 9.26 ±2.3 min, and all patients well tolerated the protection. In 15 patients presenting with pseudoaneurysms, a total of 19 double-mesh RoadSaver stents were implanted as flow-diverting devices (Table III), in order to cover the entire dissection and exclude blood flow from aneurysmatic lesions.
There were no technical failures or adverse events associated with endovascular procedures. Also, there were no in-hospital deaths, new neurological events or other serious morbidities during the procedure and postprocedural hospital stay. Patients presenting with neurological deficits prior to intervention improved after endovascular repair and this improvement was maintained at hospital discharge. There were no fatalities during 6–40 months of follow-up.
In the follow-up imaging tests, the correct apposition, complete coverage of the lesions, and full closure of the pseudoaneurysm (effect of the flow-diverter stent) were confirmed.
Discussion
Conservative management of dissected carotid arteries, comprising anticoagulation or antiplatelet therapy, results in quite good clinical outcomes. Although reported recanalization rates with hemodynamically sufficient flow through the affected artery are at the level of 50% and reocclusions are frequent [10, 11], Kremer et al. reported a 0.7% annual rate of recurrent ipsilateral stroke in patients with a permanently occluded dissected carotid artery and 0.3% in patients with a recanalized artery [12]. In the CADISS study that evaluated results of treatment in 250 patients with cervical dissection, there was 2% incidence of recurrent strokes [13]. Multiple dissections and dissection of the carotid artery were associated with poorer prognosis [14, 15].
Yet, a failed medical treatment in selected patients is an indication for endovascular repair of the dissection [16–18]. It is currently assumed that standard indications for endovascular intervention comprise recurrent ischemic events, high-grade stenosis within dissection with significantly limited flow, expanding pseudoaneurysm associated with dissection and occlusion or high-grade stenosis of the contralateral internal carotid artery. Still, endovascular management of cervical dissections can be associated with high rates of serious adverse events. The incidence of these complications in published reports was as high as 3–16% [7, 18, 19]. Adverse events were less frequent in patients with traumatic dissections [19]. Rates of serious adverse events associated with endovascular management of cervical dissection are significantly higher than those in patients undergoing carotid or vertebral artery stenting for atherosclerotic stenosis. Interestingly, although cerebral embolism is the most frequent cause of serious adverse events associated with cervical dissections, protection systems were used rather infrequently during endovascular repair of these lesions. In the study published by Cohen et al. only 13% of the patients were managed under distal protection [20]. Malek et al. [21] did not use protection at all, and in the work of Edgell et al. it was emphasized that the introduction of the protection system may lead to progression of dissection [22]. In our study, the system of protection was used in all patients, and in 42% of the patients the proximal protection system (PSP) was used.
In contrast to the above-cited studies, in our patients endovascular repair of the dissections was uneventful.
Martinelli et al. obtained similarly good results in a study where all patients were treated endovascularly under distal protection [23]. In our work both types of protection were used: proximal and distal. The PSP is the system of choice, protecting cerebral tissue from embolization from the very beginning of the procedure, and was used mainly in the case of long lesions, including 2 and more segments. In other cases, a distal protection was used, mainly the Spider system (Medtronic), which allows for the use of any guidewire. In both groups of patients, no neurological events occured, neither during hospital stay nor during follow-up.
Additionally, in our work, in 15 patients we used a new generation of double-mesh stents. Their uniqueness, in comparison with previously used stents, included low profile and high flexibility, allowing the device to be inserted into segments previously unavailable for other types of stents. Also, such a double mesh stent acted as a flow-diverter stent allowing a thrombotic closure of the aneurysm. Other authors reported the use of other stents in the segments C2-C5 [7, 24]. This translated into a relatively high percentage of reocclusions of these stents, due to their low radial force, and unpredictable effects of geometry changes of these stent that were dedicated to the treatment of lesions in the arteries, which are not subject to shape changes [7, 24]. The used RoadSaver stents, as stents dedicated to the treatment of atherosclerotic lesions, had adequate radial force, and additionally, due to the dense braid mesh, they exhibit the function of a flow-diverter stent, which allows them to be used in lesions with coexisting aneurysm [25]. In our material, all patients had occluded aneurysms and patent stents during follow-up to 40 months.
The results of our study, despite the limitations (small number of patients, retrospective study), are encouraging. During the observation period stents were patent, despite their considerable length, and patients were free from neurological symptoms. In cases when in spite of optimal conservative therapy, neurological symptoms are present, or when there is hypoperfusion of the brain, endovascular treatment may be a reasonable alternative, especially in high-risk patients. The use of a new generation of stents, with the property of flow-diverter stents and protection systems, can minimize the occurrence of adverse events during the procedure, which until now has been the most serious limitation of endovascular procedures. In addition, antiplatelet therapy reduces the risk of peri- and postoperative events, reducing the frequency of anticoagulant therapy and avoiding related complications [23].
Conclusions
Anticoagulant therapy is still the treatment of choice in patients with dissection of cervical arteries, especially in the asymptomatic group. In the cases when anticoagulation is contraindicated or there are recurrent ischemic episodes, despite appropriate medical treatment, endovascular treatment with the use of novel stents, and protection systems (especially proximal), provides good short- and midterm results. Despite small number of patients, our data suggest that endovascular treatment in such cases can be considered as an alternative treatment.








